1. Migraine aura affects approximately 25% of migraine patients and is characterized by neurological symptoms that gradually develop over 5 minutes and last less than 1 hour.
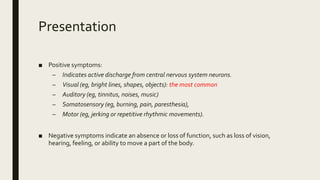
2. Common aura symptoms include visual disturbances like flashing lights, sensory changes like tingling, and speech/language problems.
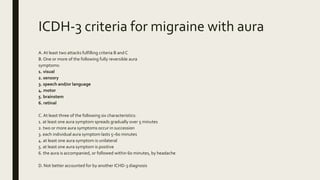
3. The International Classification of Headache Disorders criteria define migraine with aura as having at least two attacks involving reversible aura symptoms followed by headache.