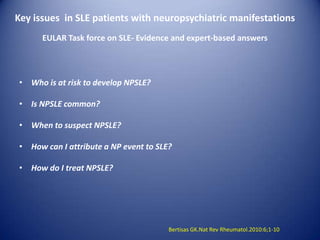
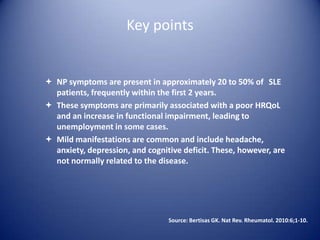
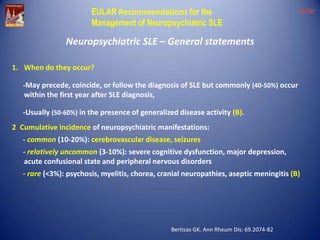
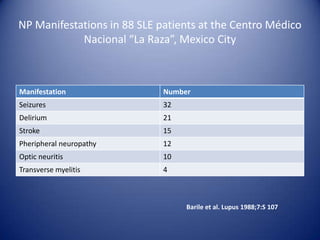
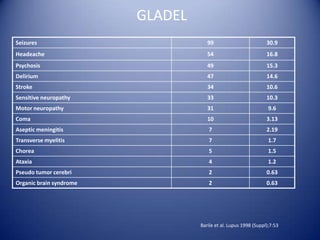
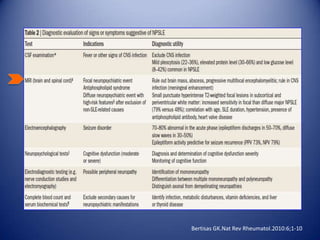
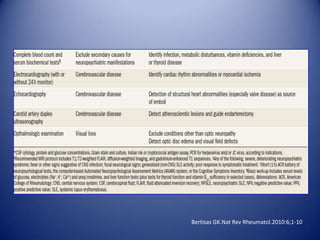
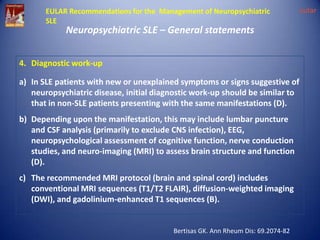
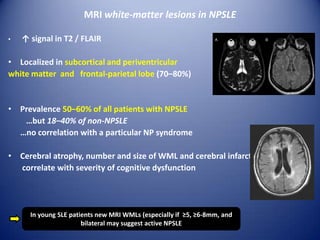
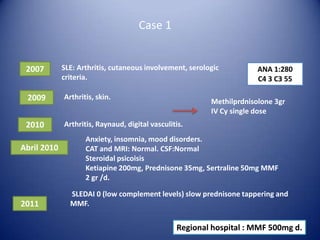
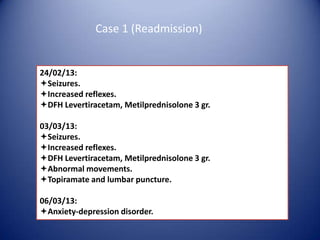
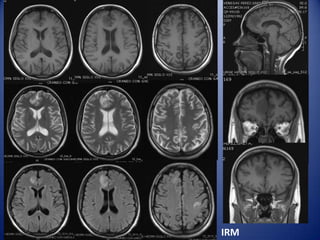
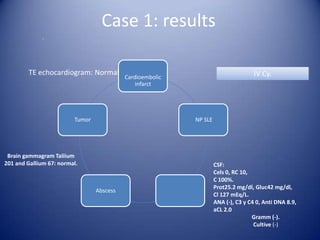
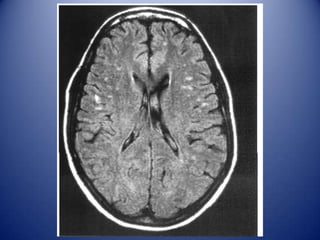
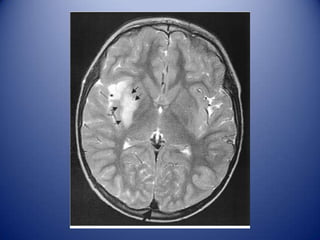
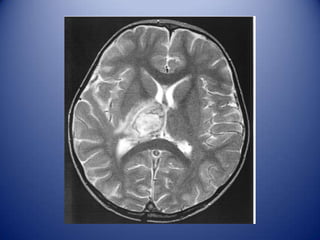
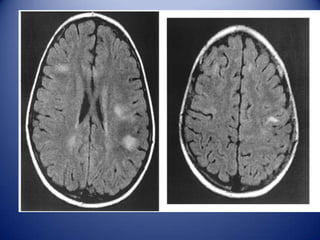
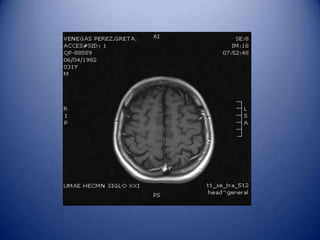
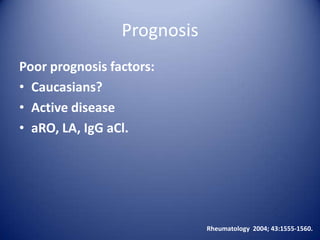
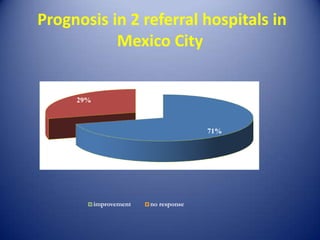
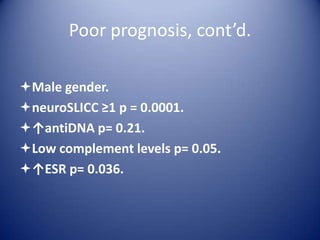
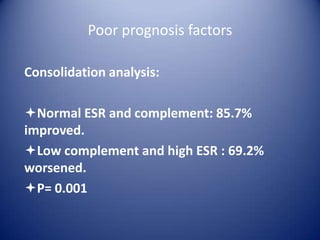
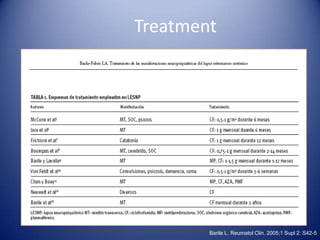
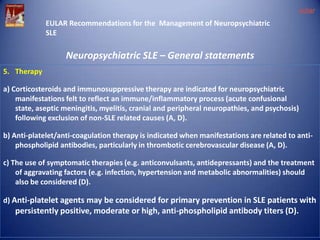
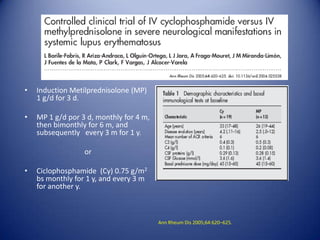
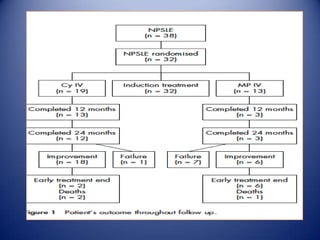
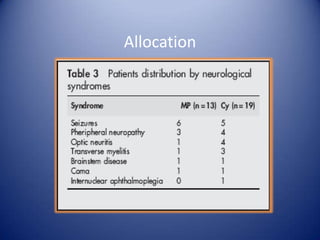
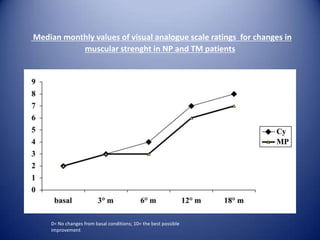
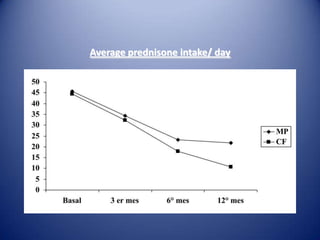
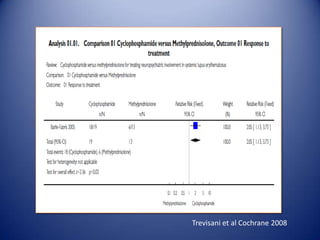
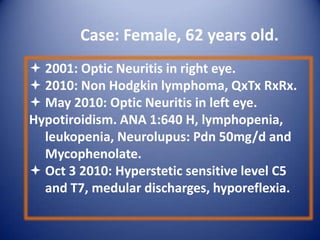
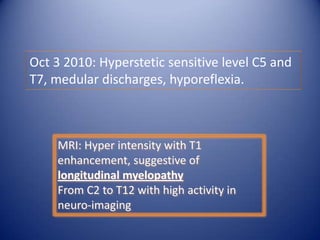
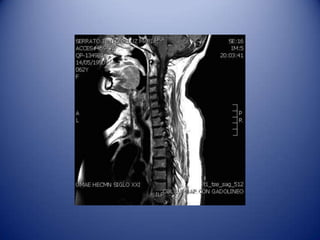
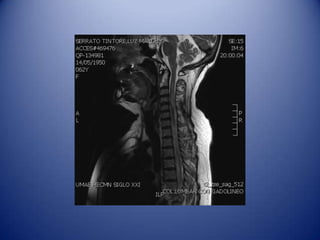
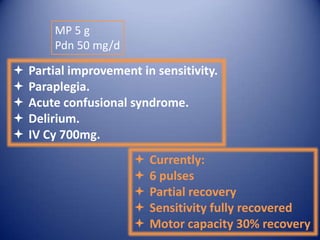
The 10th International Congress on SLE addressed the complexities of neuropsychiatric manifestations in systemic lupus erythematosus (SLE), highlighting their prevalence and diagnostic challenges. Approximately 20-50% of SLE patients experience these symptoms, impacting quality of life and functioning, with management requiring a thorough diagnostic work-up and tailored treatment strategies. EULAR guidelines recommend corticosteroids and immunosuppressive therapies aimed at addressing immune-related manifestations, while also emphasizing the need for individual patient consideration based on specific clinical circumstances.