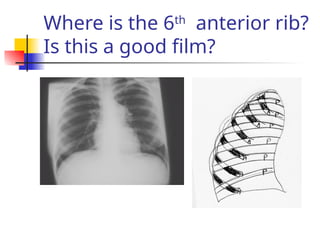
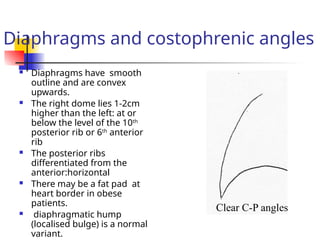
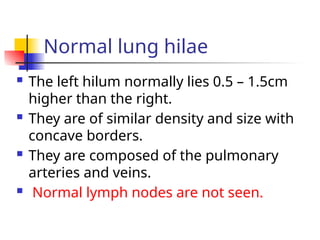
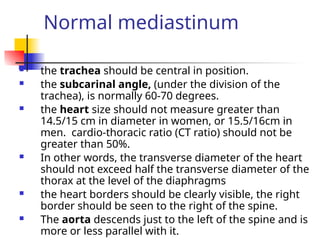
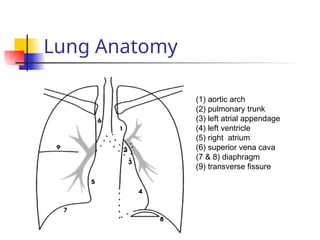
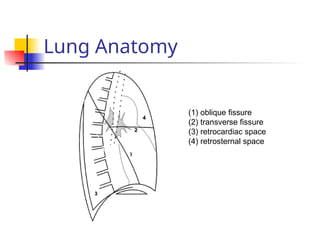
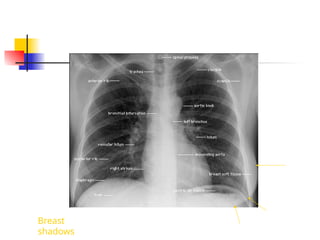
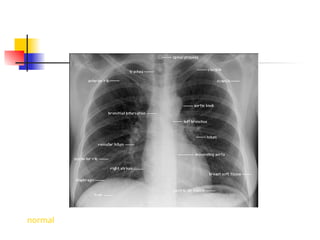
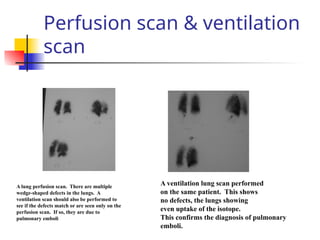
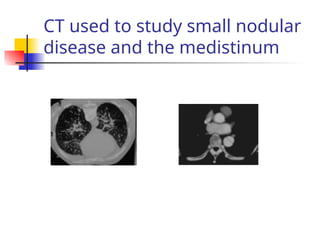
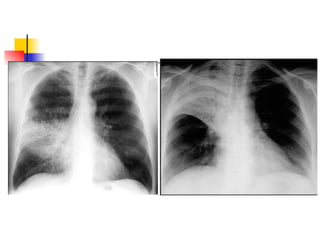
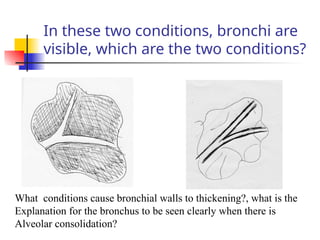
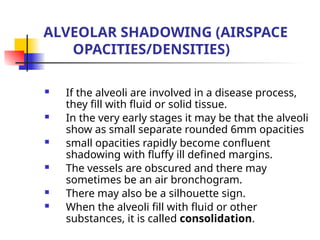
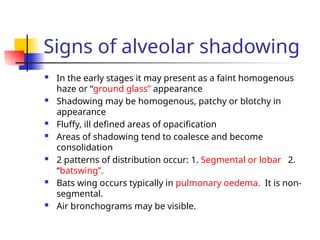
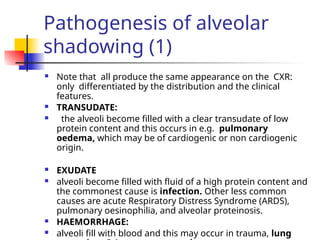
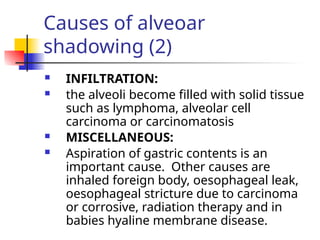
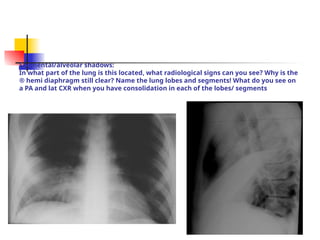
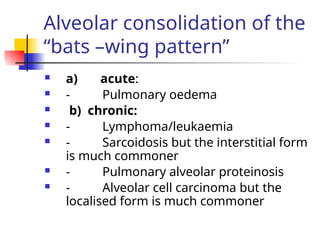
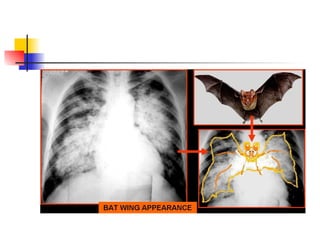
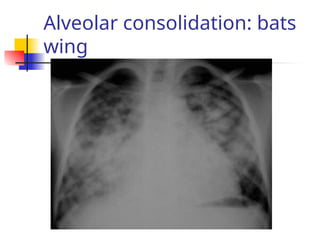
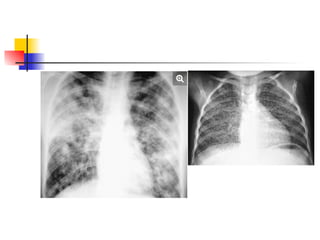
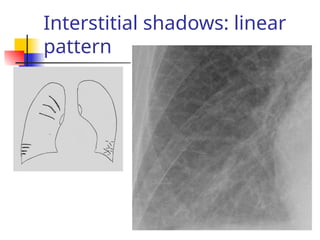
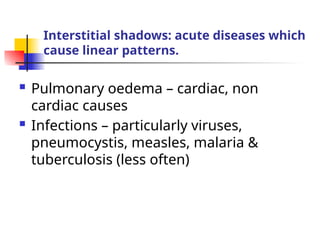
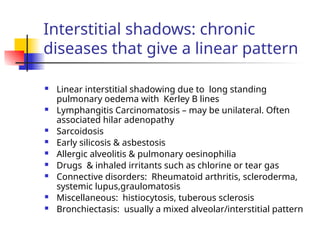
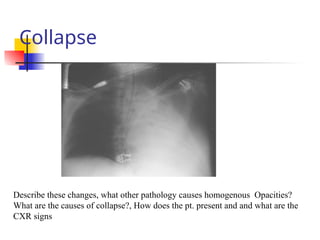
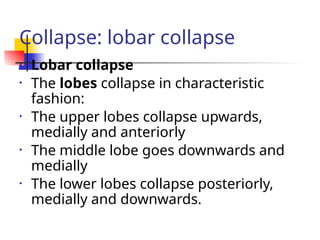
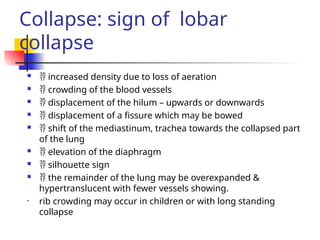
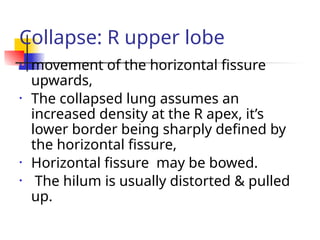
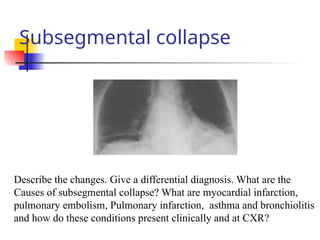
The document outlines various thoracic imaging techniques, including chest X-rays, CT scans, MRIs, and ultrasounds, detailing techniques for obtaining optimal images and identifying various anatomical structures and abnormalities. It emphasizes the importance of proper positioning and exposure to produce quality images, as well as the distinguishing characteristics of normal and abnormal findings. Additionally, it discusses the roles and limitations of advanced imaging modalities in diagnosing conditions such as pulmonary embolism, lung cancer, and other thoracic diseases.