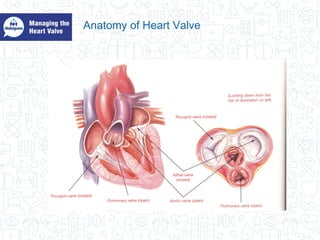
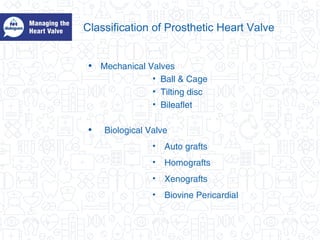
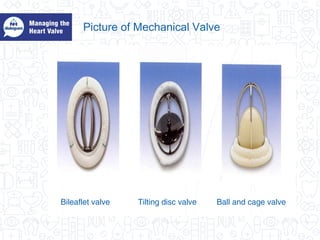
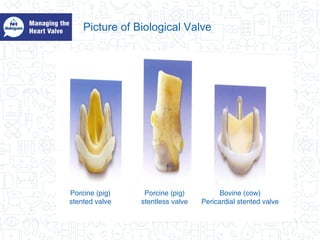
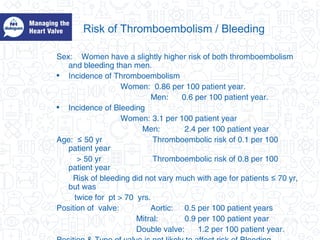
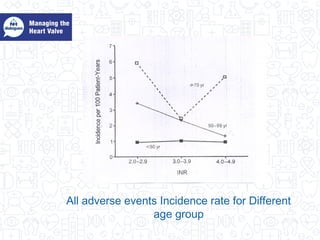
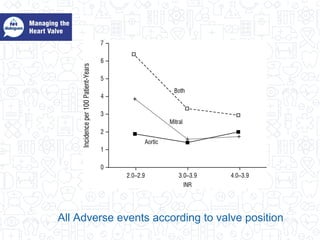
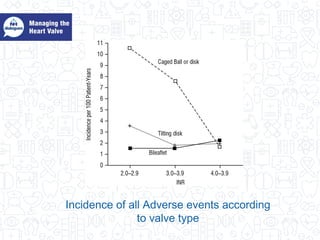
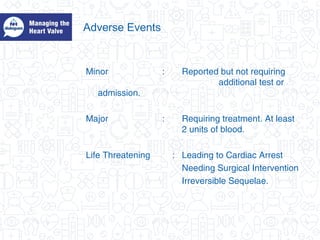
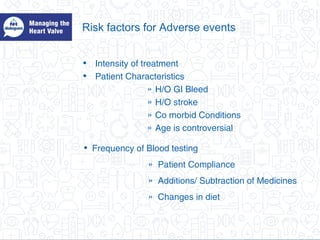
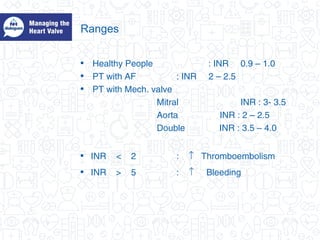
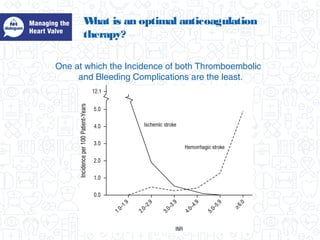
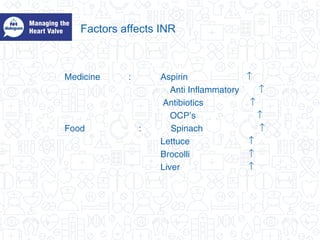
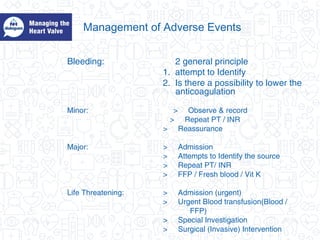
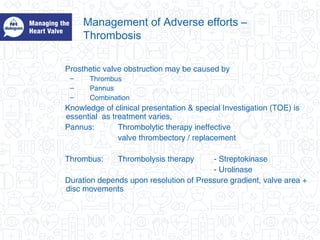
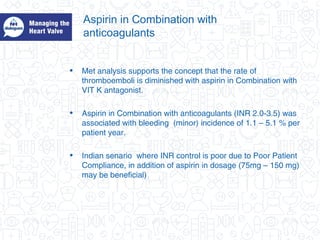
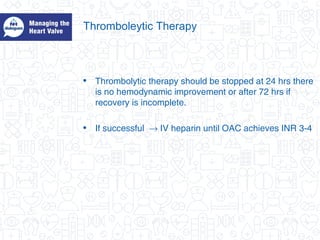
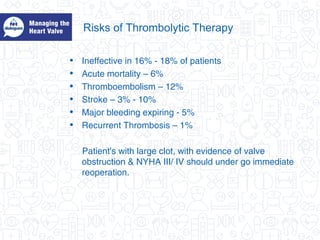
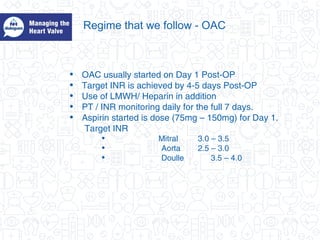
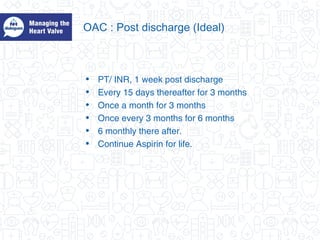
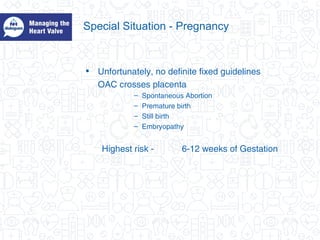
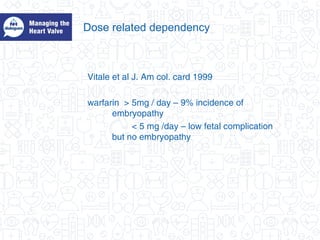
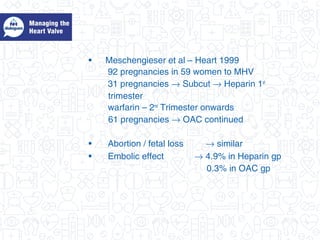
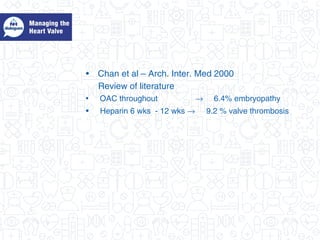
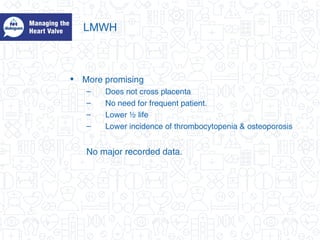
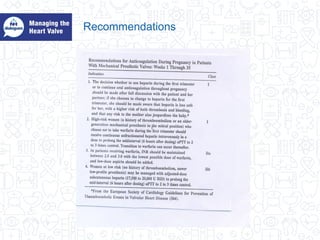
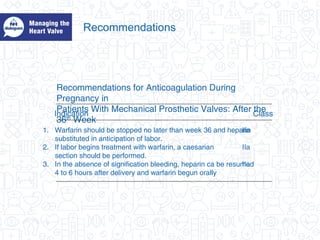
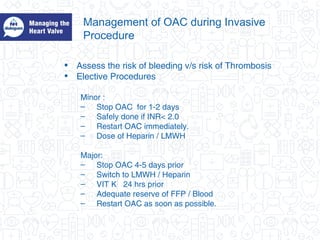
This document discusses the management of patients with prosthetic heart valves, focusing on oral anticoagulation therapy. It describes the anatomy and types of heart valves, including mechanical and biological valves. For patients with mechanical heart valves, lifelong high-intensity oral anticoagulation therapy is required to prevent thromboembolic complications. The risks of thromboembolism and bleeding depend on factors like the patient's sex, age, valve position, and valve type. Optimal anticoagulation aims to minimize both thromboembolic and bleeding risks. Adverse events are discussed and managing complications like bleeding or thrombosis is addressed. Special considerations for anticoagulation during pregnancy and invasive procedures are also covered.