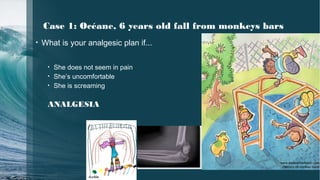
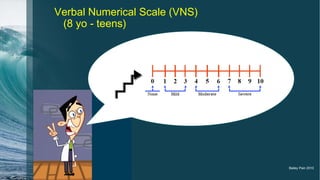
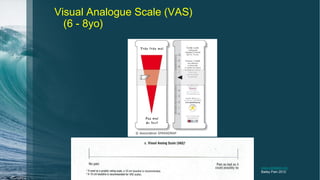
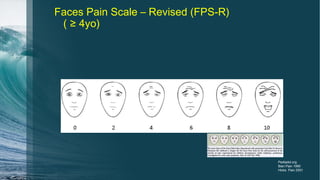
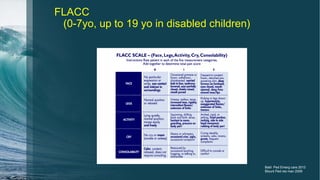
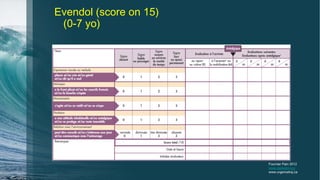
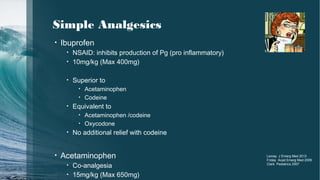
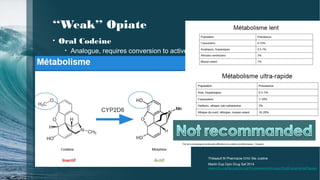
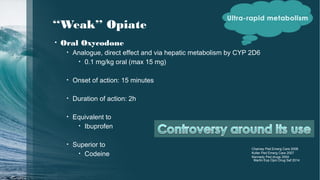
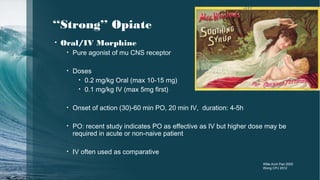
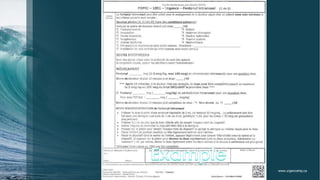
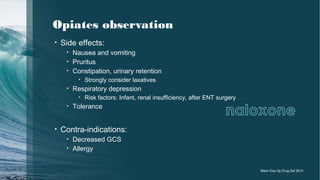
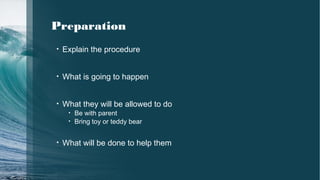
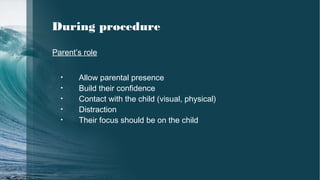
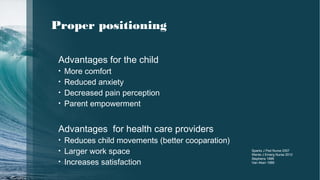
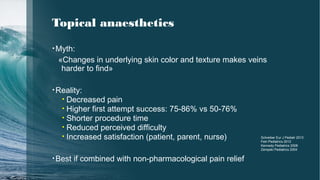
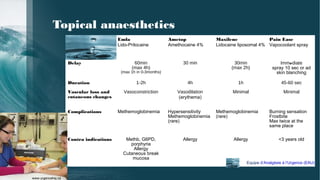
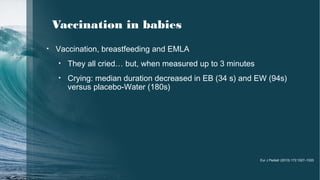
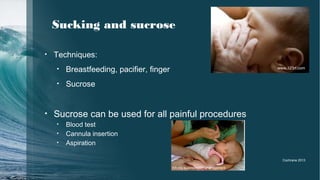
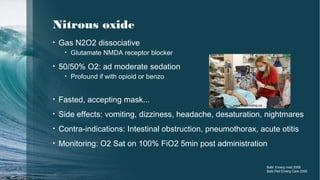
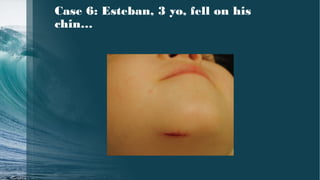
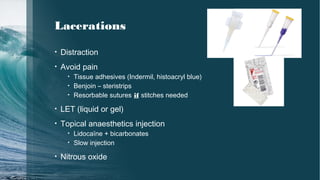
The document discusses pain management strategies for pediatric patients in emergency situations. It provides examples of analgesic plans for different pediatric cases, including a 6-year-old with a fall, a 4-year-old with diabetic ketoacidosis, and a 9-year-old needing immunizations. Non-pharmacological approaches like distraction, positioning, topical anesthetics and sucrose are recommended. Oral and intranasal medications like acetaminophen, ibuprofen, codeine, oxycodone, morphine and nitrous oxide may be used. Proper pain assessment and multimodal analgesia are emphasized.