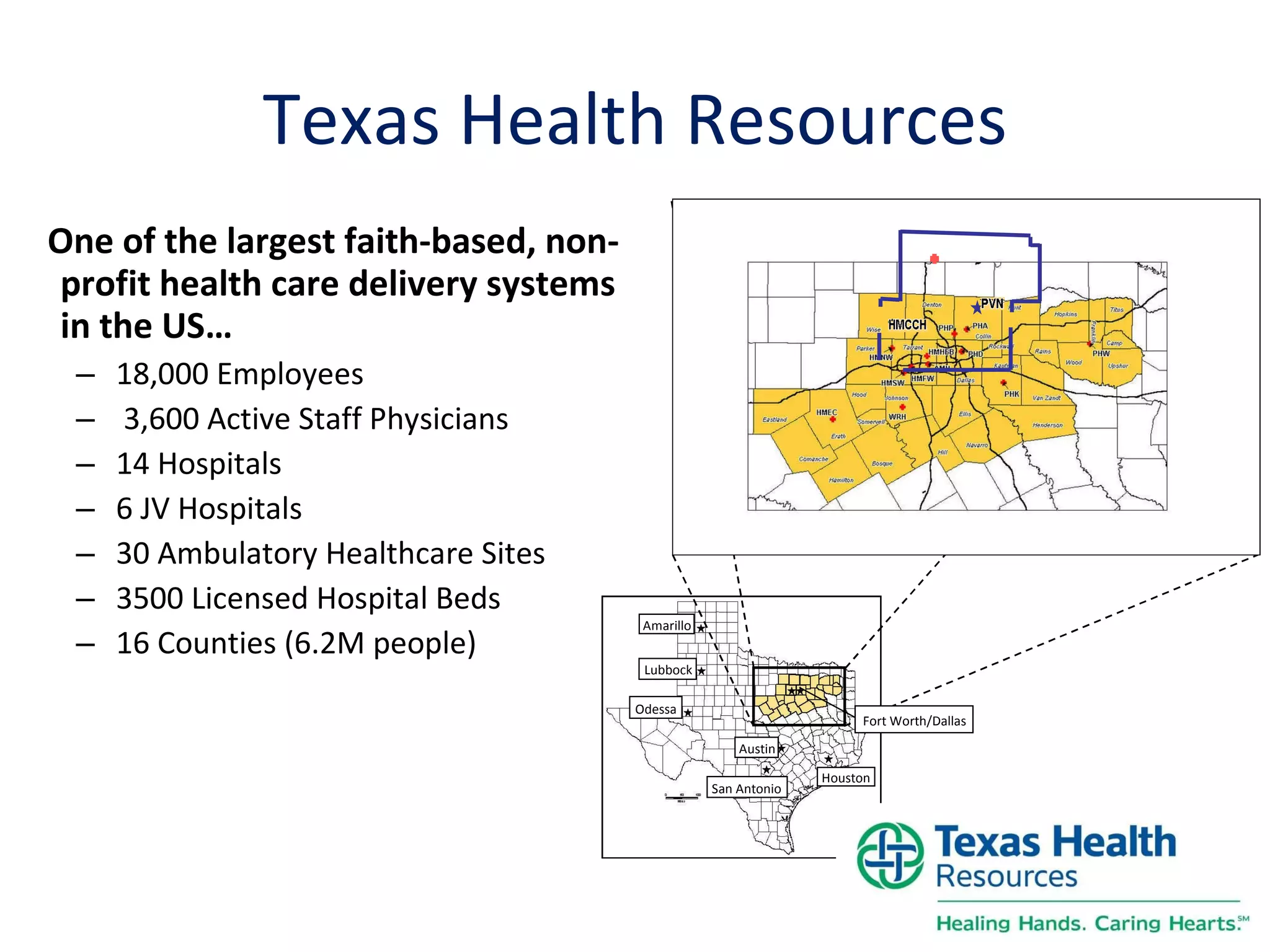
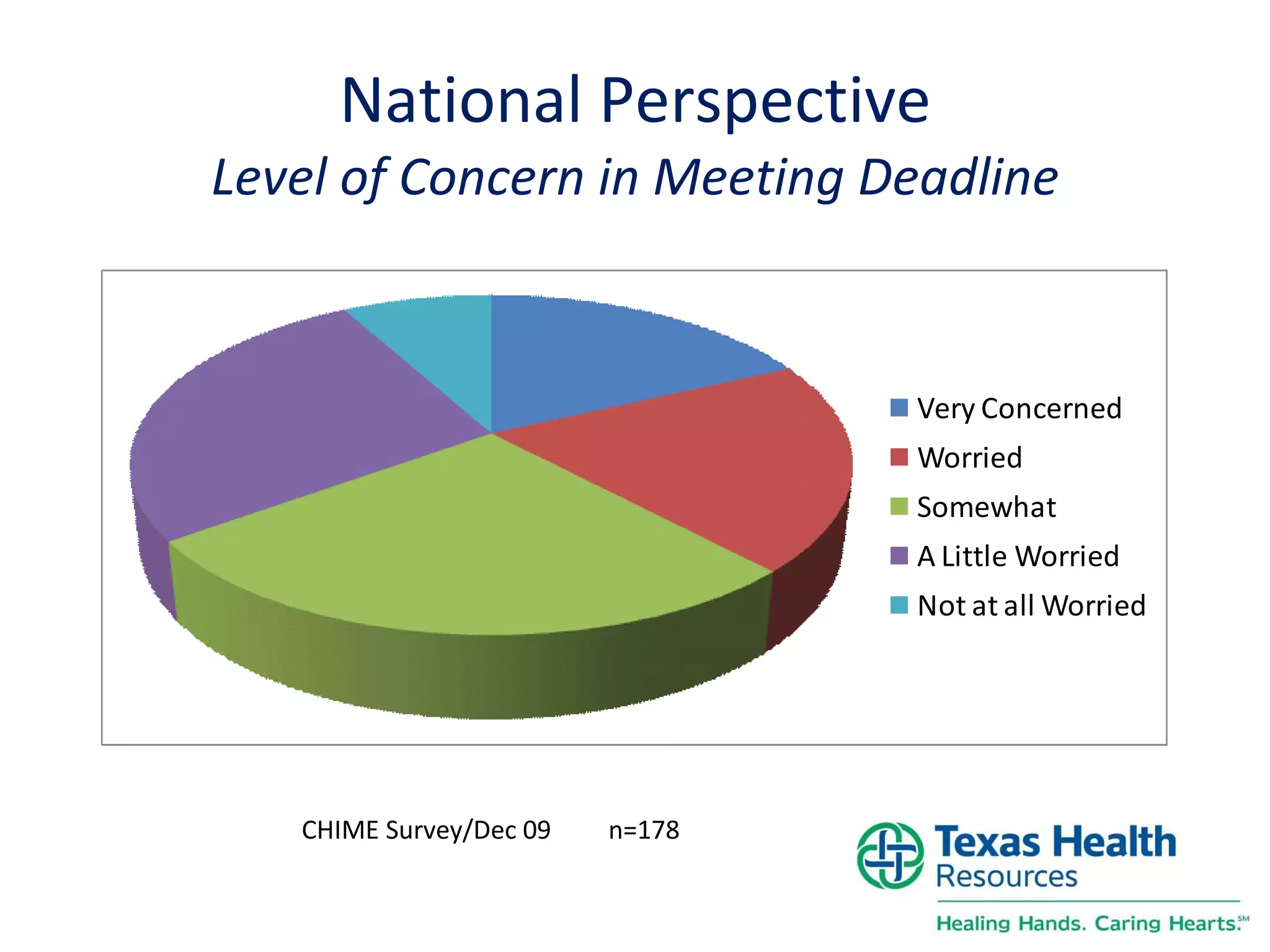
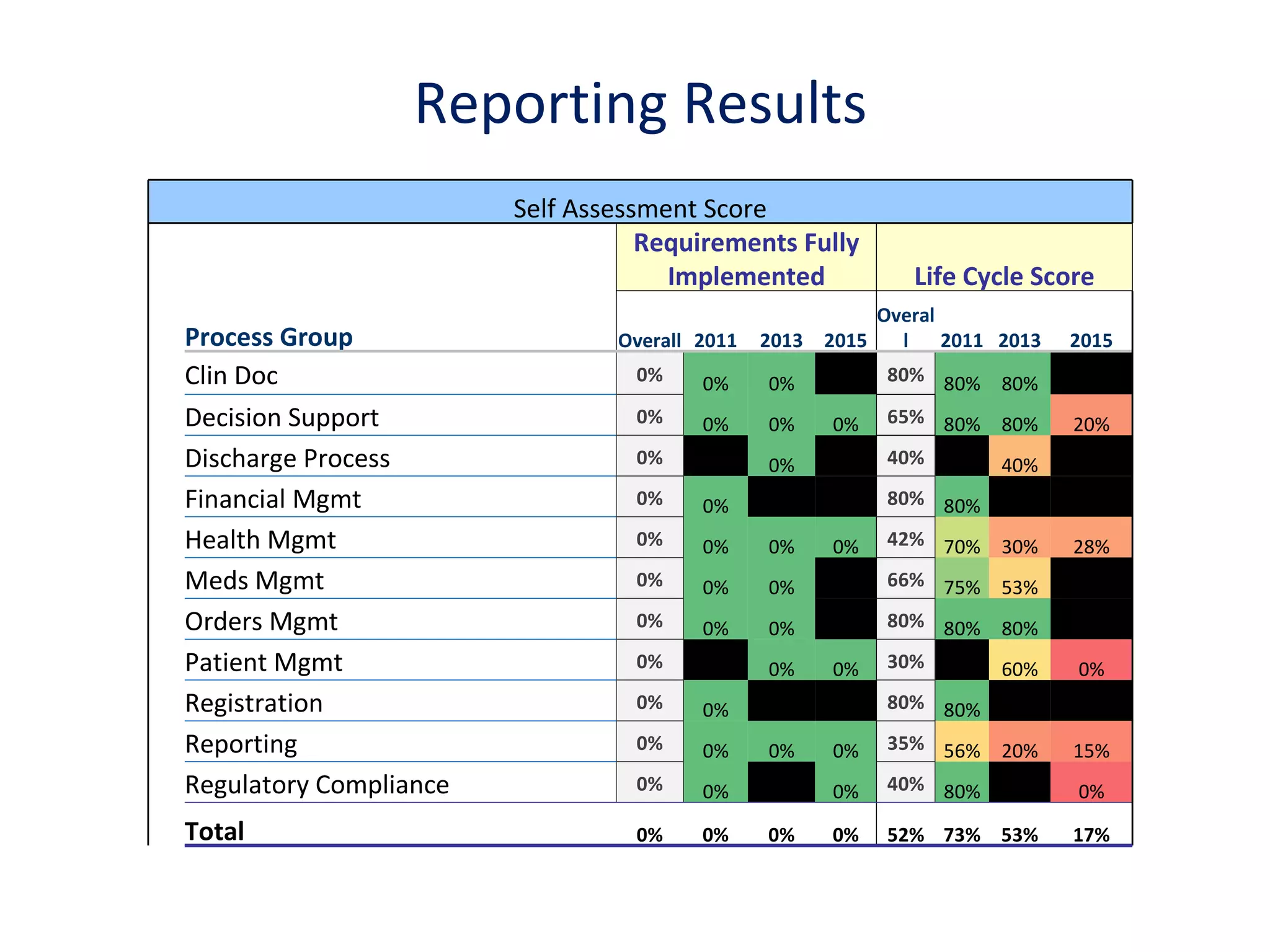
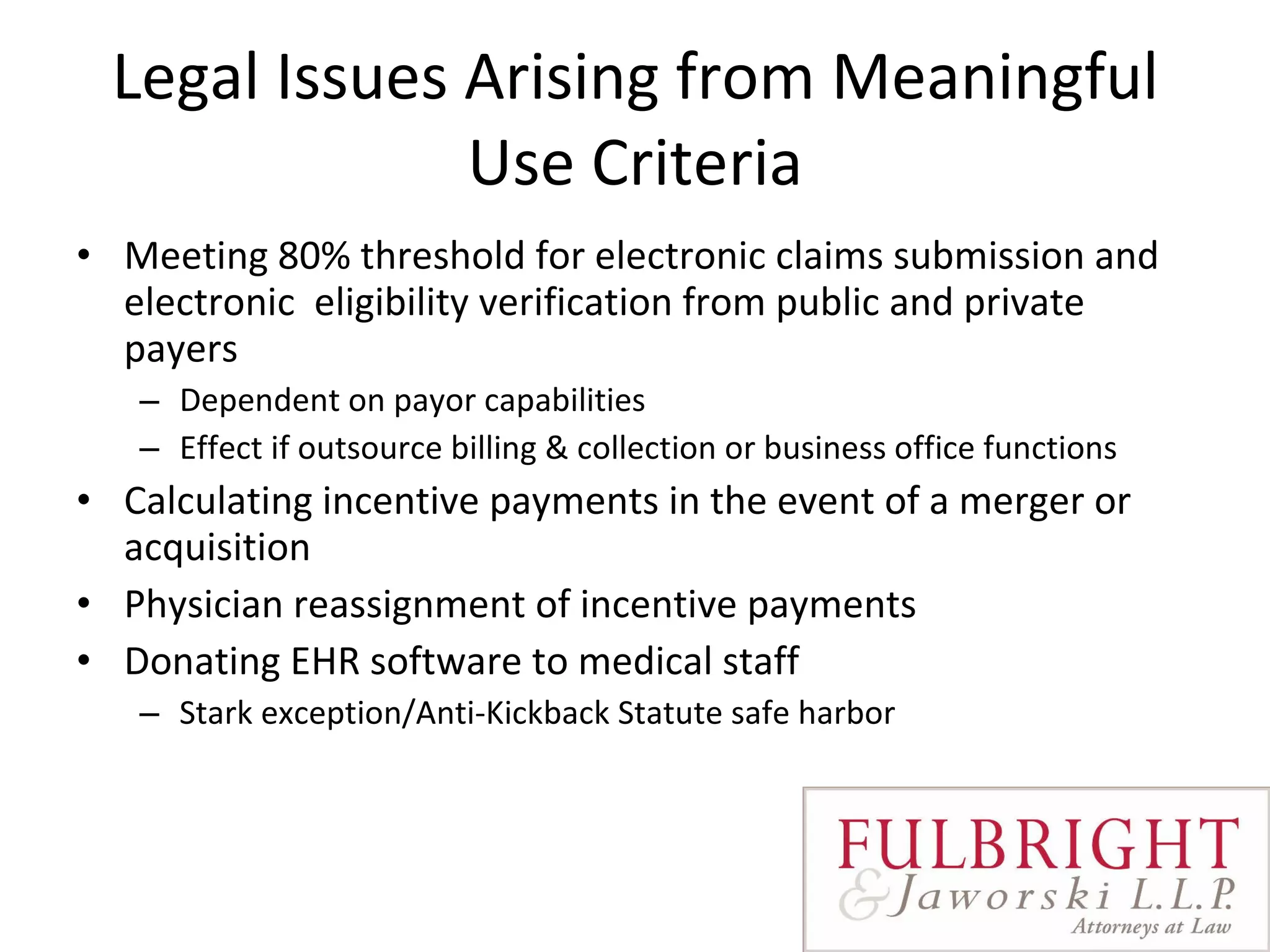
This document summarizes a panel discussion on meaningful use and achieving certification criteria for electronic health records. The panelists discussed how meaningful use goes beyond an IT project and requires organizational readiness, physician alignment, information technology considerations, and vendor sustainability. Key components for achieving meaningful use include governance, communication, physician alignment, IT considerations, quality measures, and legal issues around incentives.






![Reference Documents MU Analysis and Recommendations Report MU Starter Kit Roadmap Check List Stark Talking Points Contact Susan Walker for electronic copies [email_address]](https://image.slidesharecdn.com/meaningfulusewhen51910-12746751643478-phpapp02/75/Meaningful-Use-When-5-19-10-20-2048.jpg)
![Questions & Answers Thank You Susan Walker [email_address]](https://image.slidesharecdn.com/meaningfulusewhen51910-12746751643478-phpapp02/75/Meaningful-Use-When-5-19-10-21-2048.jpg)
![When You Think HEALTH CARE, Think Fulbright. TM AUSTIN • BEIJING • DALLAS • DENVER • DUBAI • HONG KONG • HOUSTON • LONDON • LOS ANGELES MINNEAPOLIS • MUNICH • NEW YORK • RIYADH • SAN ANTONIO • ST. LOUIS • WASHINGTON, D.C. www.fulbright.com • 866-FULBRIGHT [866-385-2744]](https://image.slidesharecdn.com/meaningfulusewhen51910-12746751643478-phpapp02/75/Meaningful-Use-When-5-19-10-39-2048.jpg)