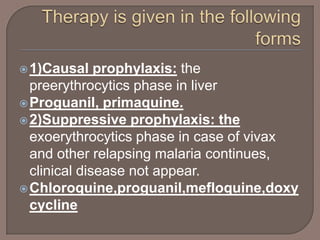
Malaria is caused by Plasmodium parasites transmitted via mosquito bites. The most serious form is caused by P. falciparum. Symptoms include fever, chills, and flu-like illness. Parasites initially develop in the liver then infect red blood cells. Treatment depends on the parasite species and includes chloroquine, primaquine, artemisinins, and others to eliminate symptoms and completely clear the infection. Multiple drugs may be used in combination to combat drug resistance. Prevention involves mosquito control and chemoprophylaxis with drugs like mefloquine, doxycycline or atovaquone-proguanil.