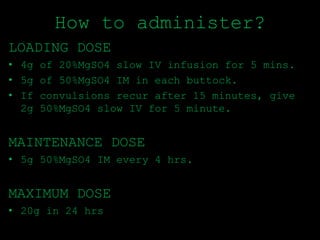
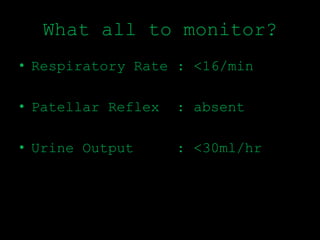
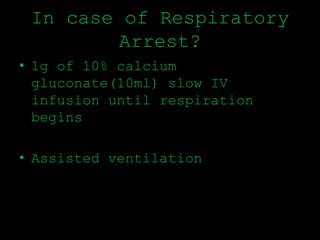
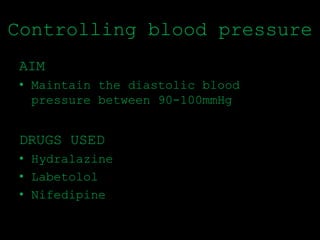
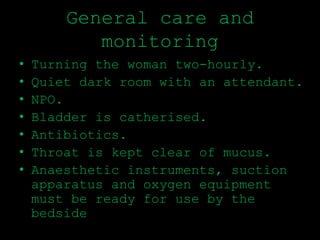
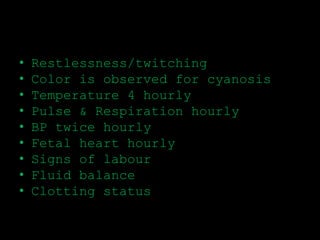
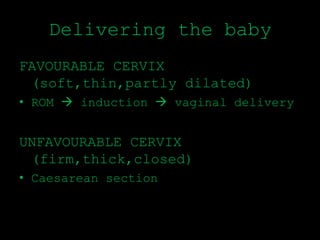
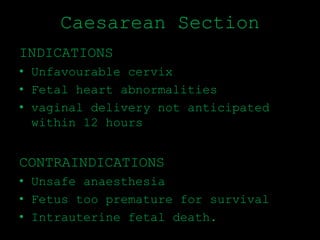
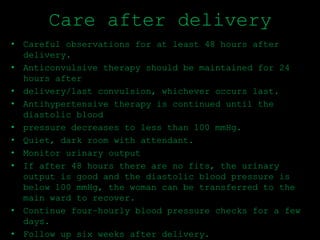
The management of eclampsia involves six stages: 1) ensuring the airway is clear and the woman can breathe, 2) controlling seizures, 3) controlling blood pressure, 4) general care and monitoring, 5) delivering the baby, and 6) care after delivery. Magnesium sulfate is the drug of choice for controlling seizures, and blood pressure is aimed to be maintained between 90-100 mmHg through drugs like hydralazine and labetolol. Delivery should occur within 12 hours of the first seizure, either vaginally if the cervix is favorable or through c-section if not. Care is continued for 48 hours after delivery to monitor for further seizures.