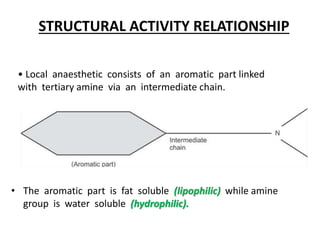
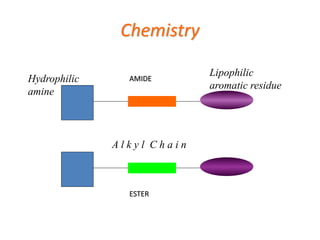
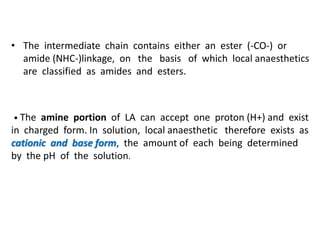
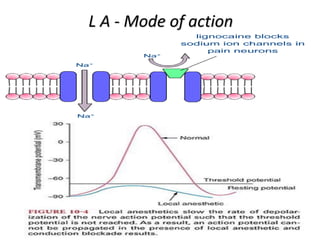
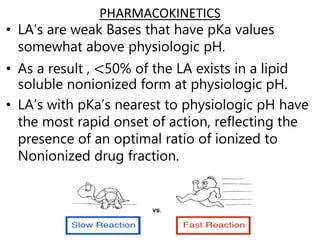
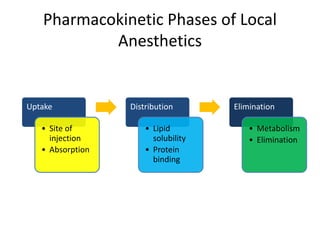
The document presents an extensive overview of local anesthetics, including definitions, historical context, mechanisms of action, properties, classifications, pharmacokinetics, and clinical uses. It details the evolution of local anesthetics from cocaine to various synthetic options and outlines factors influencing their effectiveness and safety. The document emphasizes the importance of structure-activity relationships and the physiological principles underlying the action of these medications on nerve conduction.

![Acidic
LAH+ LA + [H+]
cationic(water sol. Alkaline Base(fat soluble
non-diffusible form) diffusible form)
• That is why carbonated solutions of local
anesthetics show faster onset and increased
efficacy as compared to hydrochloride solutions.](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-15-320.jpg)

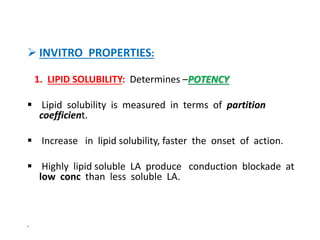
![2. DISSOCIATION CONSTANT: [pKa]
pKa expresses the relationship between ionized and non-ionized
forms of local anesthetic.
pKa is the pH at which the ionized and non-ionized forms are
equal.](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-31-320.jpg)
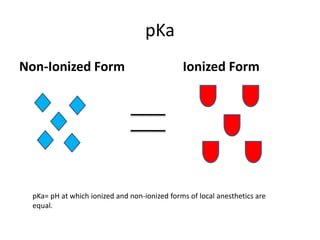
![(Contd..) DISSOCIATION CONSTANT: [Pka]- >7.4
Determines - ONSET OF ACTION
Lower Pka-faster acting [ex:lidocaine;mepivacaine]
Higher Pka-slow acting [ex:bupivacaine; procaine; tetracaine]
LA with Pka close to physiological pH will have high
concentration of unionized form that can cross the
membrane easily.](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-33-320.jpg)
![• OTHERS:
Hyaluronidase
Dextran
Compounding: [ ex:LIDOCAINE+BUPIVACAINE]
Opioids like fentanyl
Dexmeditomidine
Preservative free ketamine.](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-66-320.jpg)

![ METHEMOGLOBINEMIA:
• Due to administration certain drugs that cause oxidation of
Hb to methHb. [ex:prilocaine,benzocaine, and lidocaine]
• MethHb cannot bind O2 or CO2,resulting in loss of Hb
molecules transport function.
• Central cyanosis usually occurs when methHb concentration
exceeds 15%.
• Treatment: 1% methylene blue, 1-2mg/kg IV over 5min.
MALIGNANT HYPERTHERMIA: Lignocaine can cause malignant
hyperthermia in susceptible individuals.](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-71-320.jpg)

![USES OF LOCAL ANAESTHETICS
• Topical(surface anaesthesia)
• Infiltration anaesthesia
• Nerve blocks
• Intravenous regional anaesthesia (BIER’S BLOCK)
• Central neuraxial blocks –spinal and epidural anesthesia.
EMLA[Eutectic mixture of local Anaesthetics]:
o This is unique topical preparation which can anaesthetize
intact skin.
o It is a mixture of 2.5%lidocaine and 2.5%prilocaine.
o It acts slowly and the cream must held in contact with skin
for at least 1hr with the help of adhesive covering.
o Depth of penetration is usually 3-5mm.
o Duration of action is 1-2hrs.](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-86-320.jpg)
![• EMLA is used to make venipuncture painless especially in
children and for procedures like skin grafting and
circumcision.
• EMLA should not be used on cut surfaces and mucous
membranes.
BIER’S BLOCK: [IVRA]
It can be used for short procedures(<90min) involving the
limb extremities.
An IV cannula is placed as far distally as possible in the
extremity to be operated.
A double tourniquet is placed proximally in the same limb](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-87-320.jpg)
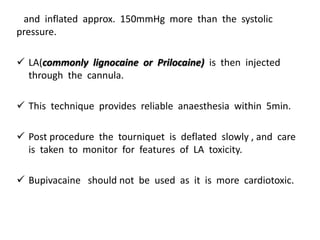
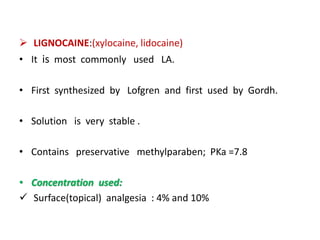
![ Nerve blocks :1 to 2%
Urethral procedures (as jelly) :2%
Spinal :5%
Epidural :1 to 2%
IVRA :0.5%
Infiltration block :1 to 2%
o METABOLISM: Metabolized in liver, excreted by kidney.
o DURATION OF EFFECT: with out Adrenaline :45-60 min
with Adrenaline :2-3 hrs
o MAXIMUM SAFE DOSE : without adrenaline :4.5mg/kg[max 300mg]
with adrenaline :7mg/kg [max 500mg]
• systemic toxicity is much less than bupivacaine.
• Lignocaine releases Ca++ from sarcoplasmic reticulum so
should not be used in pts with h/o malignant hyperthermia.](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-95-320.jpg)
![o OTHER USES:
1) Used for treating ventricular tachycardia.
2) Preservative free lignocaine [available as xylocard 2%] is
used intravenously in dose of 2mg/kg.
3) IV xylocard is used for blunting cardiovascular response
to laryngoscopy and intubation.
MEPIVACAINE: Mepivacaine is similar to lignocaine except
duration of action slightly longer than lignocaine.](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-96-320.jpg)
![ PRILOCAINE:
• It is an amide LA derived from toluidine.
• Many properties [potency , speed of onset , protein binding]
are similar to lignocaine.
• CNS and cardiovascular toxicity is less than that of lignocaine.
• Maximum dose should not be more than 6mg/kg.
• Methemoglobinemia occurs at high dose [>6mg/kg] and this is
because of accumulation of its metabolite ortho toluidine
which can convert Hb to methHb.](https://image.slidesharecdn.com/localanesthetics-200503073053/85/Local-anesthetics-NIYAZ-PV-98-320.jpg)