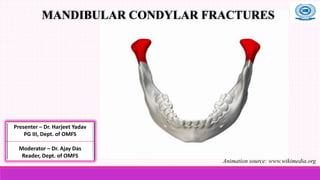
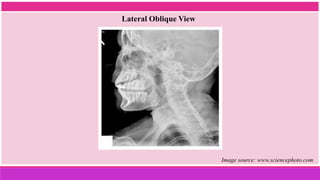
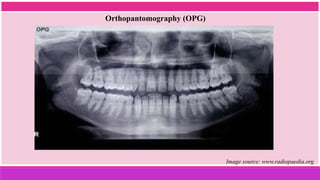
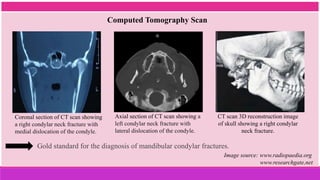
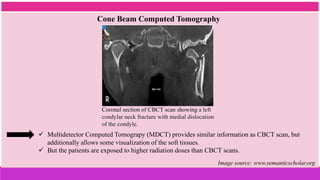
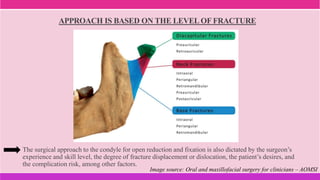
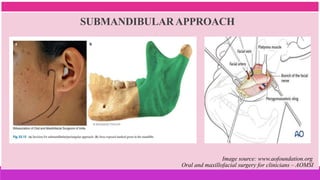
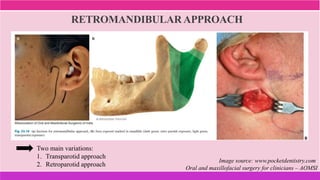
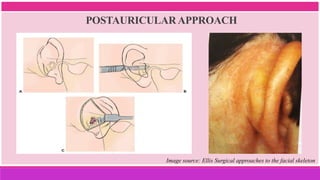
This document discusses mandibular condylar fractures, including:
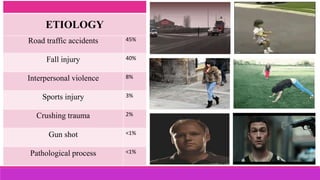
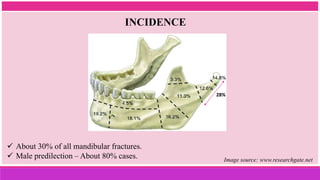
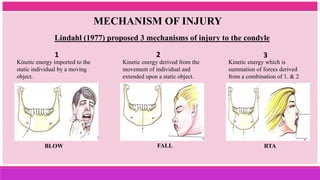
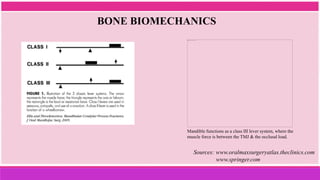
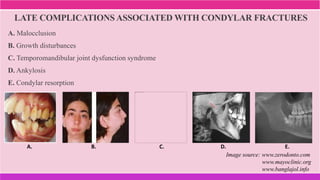
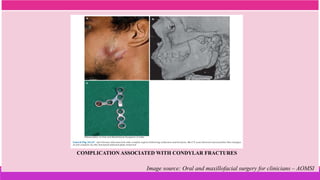
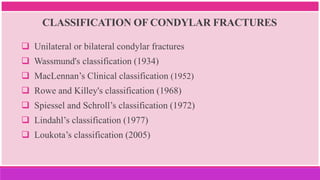
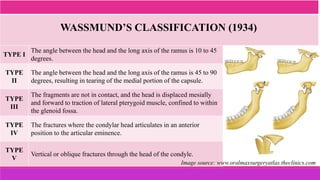
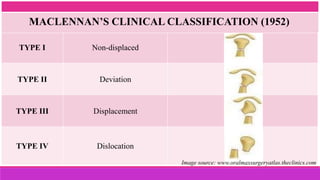
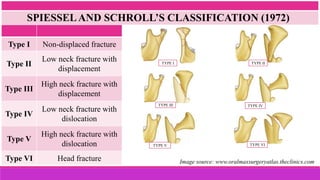
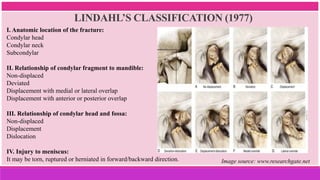
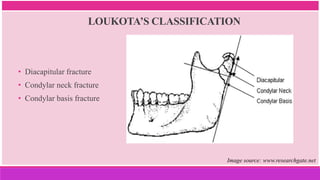
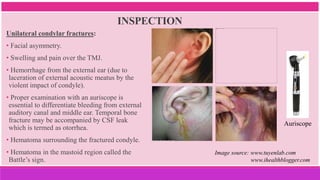
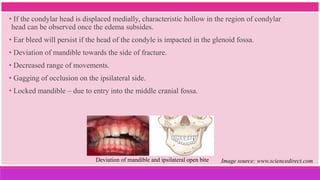
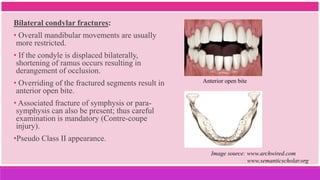
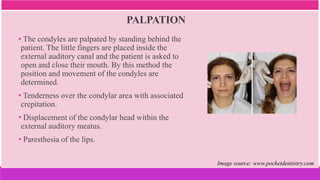
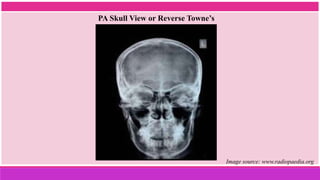
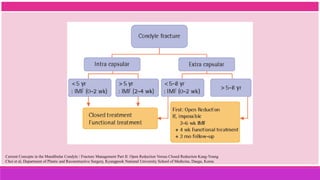
1. It provides an overview of the etiology, classification, clinical features, diagnosis, and management of mandibular condylar fractures.
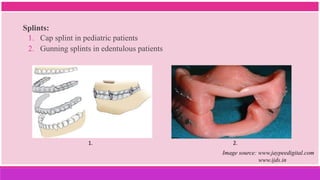
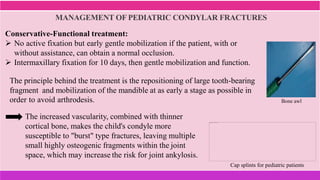
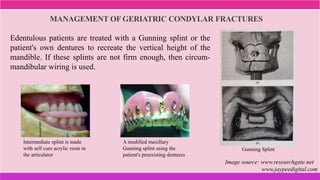
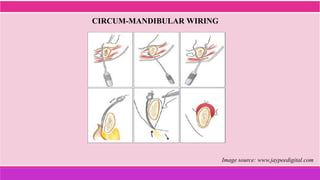
2. Treatment protocols for geriatric and pediatric patients are also discussed.
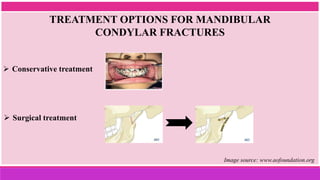
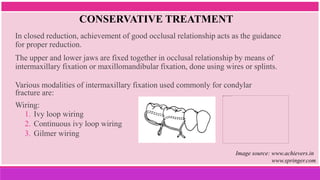
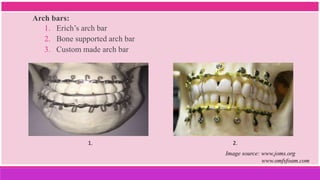
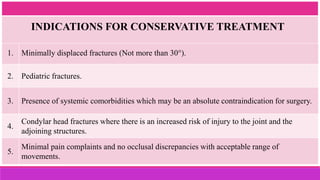
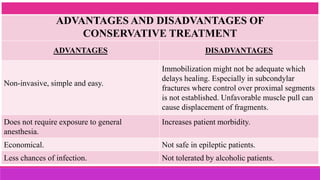
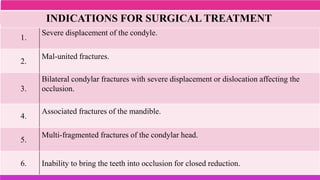
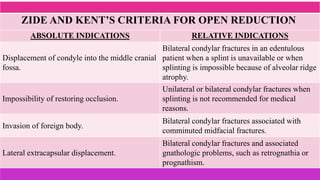
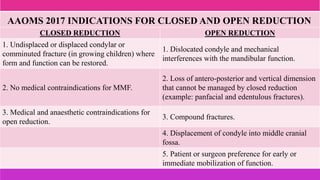
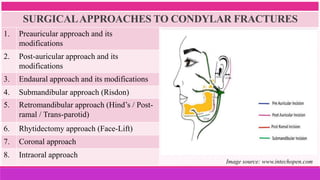
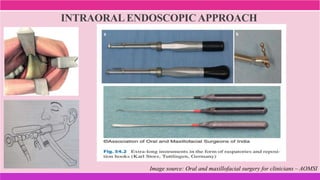
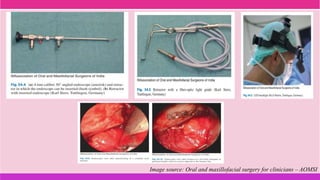
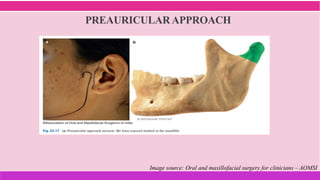
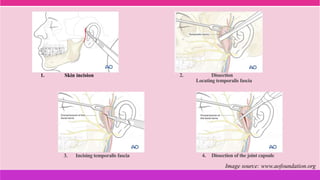
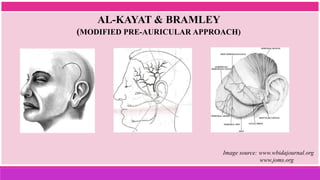
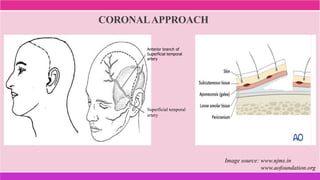
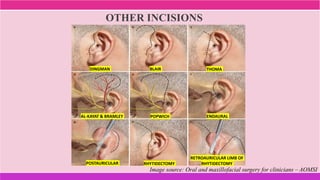
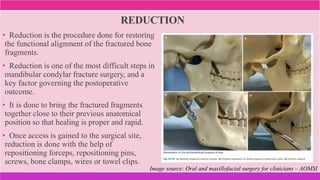
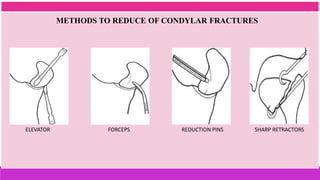
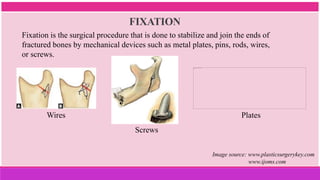
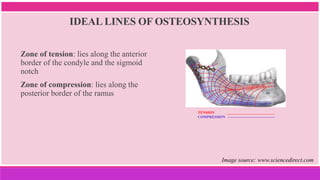
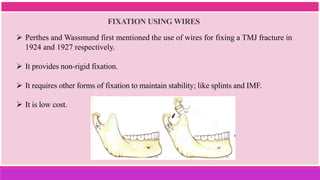
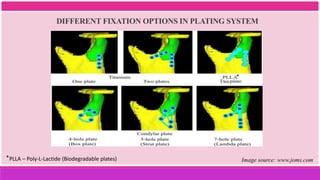
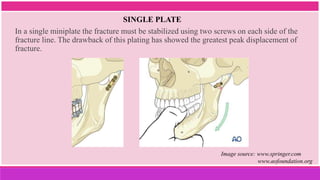
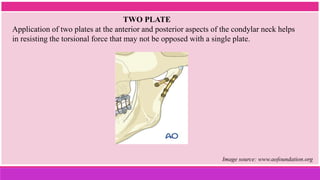
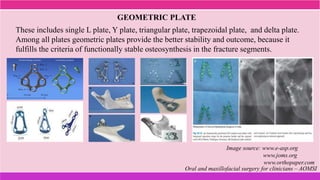
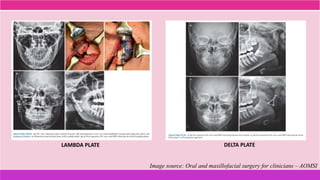
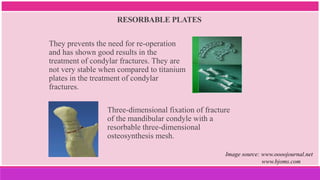
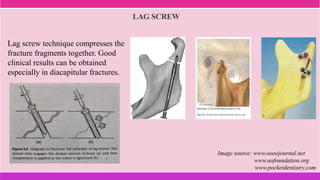
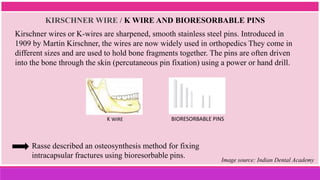
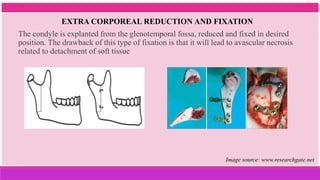
3. The indications and contraindications of closed and open reduction and fixation techniques for condylar fractures are analyzed in detail.