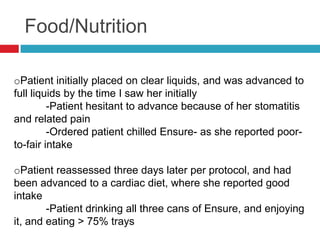
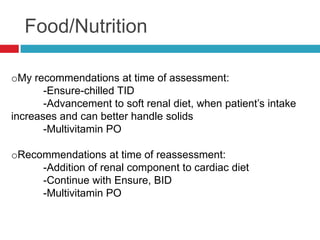
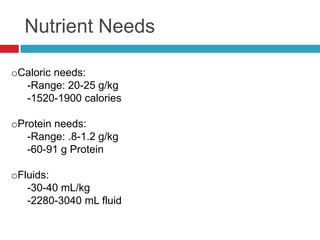
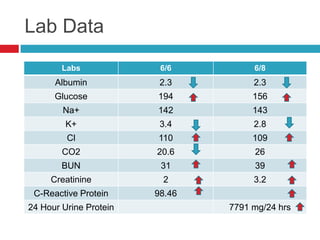
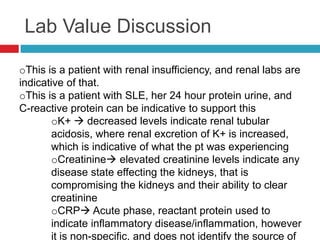
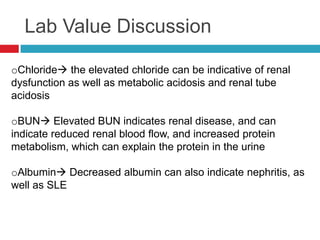
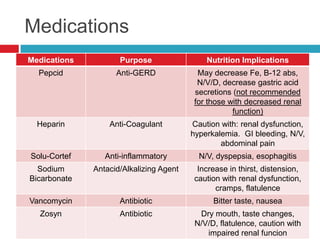
The document discusses a patient with systematic lupus erythematosus (SLE) and impaired renal function, reporting symptoms such as fatigue and stomatitis affecting oral intake. Initial nutrition interventions included a clear liquid diet advanced to a cardiac diet, with recommendations for Ensure and multivitamins. Follow-up indicated improved intake and resolution of stomatitis after dietary adjustments, reflecting the interrelation of lupus and its impact on kidney health.