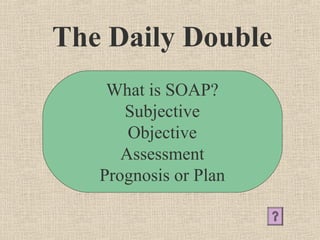
SOAP stands for:
Subjective
Objective
Assessment
Plan
It is a common format for documenting patient encounters and represents the key components of a medical note: Subjective (symptoms), Objective (signs), Assessment (diagnosis), Plan (treatment and follow-up).