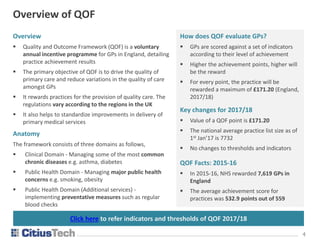
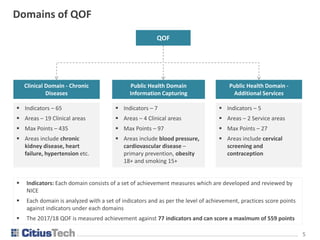
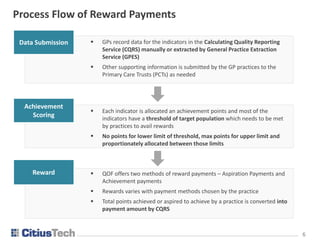
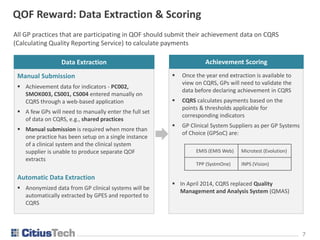
This document provides an overview of the Quality and Outcomes Framework (QOF) for General Practitioners (GPs) in England, detailing its objectives, key changes for 2017/18, and the associated payment processes. It outlines the scoring system based on a set of indicators divided into clinical and public health domains, and describes the methods of reward payments available to practices. The document emphasizes the importance of standardized improvements in primary healthcare quality and addresses challenges in utilizing QOF data effectively.
![1313
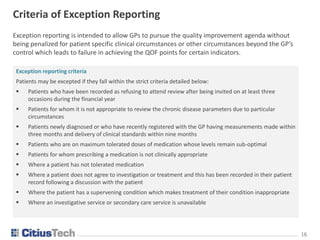
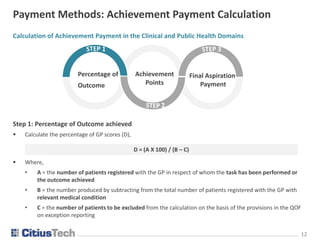
Calculation of Achievement Payment in the Clinical and Public Health Domains
Step 2: Achievement Points
Calculate the number of points which the practice is entitled to in relation to that indicator
Where,
• E = minimum percentage score set for that indicator (lower threshold)
• F = maximum percentage score set for that indicator (upper threshold)
• G = total number of points available in relation to that indicator
Achievement points = [(D – E) / (F – E)] X G
Payment Methods: Achievement Payment Calculation
Final Aspiration
Payment
Percentage of
Outcome
Achievement
Points](https://image.slidesharecdn.com/qualityoutcomesframeworkqof-171106080119/85/Quality-Outcomes-Framework-QOF-13-320.jpg)
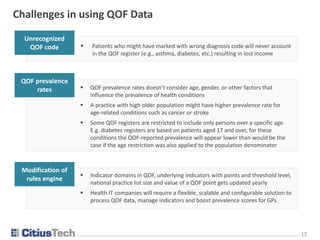
![1515
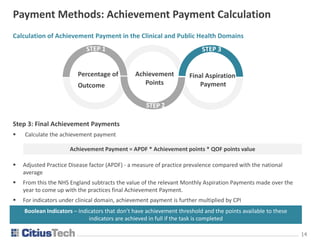
Calculation of Achievement Payment in the Public Health - Additional Services Domain
Step 1: Population Outcome = Practice's relevant target population/GPs registered list size
Step 2: Target Population Factor = Population Outcome / [Avg no of patients registered with all practices in the
relevant target population / Avg of all practices registered list sizes]
Step3: Achievement payment = Target population factor * QOF points value * Achievement points * CPI
Payment Methods: Achievement Payment Calculation
Achievement
Payment
Total Population
Factor
Population
Outcome
Indicators under public health – additional services do not apply to all of the GP’s registered population
and the achievement points will be paid if the service is offered to the relevant target population
Some indicators such as CS002 and CON003 have achievement thresholds, and the method for calculating
achievement points is same as that for this type of indicator in the clinical domain and others are Boolean
indicators](https://image.slidesharecdn.com/qualityoutcomesframeworkqof-171106080119/85/Quality-Outcomes-Framework-QOF-15-320.jpg)