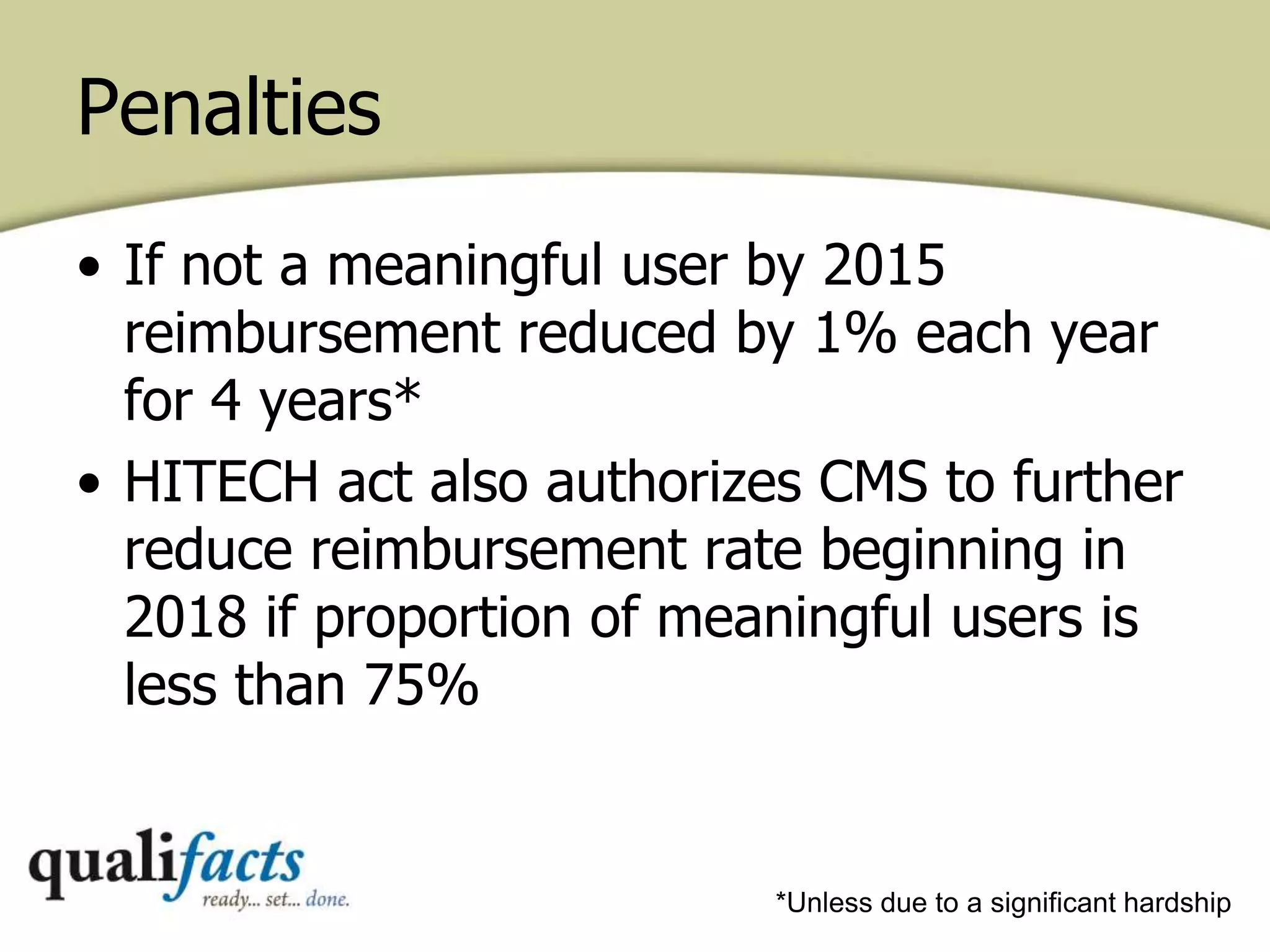
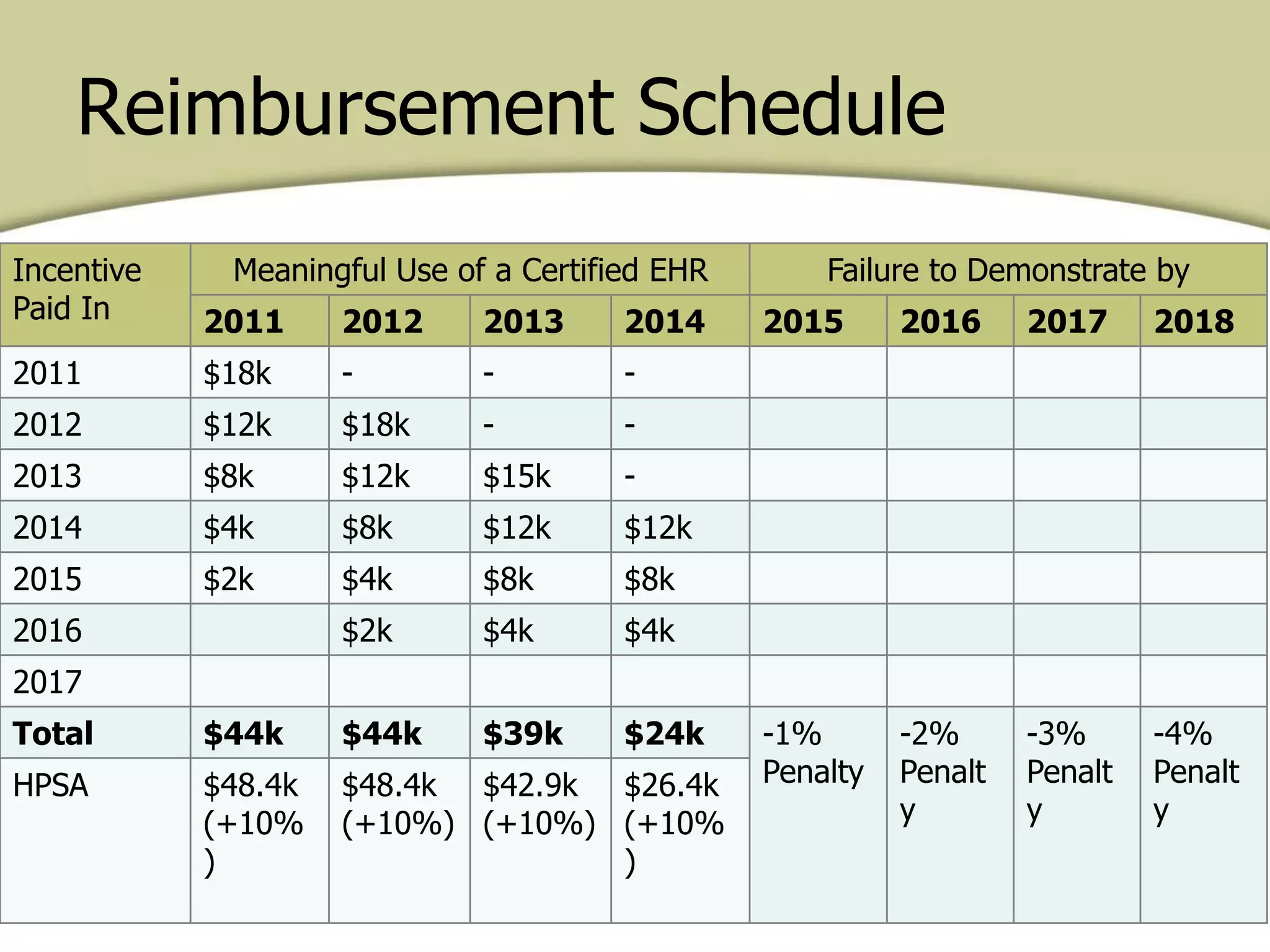
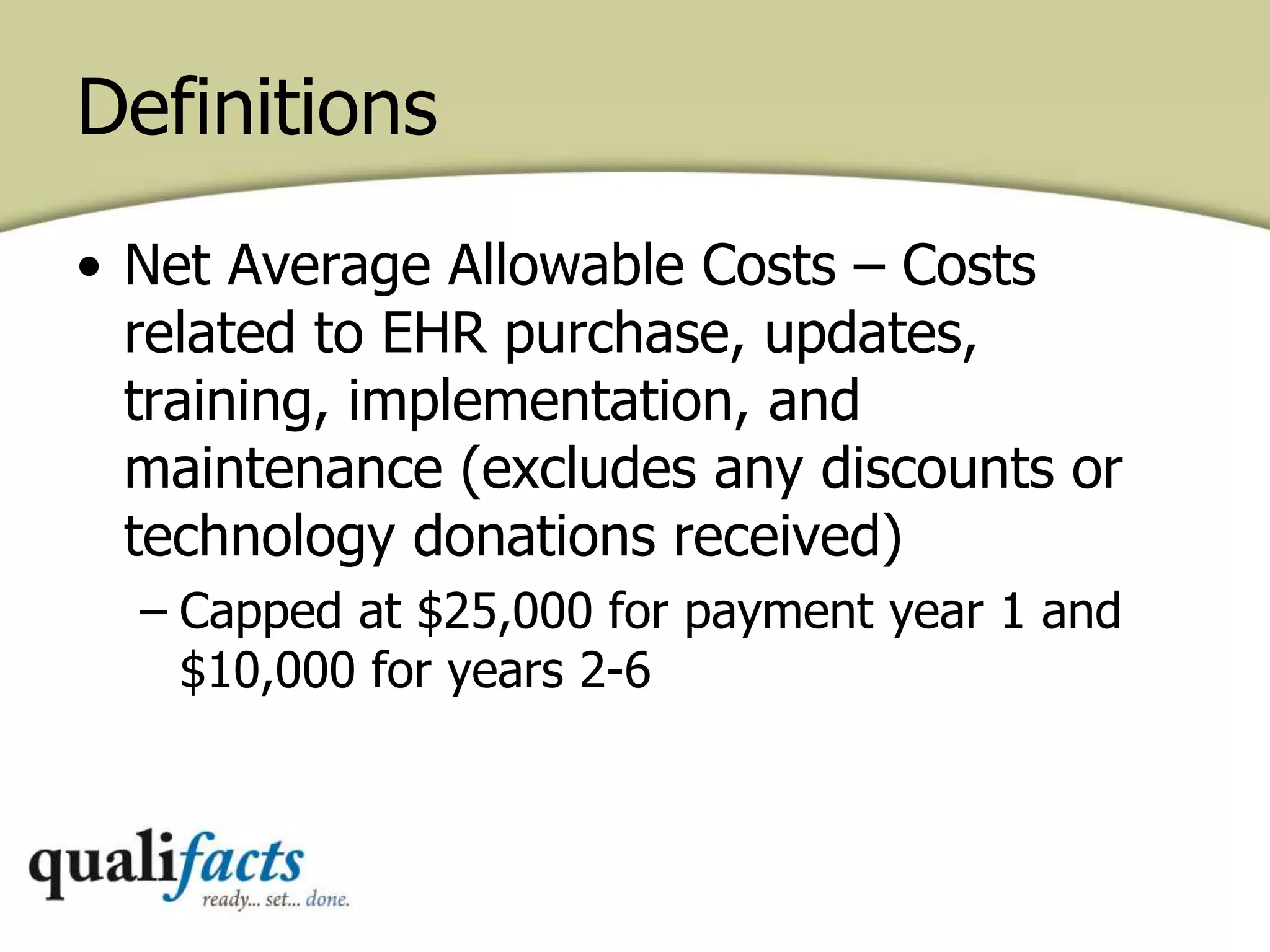
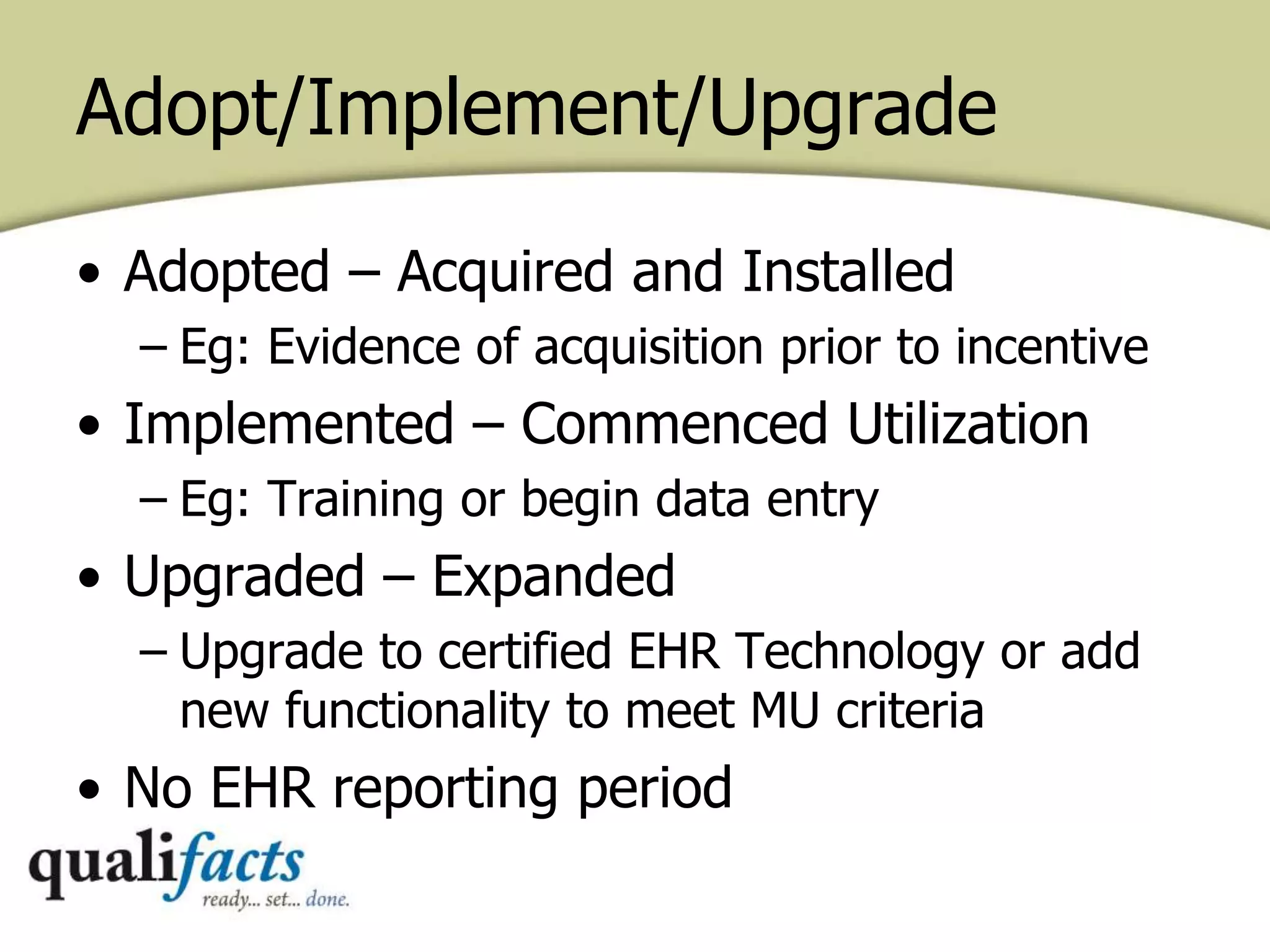
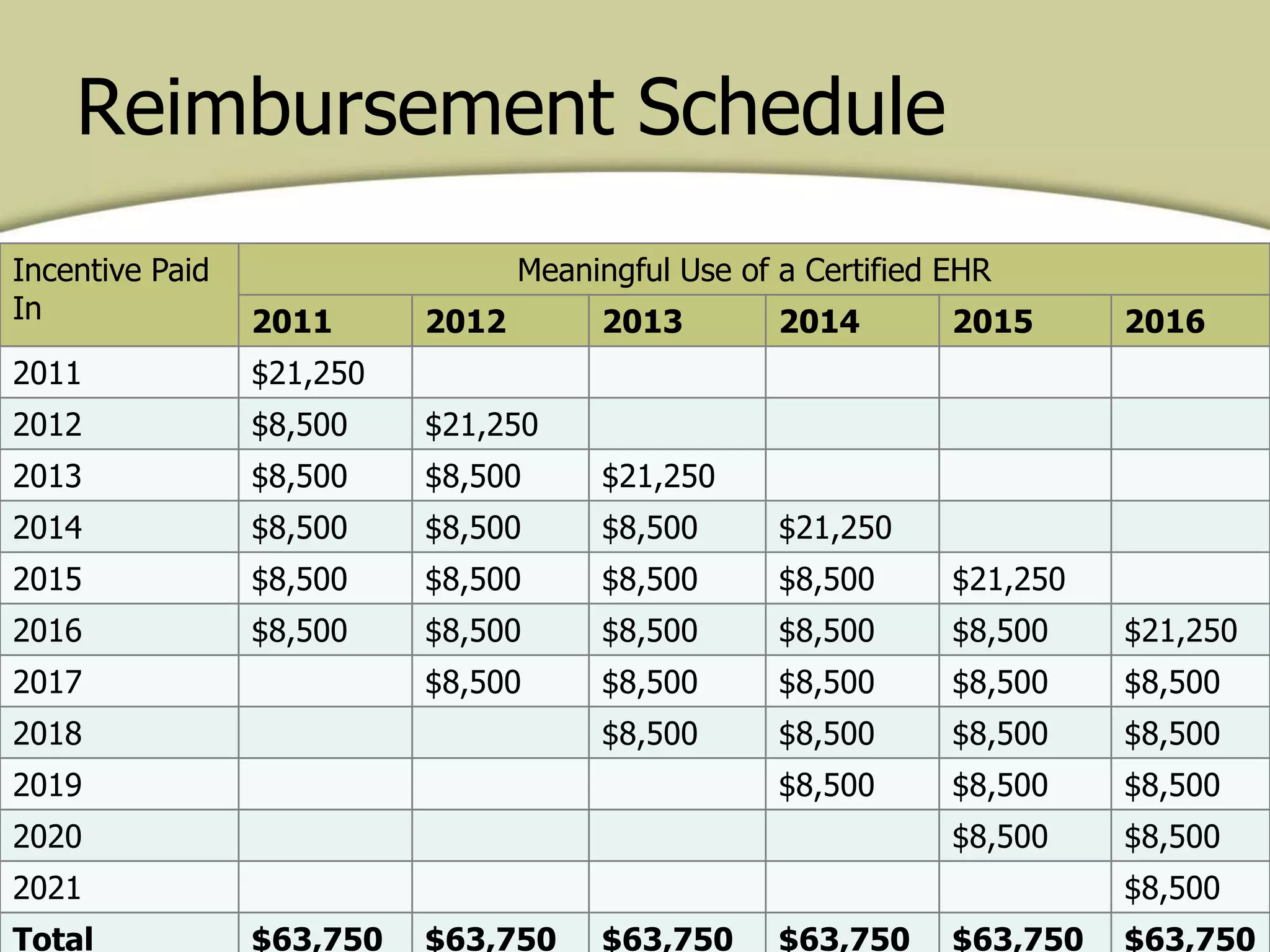
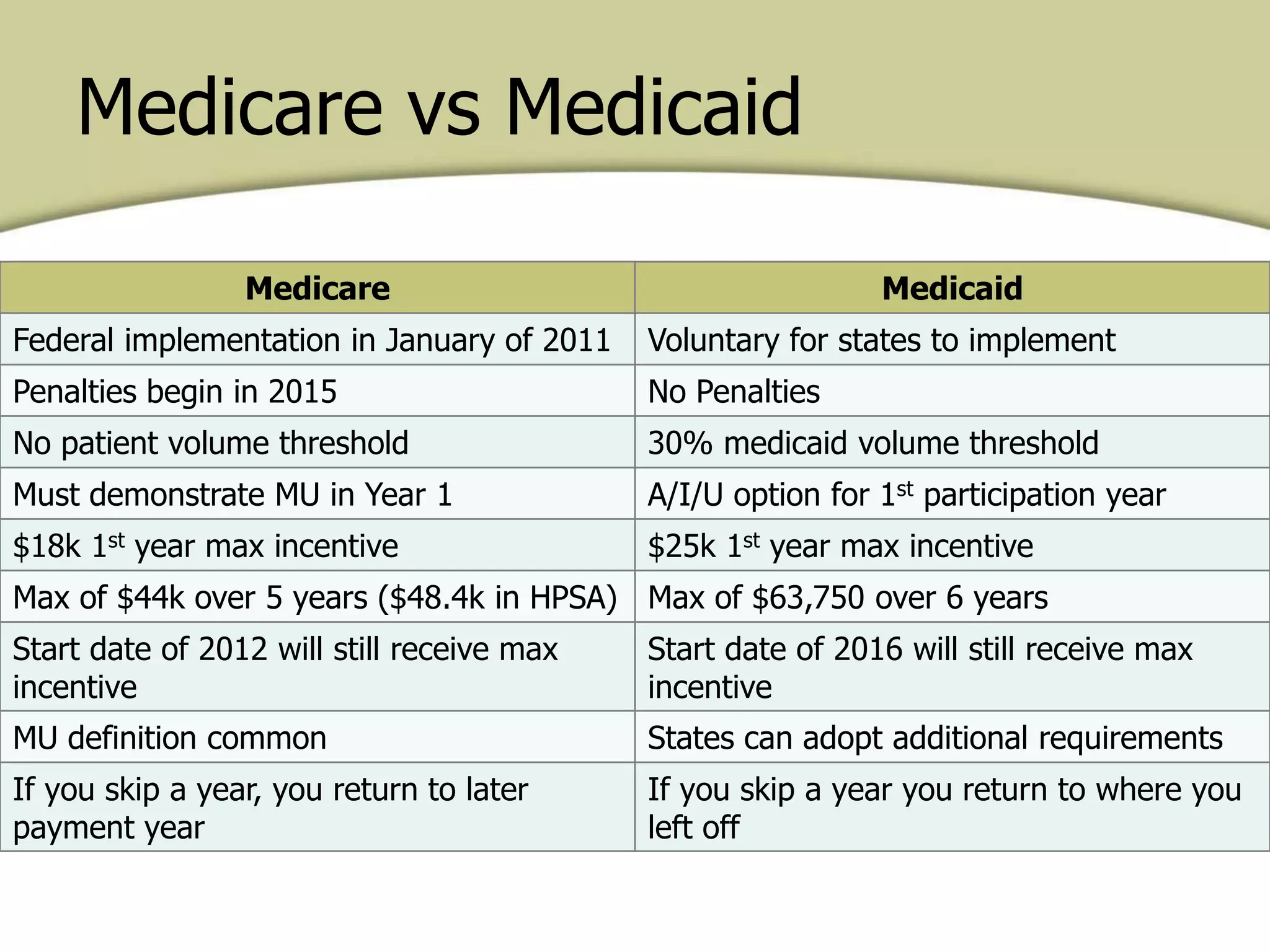
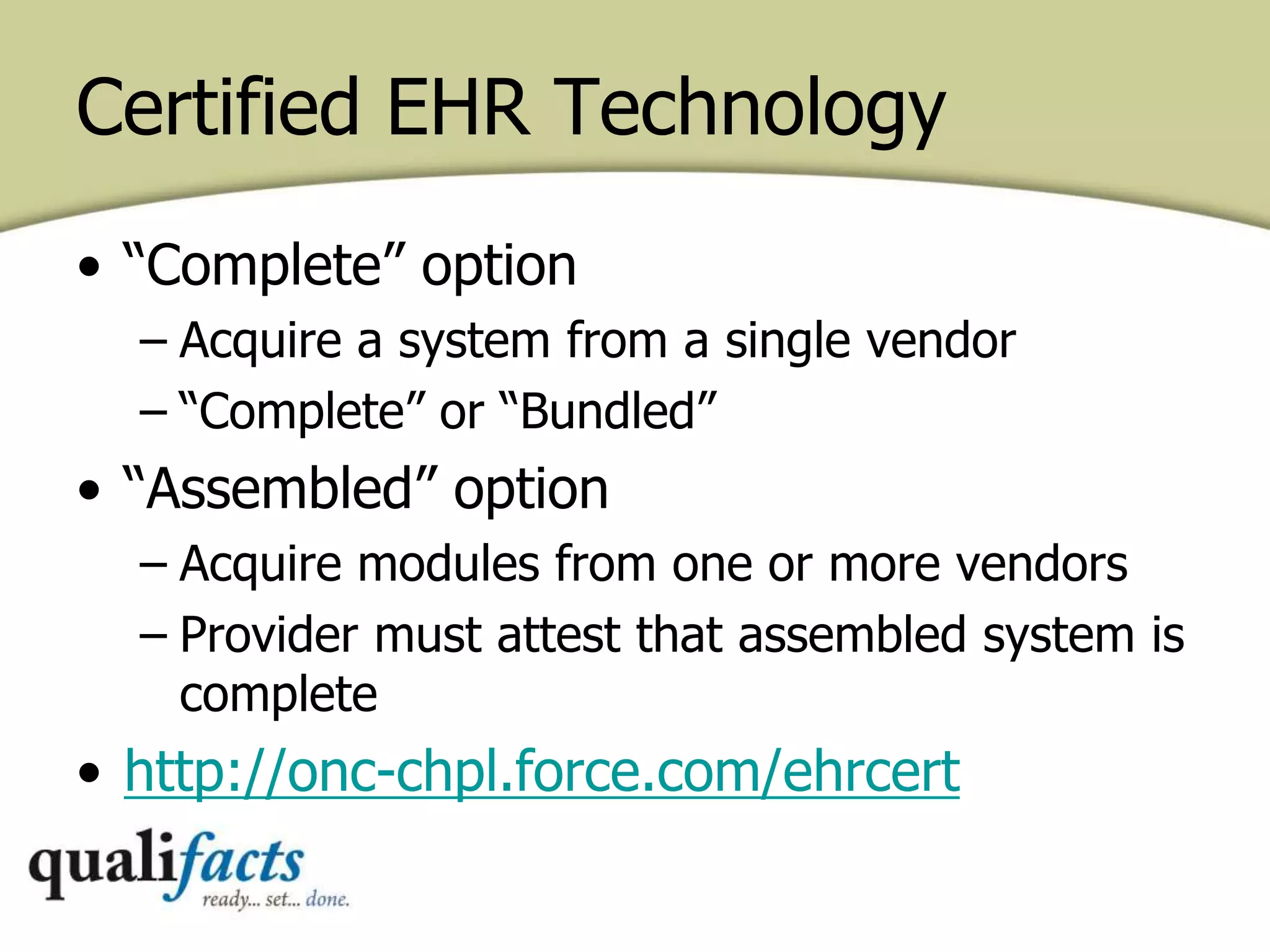
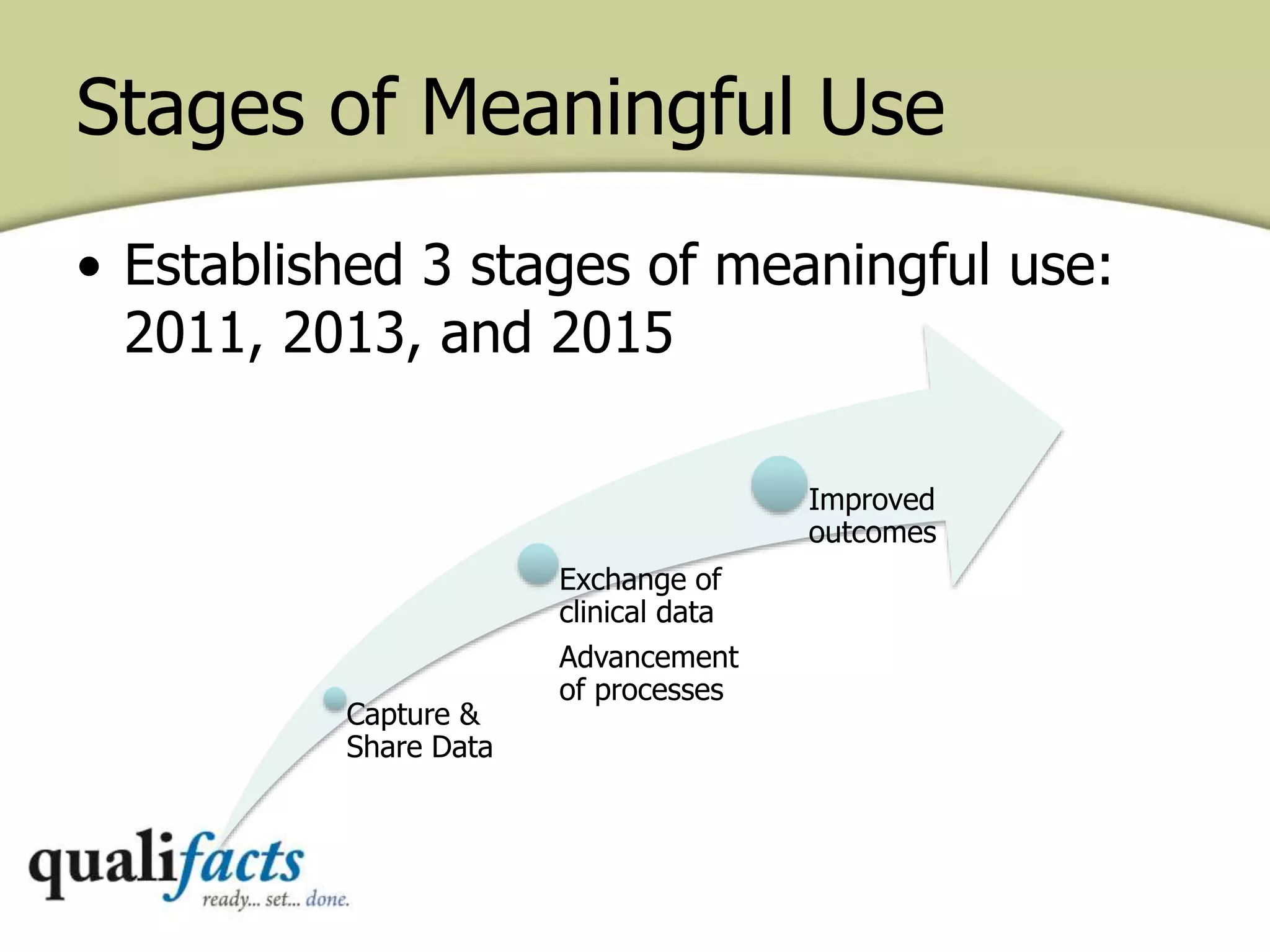
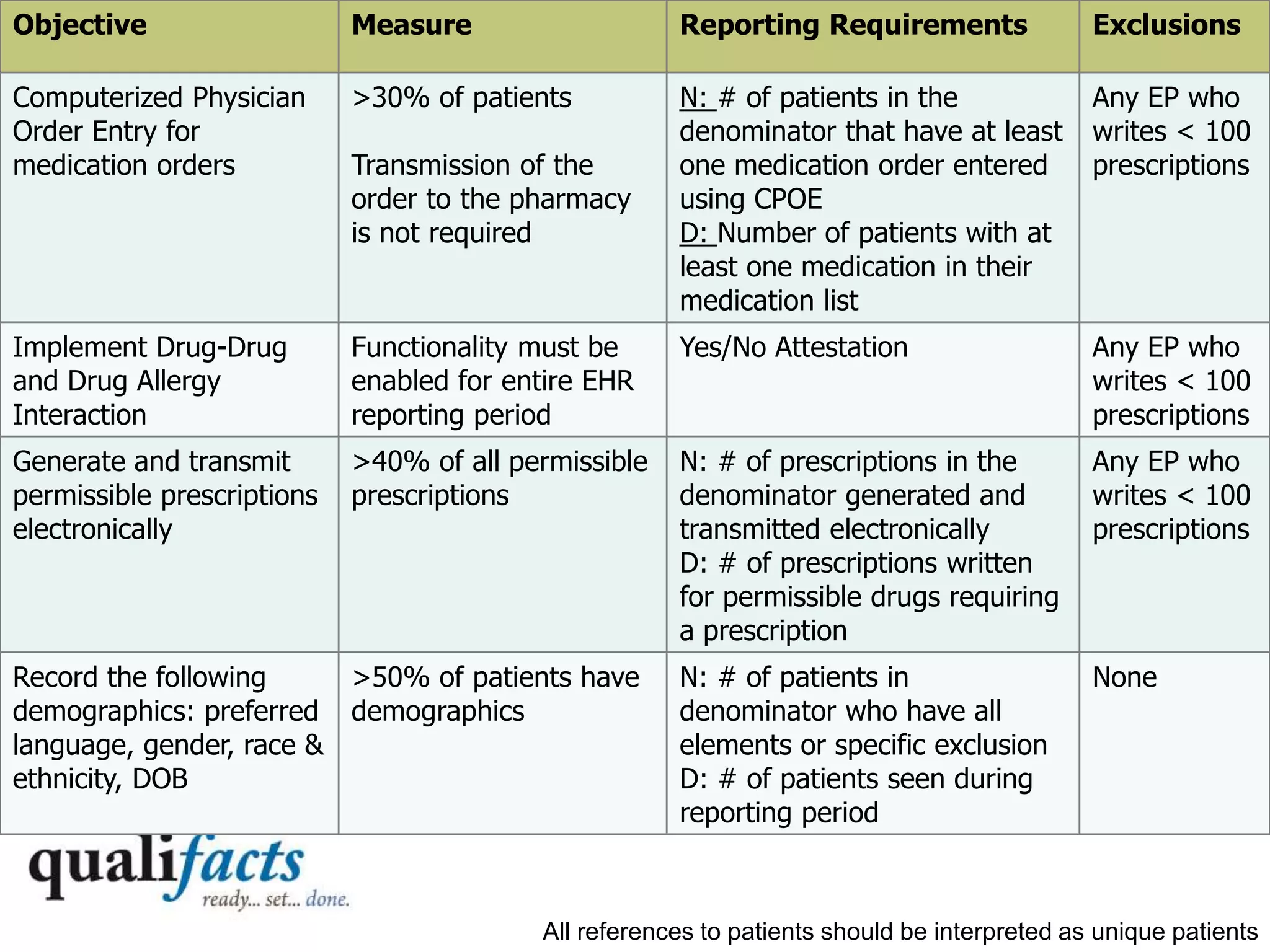
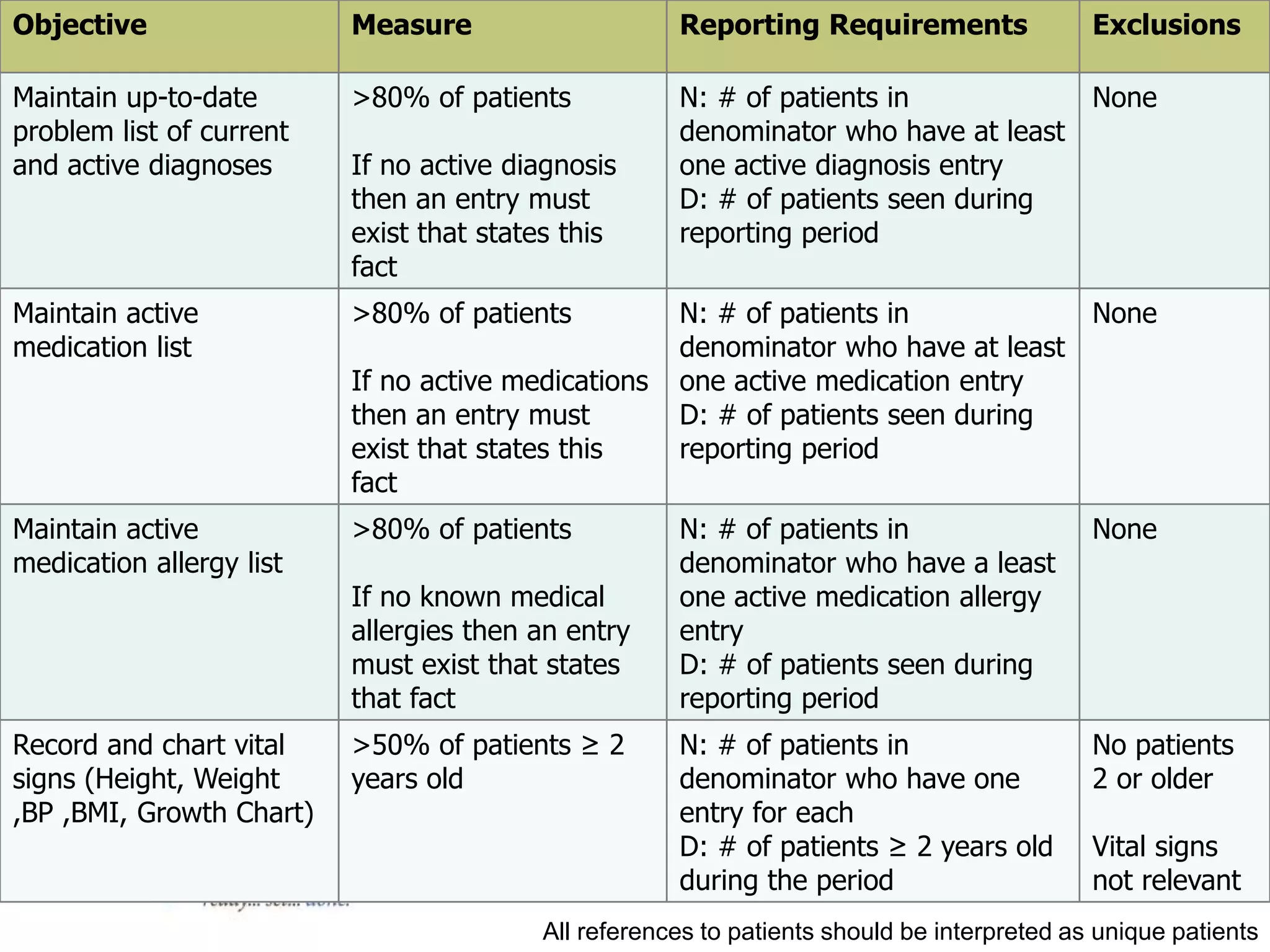
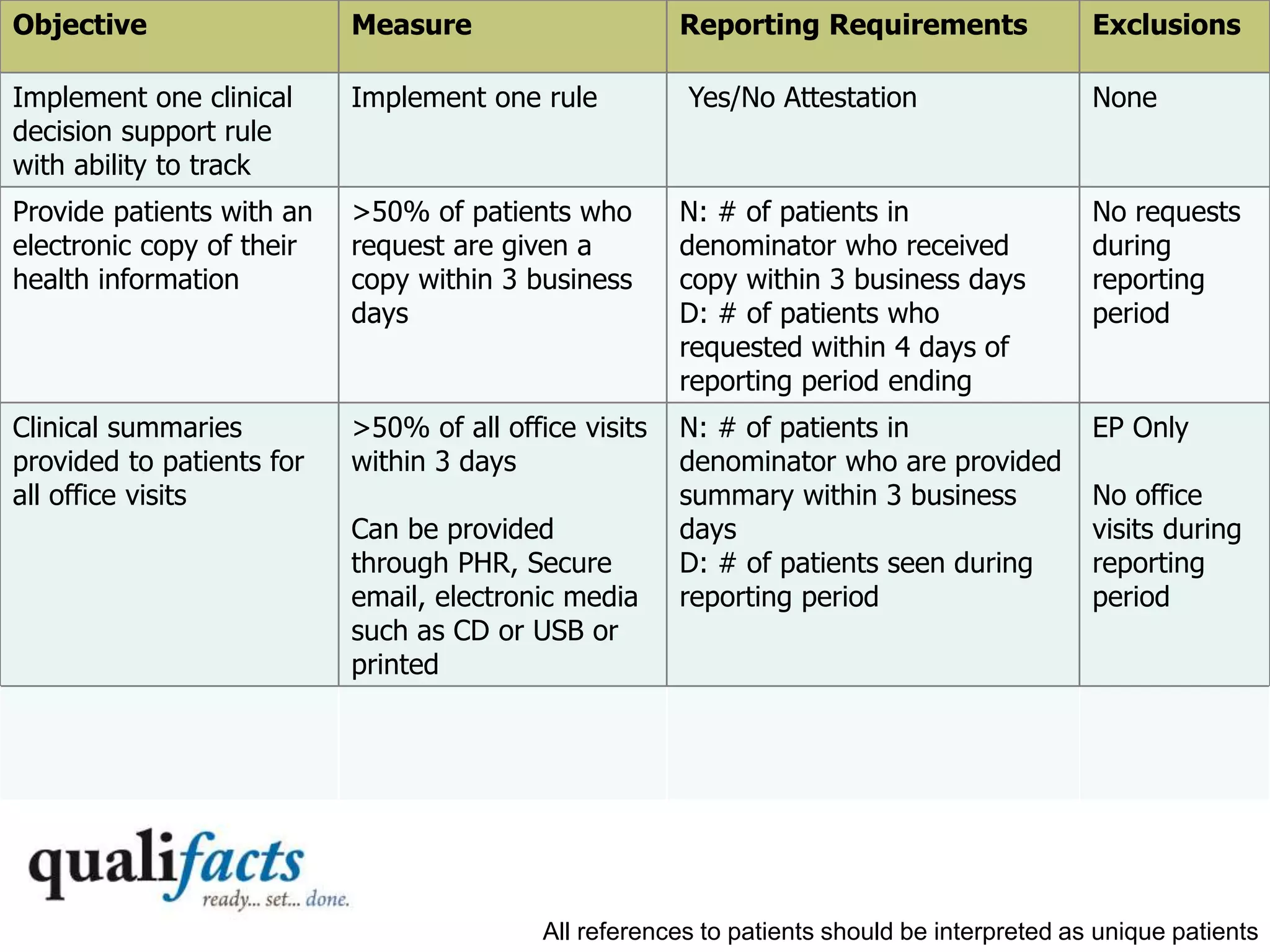
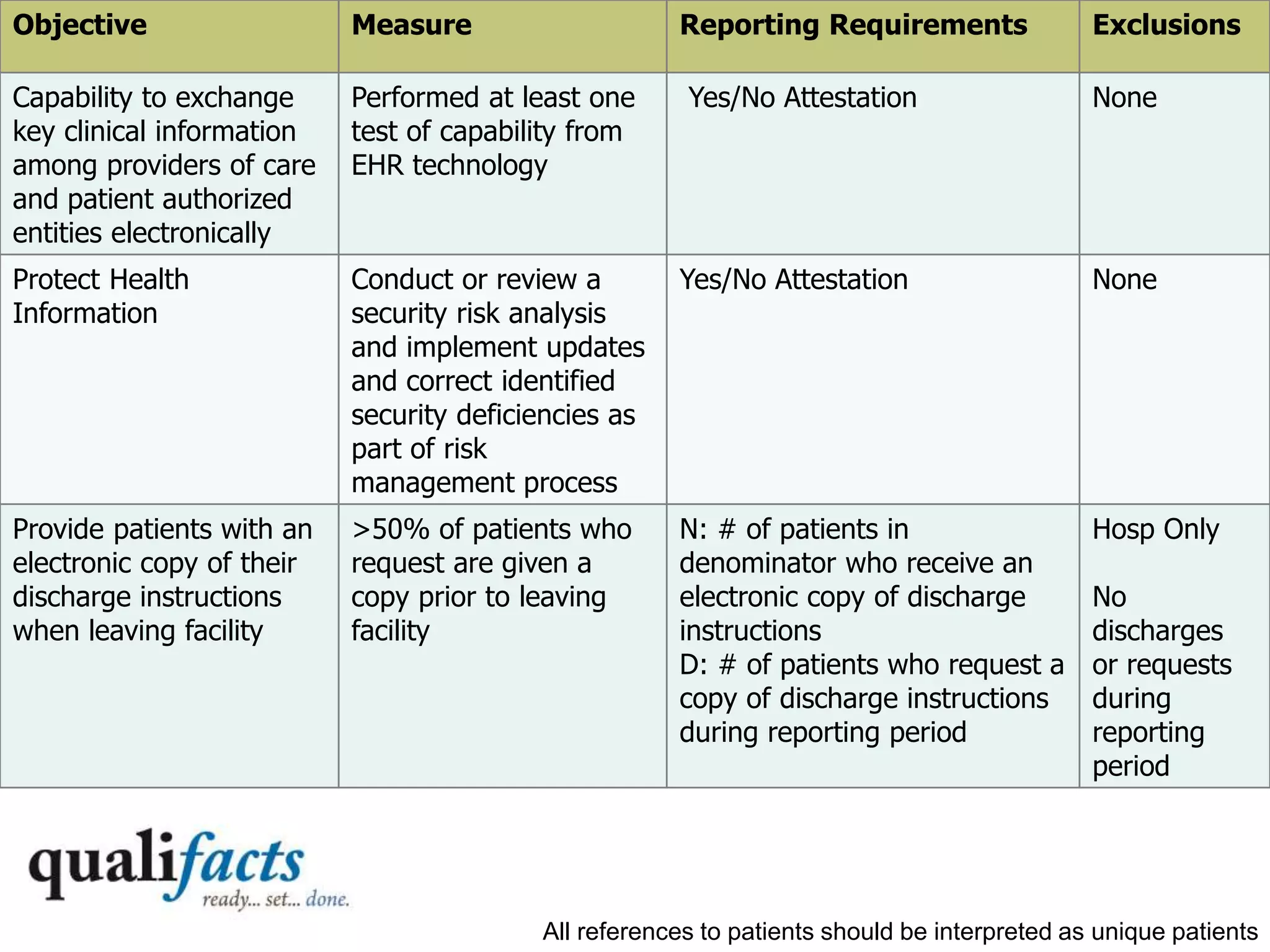
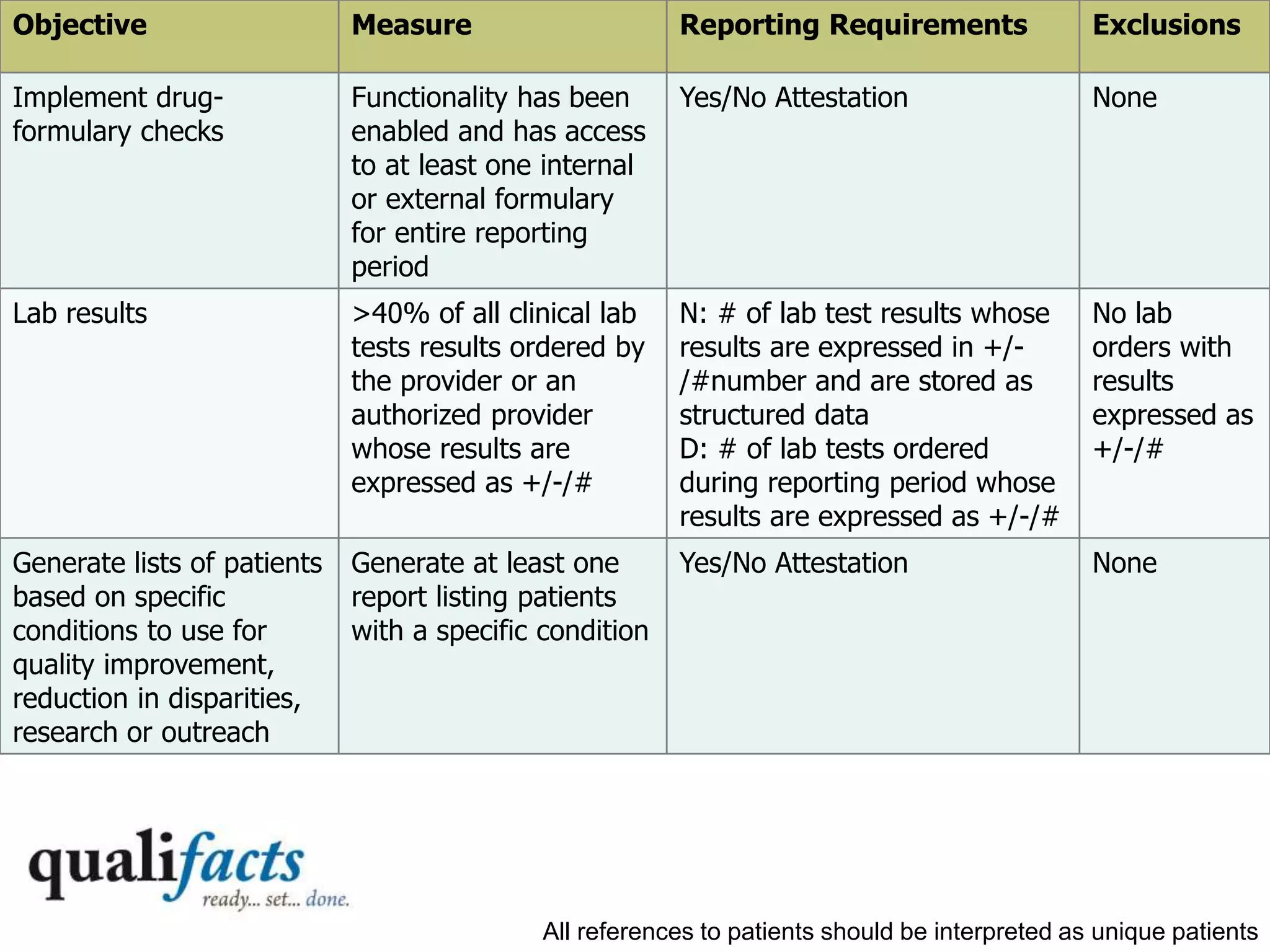
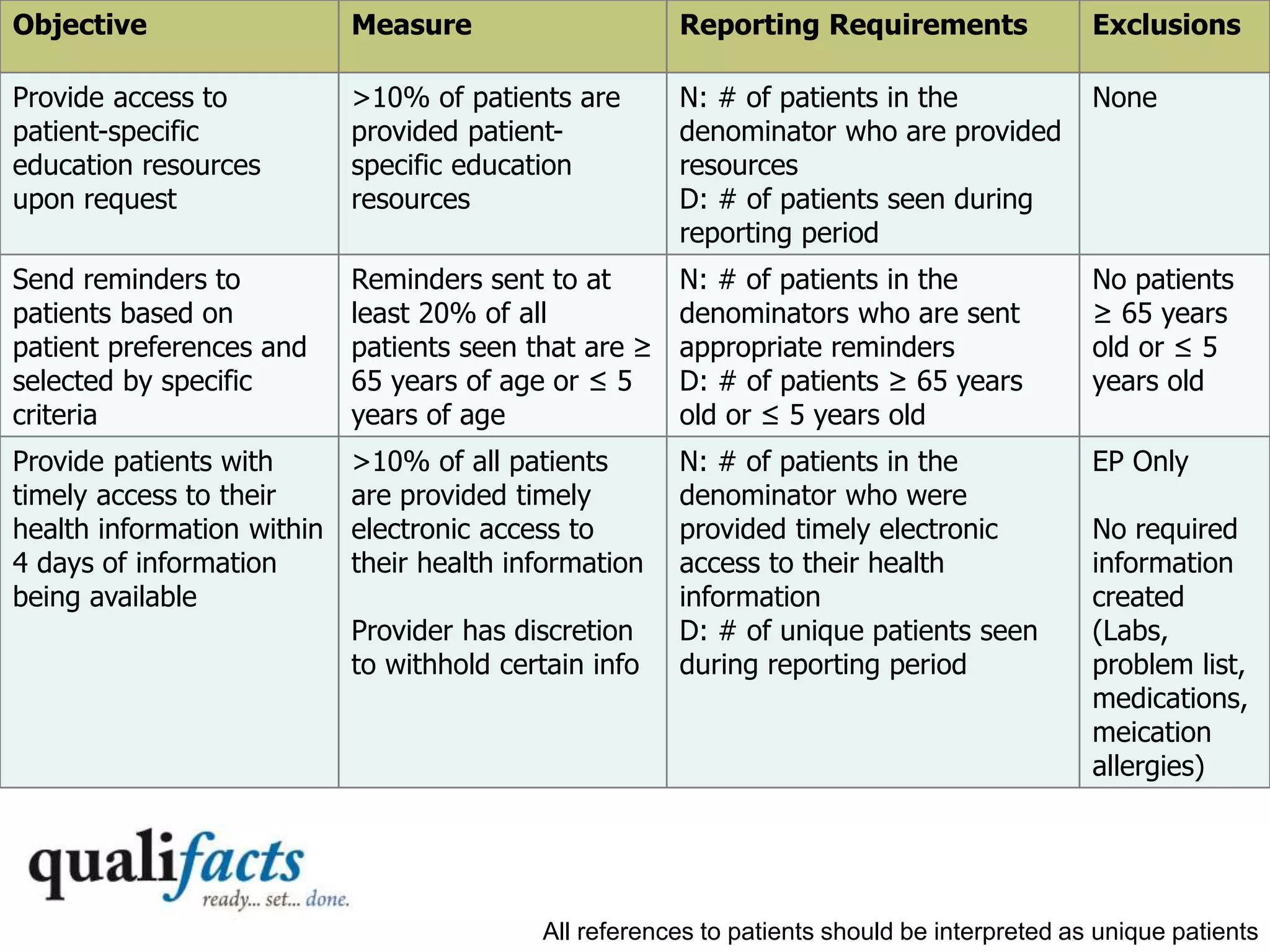
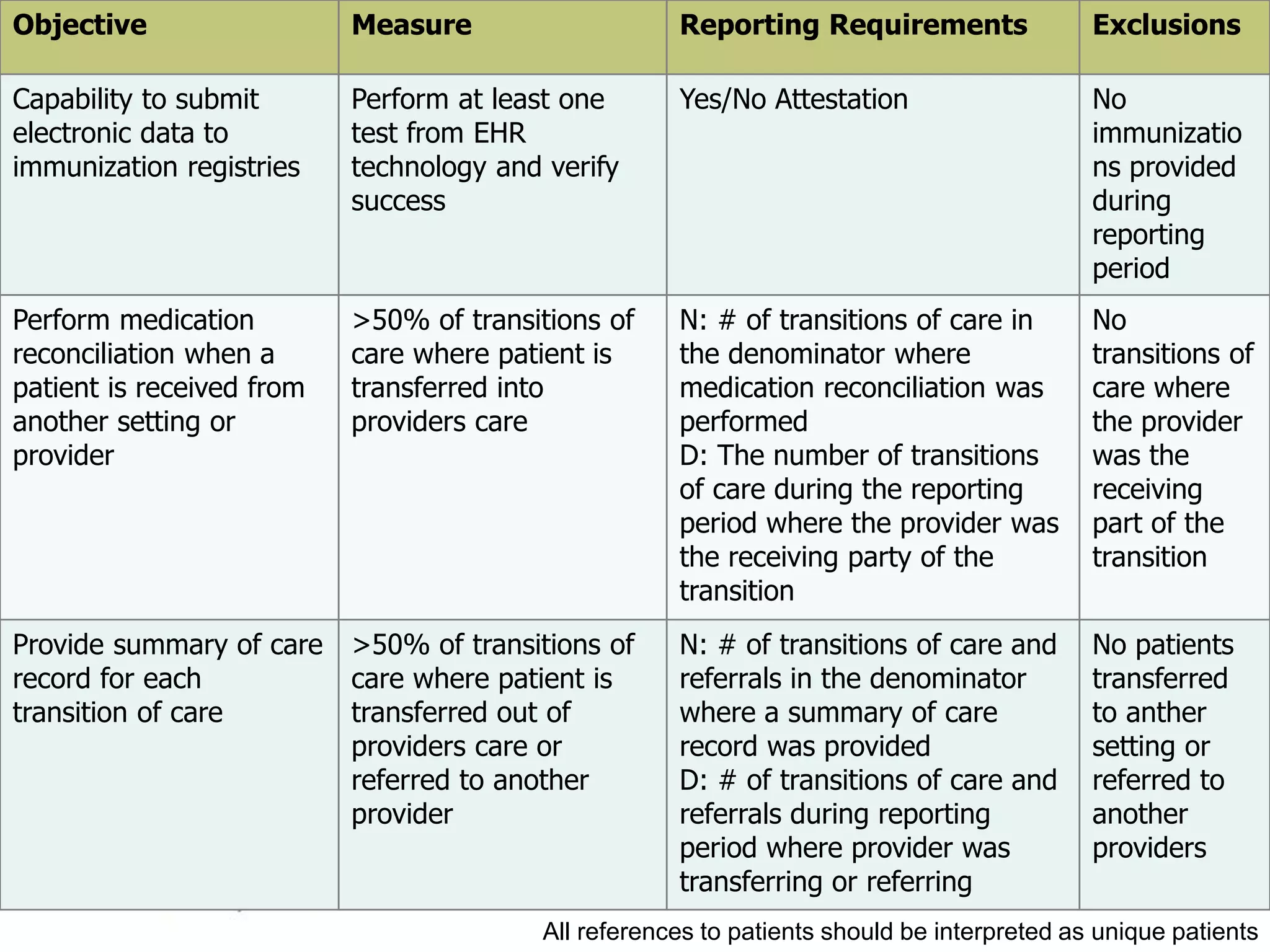
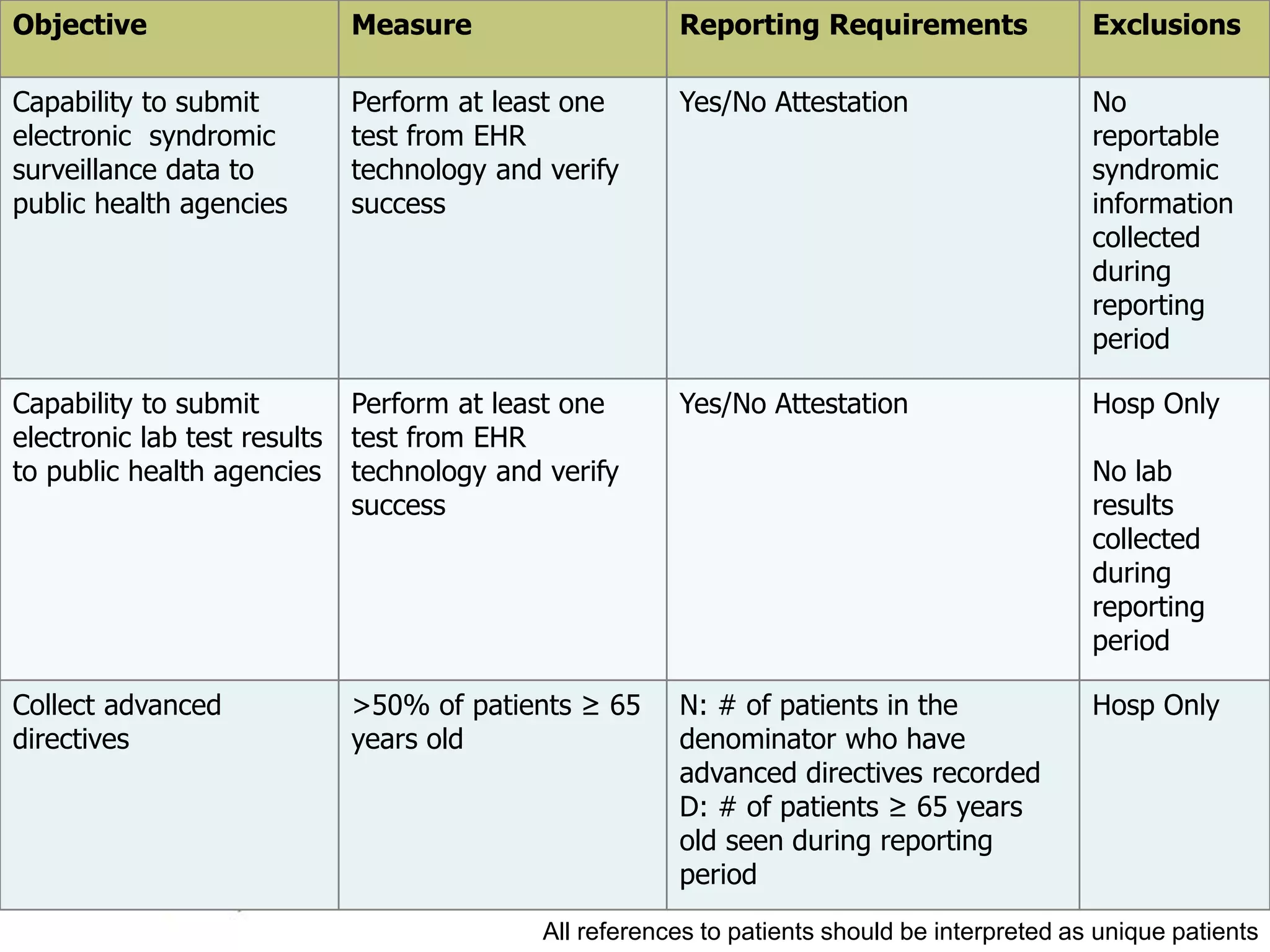
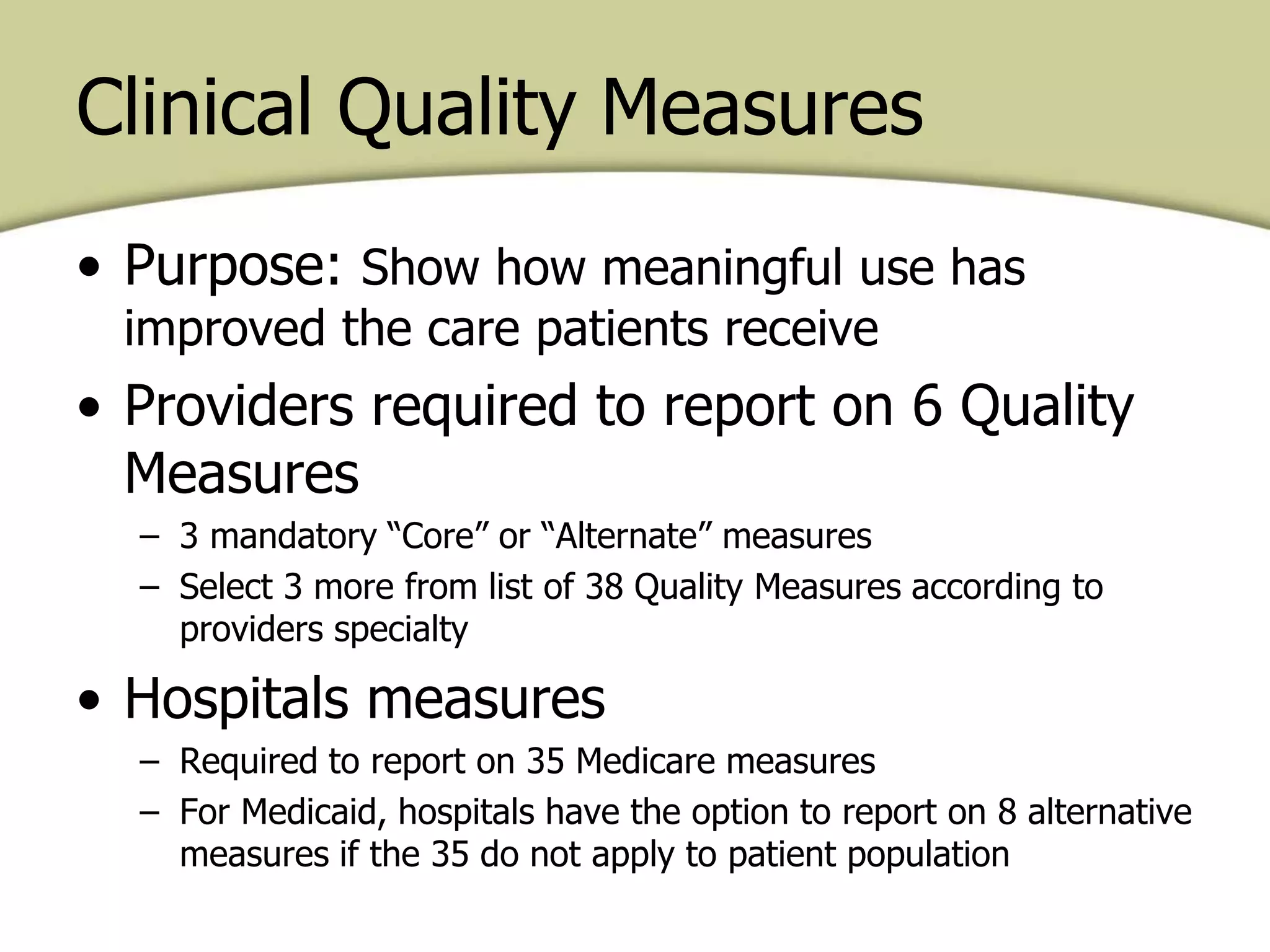
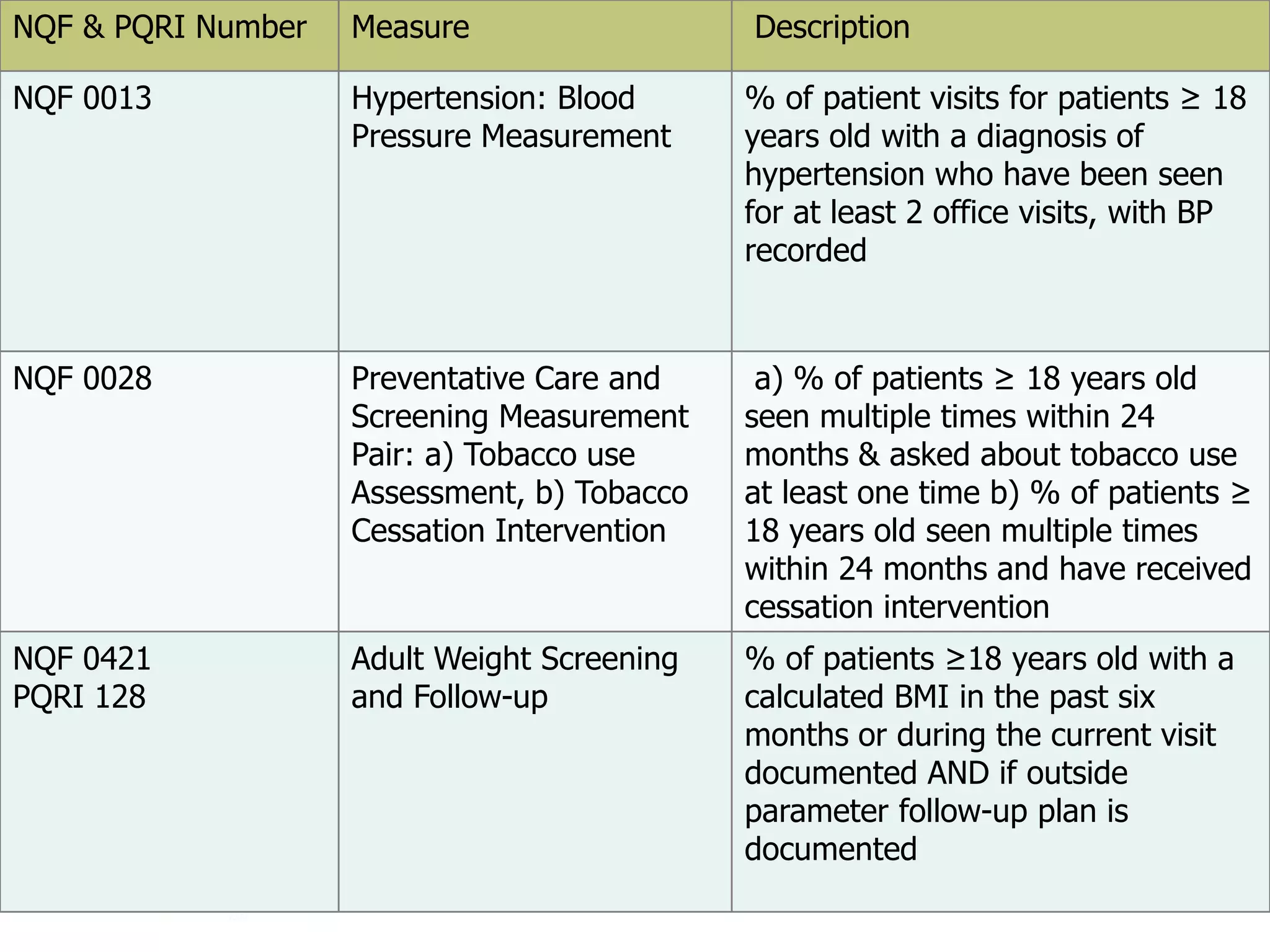
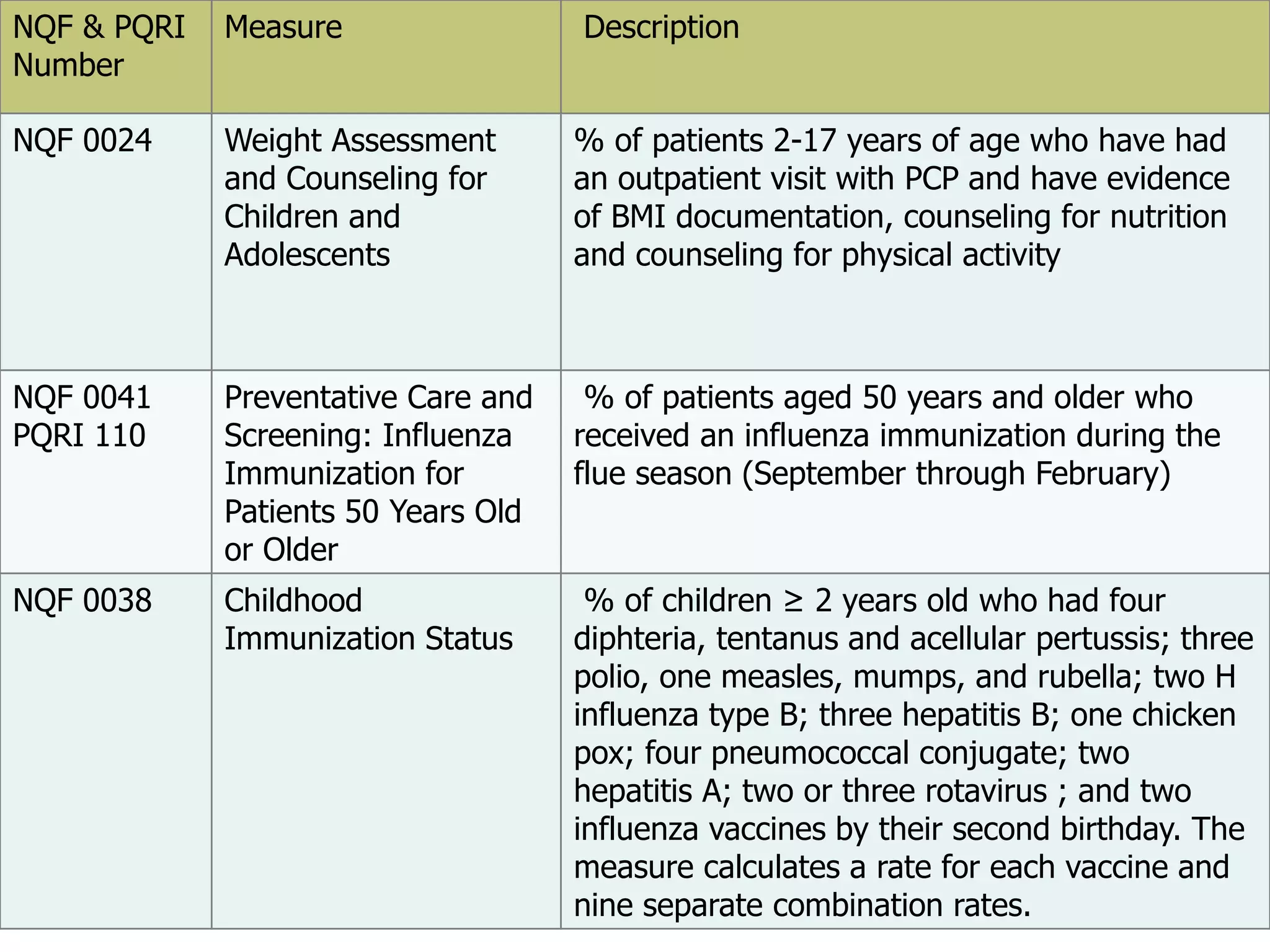
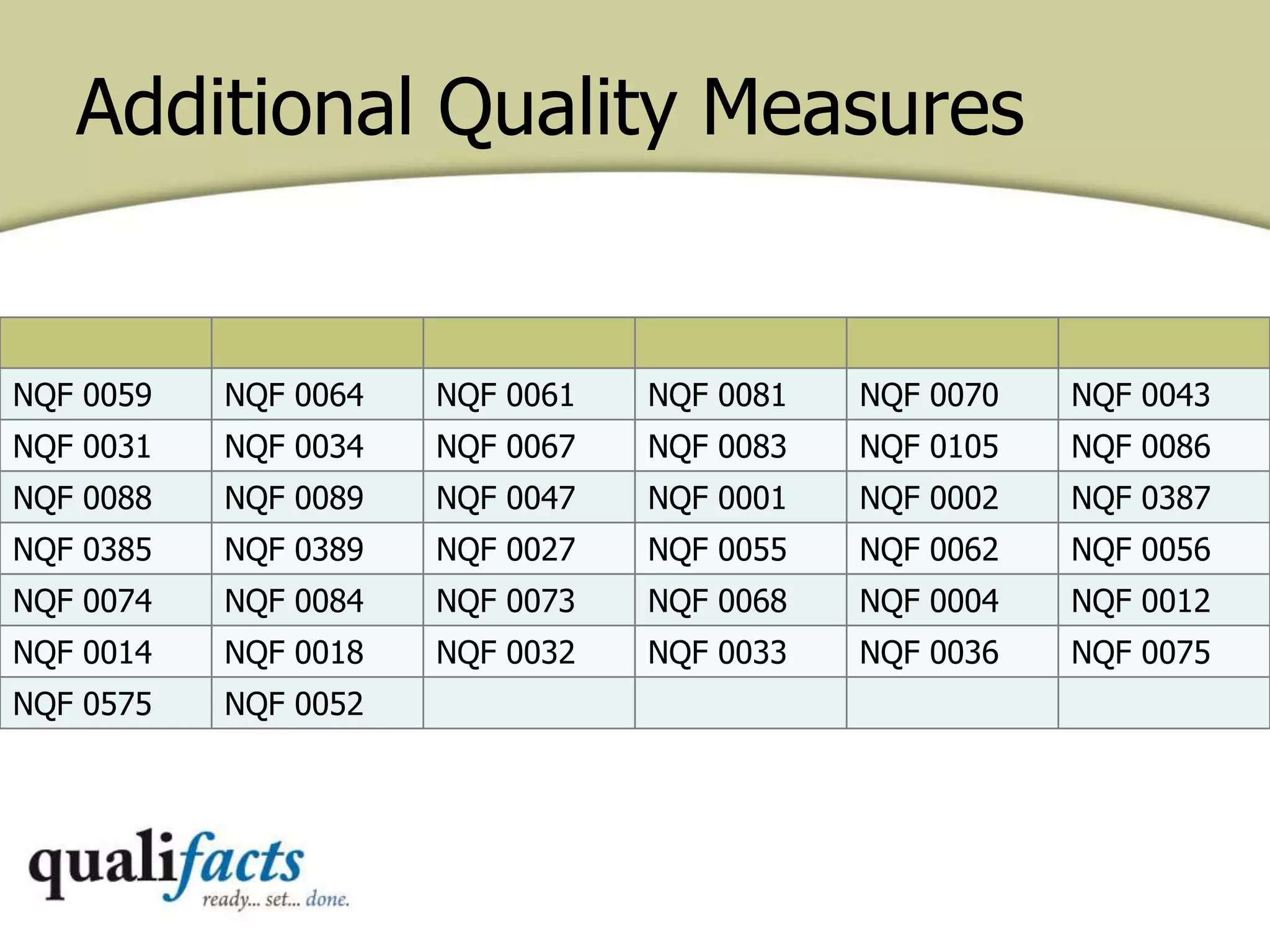
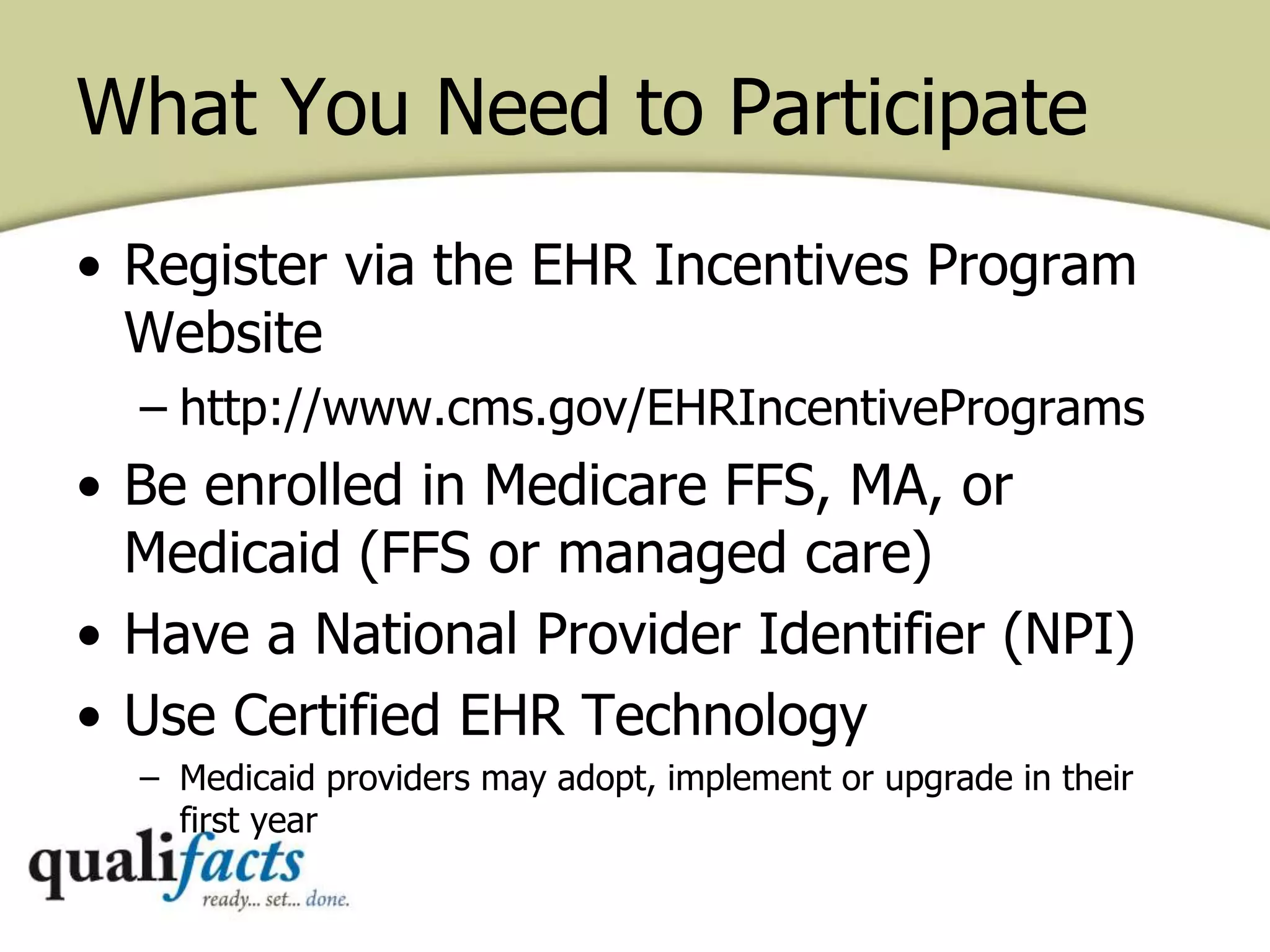
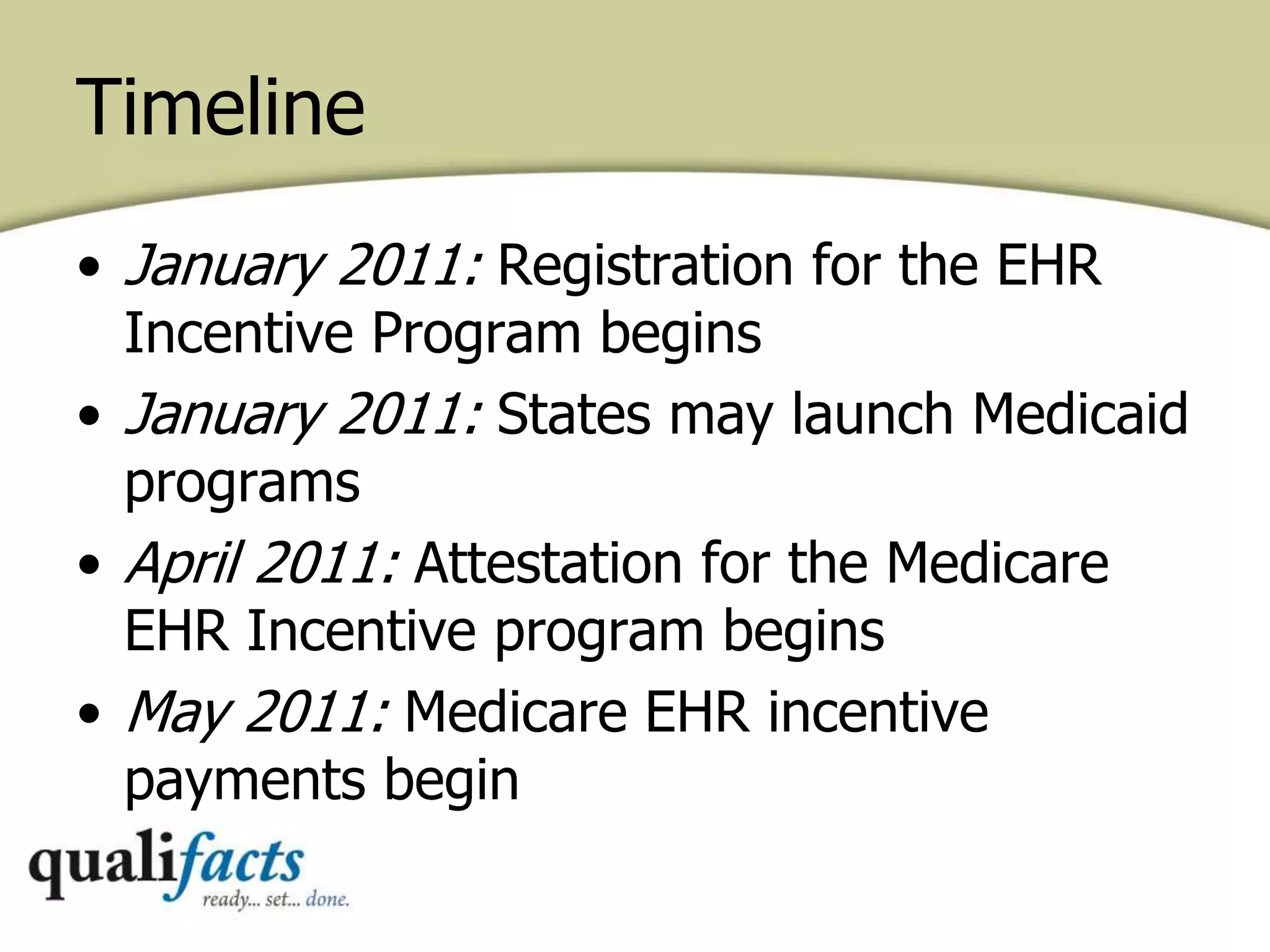
The document provides information on the Medicare and Medicaid EHR incentive programs established under the HITECH Act to promote the meaningful use of electronic health records (EHRs) by eligible providers. It outlines the core and menu requirements to achieve meaningful use certification, associated incentive payment amounts for both programs from 2011-2021, and penalties for providers who do not successfully demonstrate meaningful use. The stages of meaningful use are also summarized, including the objectives and measures for Stage 1 which focus on data capture, tracking clinical conditions, and reporting clinical quality measures.