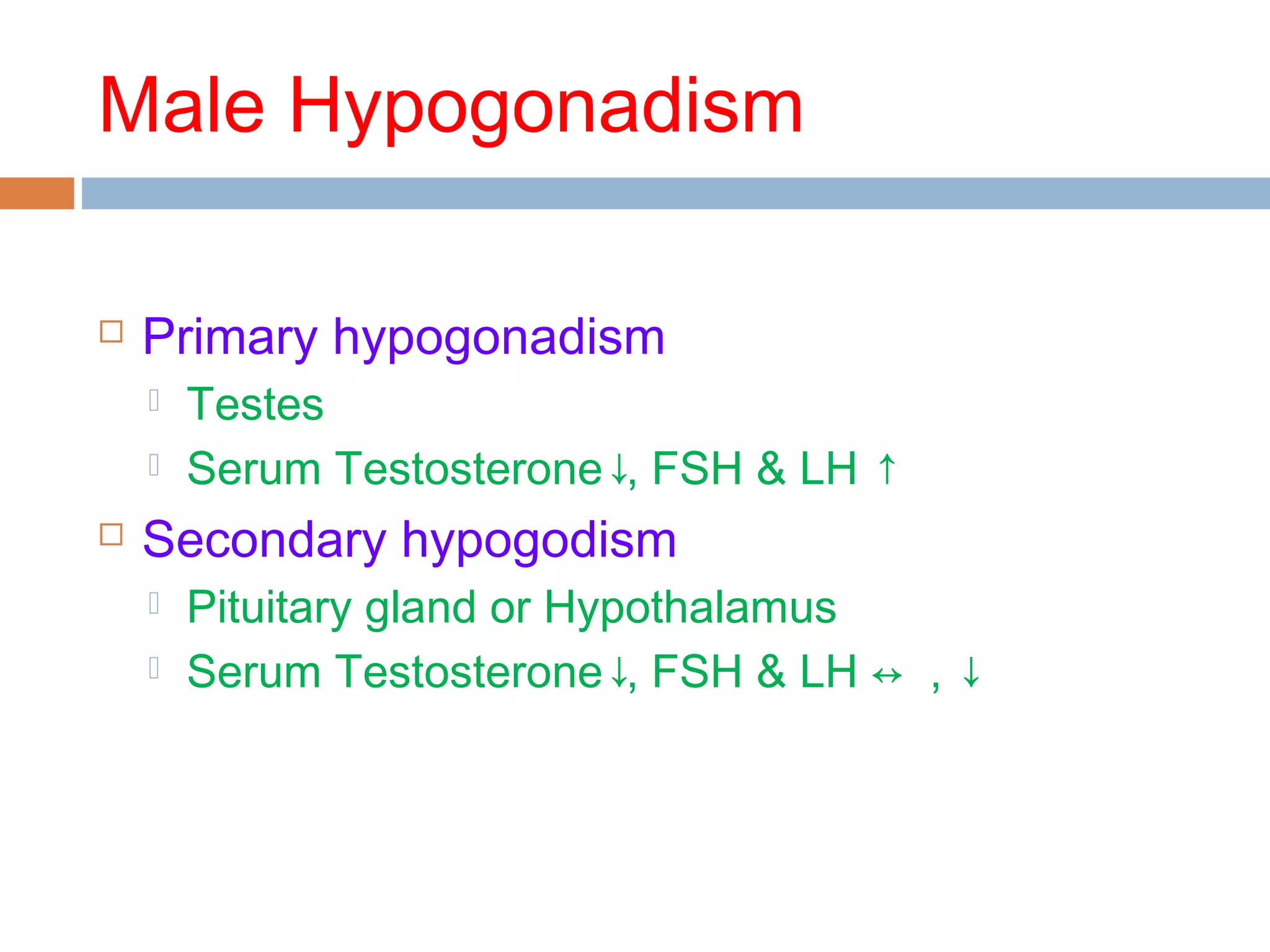
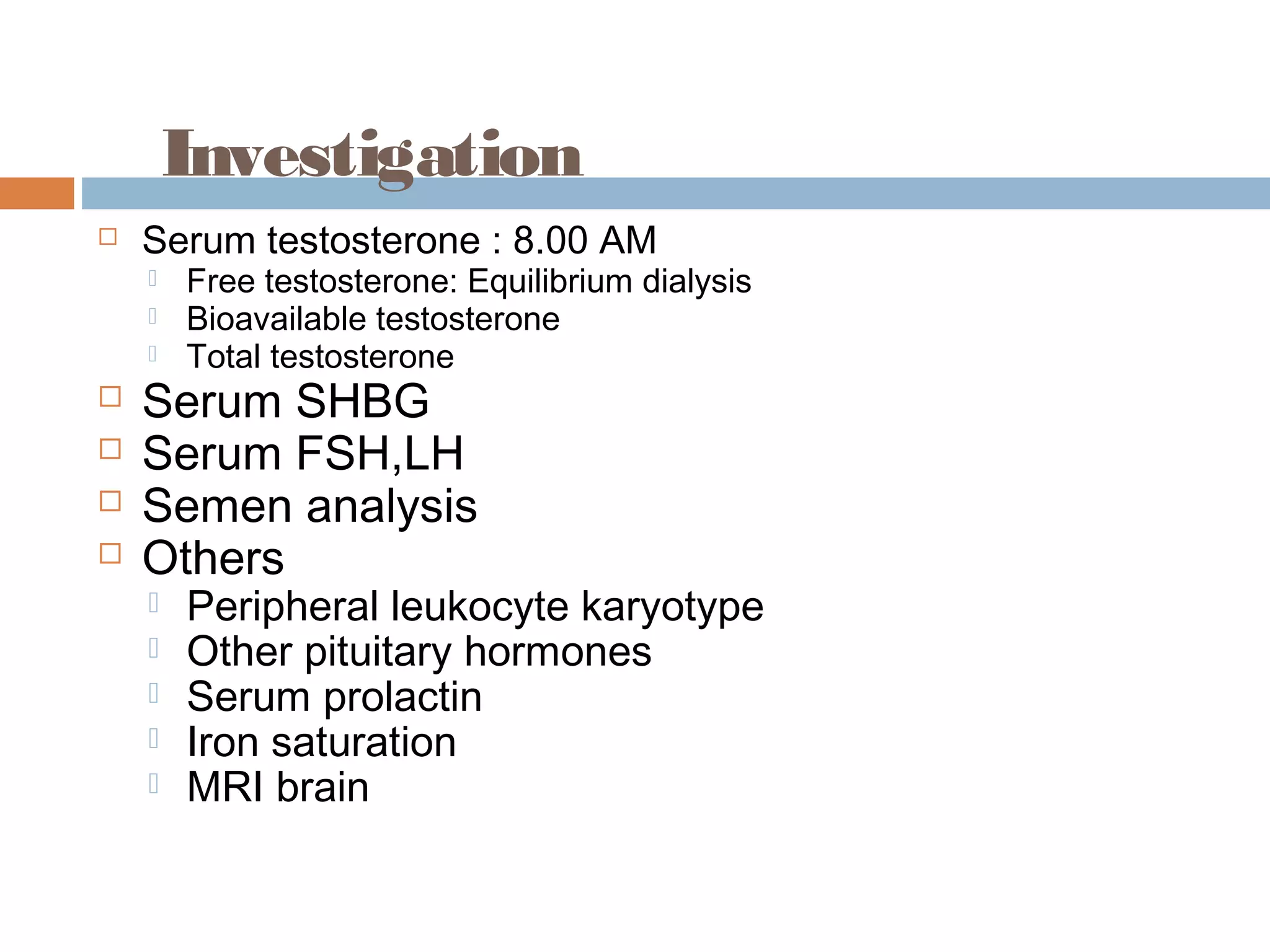
This document discusses male hypogonadism, defined as a decrease in sperm production or testosterone production by the testes. It describes primary hypogonadism, caused by testicular issues, and secondary hypogonadism, caused by pituitary or hypothalamic issues. Causes of primary hypogonadism include Klinefelter's syndrome, infections, drugs, trauma, and genetic mutations. Causes of secondary hypogonadism include tumors, infections, drugs, and chronic illnesses. The document outlines evaluations and tests used in diagnosis, including levels of testosterone, FSH, LH, and additional tests depending on the situation.