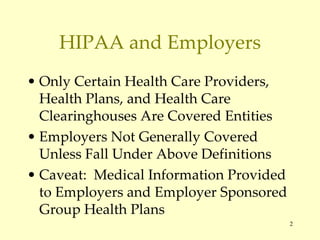
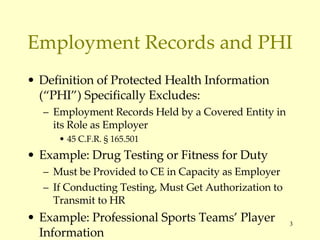
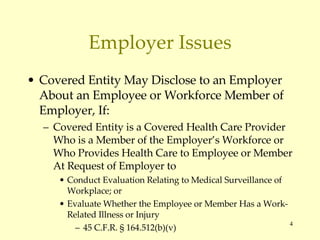
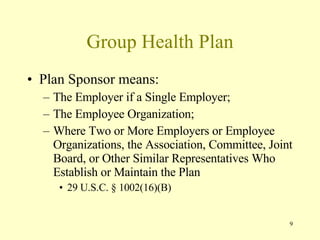
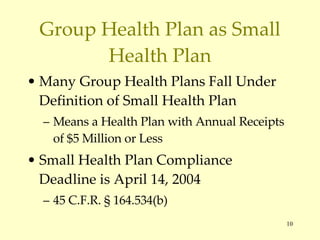
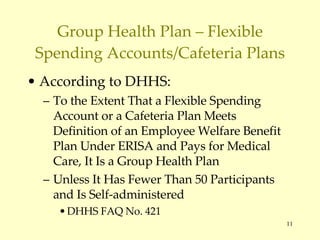
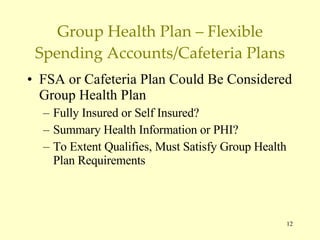
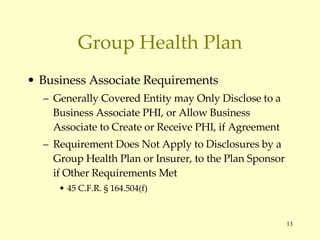
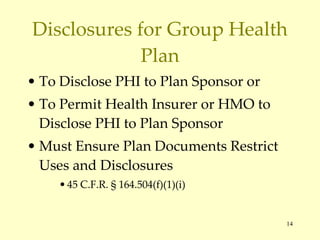
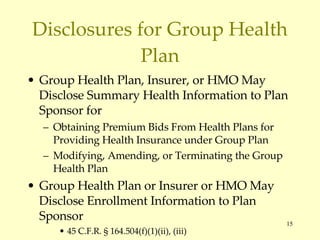
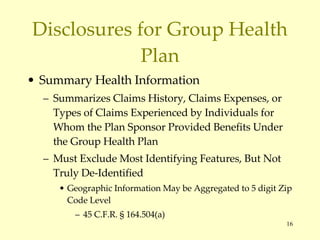
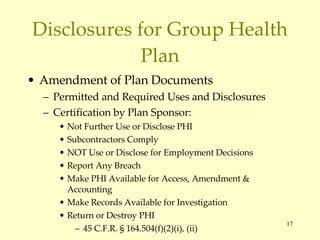
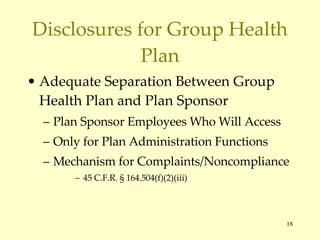
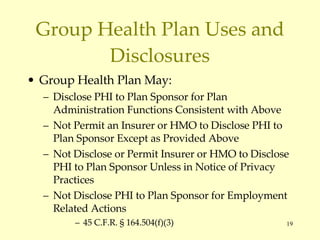
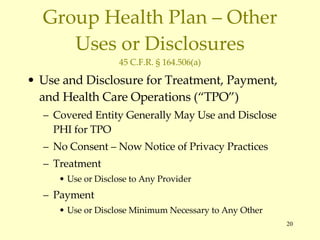
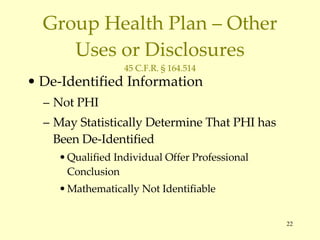
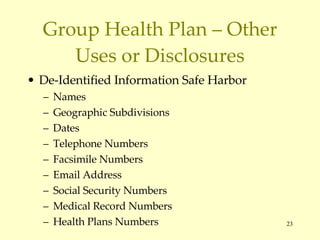
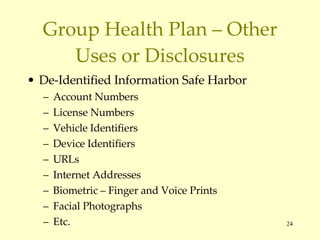
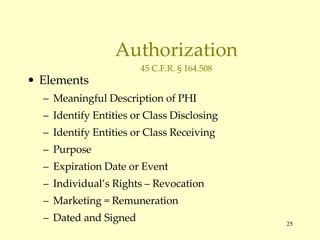
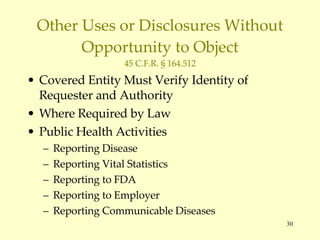
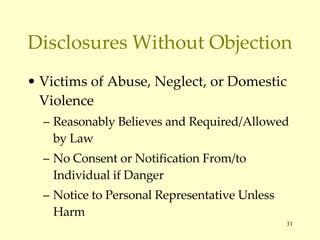
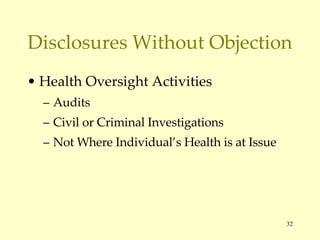
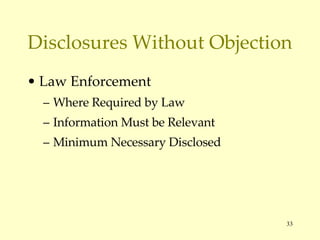
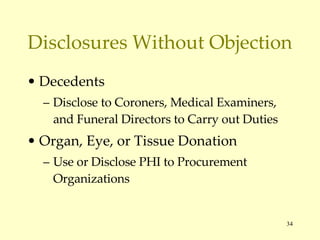
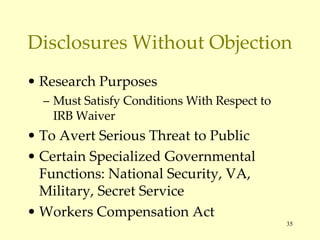
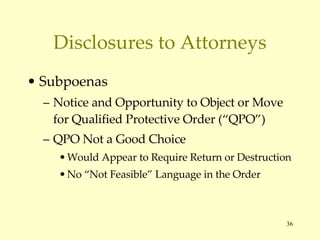
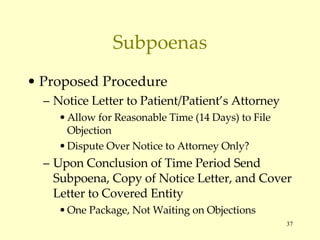
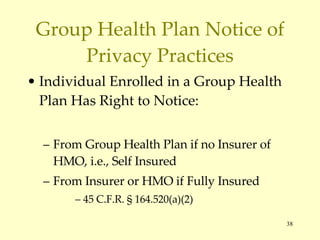
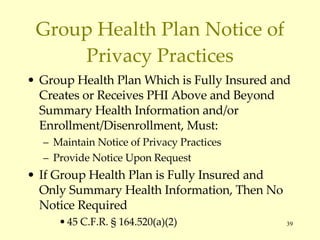
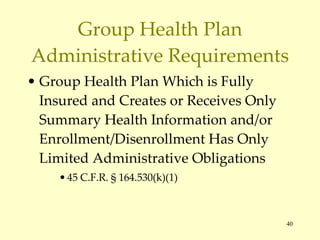
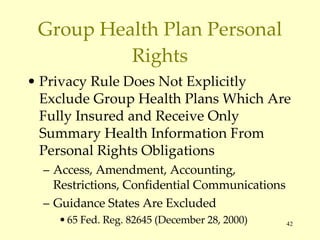
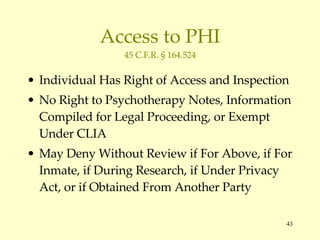
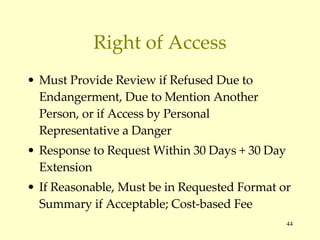
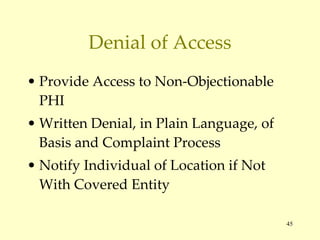
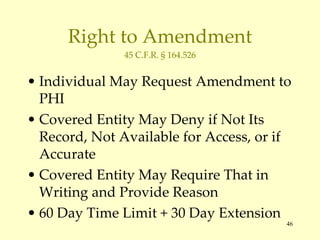
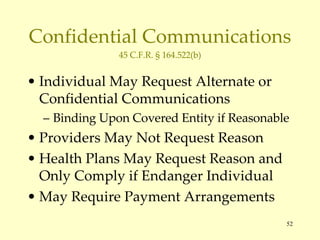
The document outlines key aspects of HIPAA regulations relevant to employers, group health plans, and protected health information (PHI). It details the definitions of covered entities, disclosures permitted under specific circumstances, and compliance requirements for group health plans, including guidelines for handling PHI and patient rights. The content emphasizes the importance for non-health care employers to understand their responsibilities and potential liabilities under HIPAA.



![Conclusion/Questions Gerald “Jud” E. DeLoss Barnwell Whaley Patterson & Helms, LLC 885 Island Park Drive (29492) Post Office Drawer H Charleston, South Carolina 29402 (843) 577-7700 Telephone (843) 577-7708 Facsimile [email_address] www.barnwell-whaley.com](https://image.slidesharecdn.com/delossi-1212757461393710-9/85/slide-54-320.jpg)