The document discusses the U.S. case study on health information systems, focusing on the evolution and impact of electronic health records (EHRs) and health information technology (HIT) policies, particularly the HITECH Act and its 'meaningful use' regulations. It highlights the benefits of EHRs in improving healthcare efficiency, patient safety, and financial performance while identifying lessons for other countries, such as Thailand, regarding health IT implementation. Key themes include the necessity for leadership, substantial investment, and evidence-based criteria for meaningful use to enhance interoperability and provider acceptance of technology.
































![References (1)
• Amarasingham R, Plantinga L, Diener-West M, Gaskin DJ, Powe NR. Clinical information technologies and
inpatient outcomes: a multiple hospital study. Arch Intern Med. 2009;169(2):108-14.
• Balas EA, Austin SM, Mitchell JA, Ewigman BG, Bopp KD, Brown GD. The clinical value of computerized
information services. A review of 98 randomized clinical trials. Arch Fam Med. 1996;5(5):271-8.
• Blumenthal D. Launching HITECH. N Engl J Med. 2010 Feb 4;362(5):382-5.
• Blumenthal D, DesRoches C, Donelan K, Ferris T, Jha A, Kaushal R, Rao S, Rosenbaum S. Health information
technology in the United States: the information base for progress [Internet]. Princeton (NJ): Robert Wood
Johnson Foundation; 2006 [cited 2010 Oct 14]. 81 p. Available from:
http://www.rwjf.org/files/publications/other/EHRReport0609.pdf
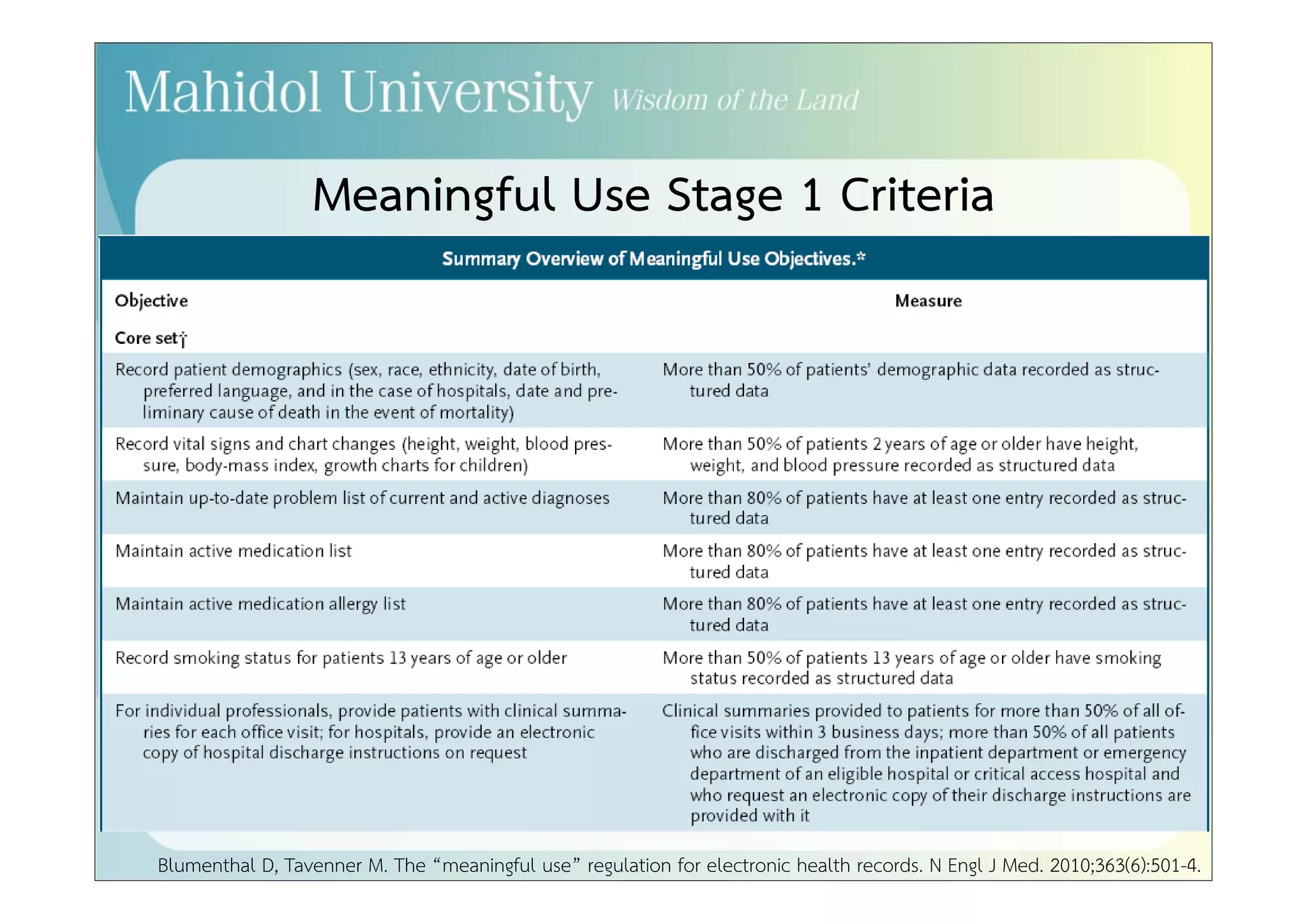
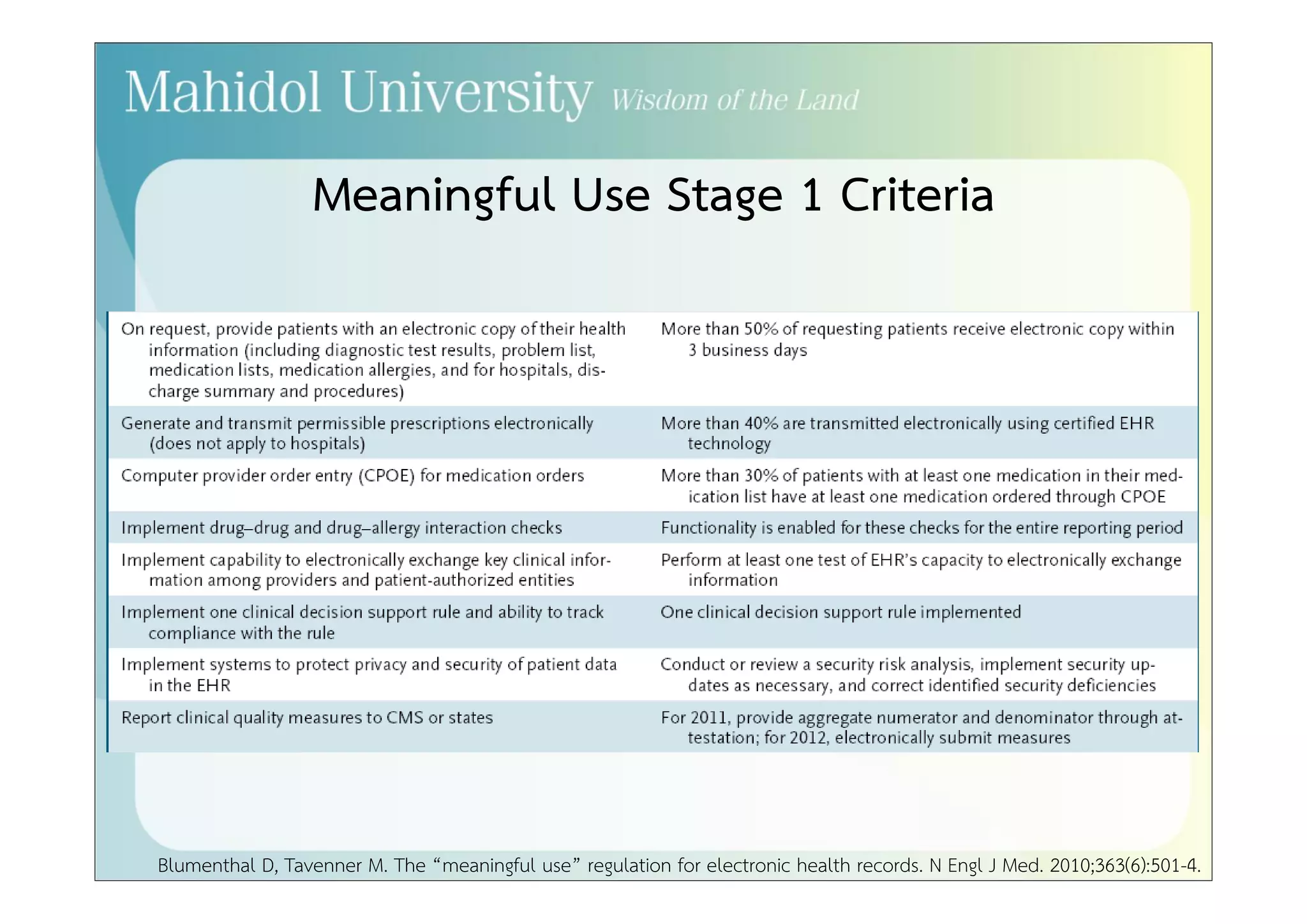
• Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010
Aug 5;363(6):501-4.
• Borzekowski R. Measuring the cost impact of hospital information systems: 1987-1994. J Health Econ.
2009;28(5):939-49.
• Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic review: impact
of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med.
2006;144(10):742-52.](https://image.slidesharecdn.com/policyrelatedtohealthinformationsystems-au-141018073516-conversion-gate01/75/Policy-Related-to-Health-Information-Systems-A-U-S-Case-Study-61-2048.jpg)
![References (2)
• Garg AX, Adhikari NKJ, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized
clinical decision support systems on practitioner performance and patient outcomes: a systematic review.
JAMA. 2005;293(10):1223-38.
• Hsiao C, Beatty PC, Hing ES, Woodwell DA. Electronic medical record/electronic health record use by office-based
physicians: United States, 2008 and preliminary 2009 [Internet]. 2009 [cited 2010 Apr 12]; Available from:
http://www.cdc.gov/nchs/data/hestat/emr_ehr/emr_ehr.pdf
• Institute of Medicine, Board on Health Care Services, Committee on Data Standards for Patient Safety. Key
Capabilities of an electronic health record system: letter report [Internet]. Washington, DC: National Academy
of Sciences; 2003 [cited 2010 Oct 14]. 31 p. Available from: http://www.nap.edu/catalog/10781.html
• Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, Shields A, Rosenbaum S, Blumenthal D.
Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628-38.
• Jha AK, Doolan D, Grandt D, Scott T, Bates DW. The use of health information technology in seven nations. Int
J Med Inform. 2008;77(12):848-54.
• Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support
systems on medication safety: a systematic review. Arch. Intern. Med. 2003;163(12):1409-16.](https://image.slidesharecdn.com/policyrelatedtohealthinformationsystems-au-141018073516-conversion-gate01/75/Policy-Related-to-Health-Information-Systems-A-U-S-Case-Study-62-2048.jpg)
