The document discusses headache disorders, with a focus on migraines, highlighting their prevalence, etiology, and clinical management. It details types of pharmacological and non-pharmacological therapies, their effectiveness, and potential side effects, emphasizing the importance of individualized treatment. Additionally, it outlines the role of various medications, including triptans and beta-adrenergic antagonists, in both acute management and prophylactic therapy for migraine sufferers.
![Introduction [2]
All clinicians should be familiar with:
The various types of headache,
Clinical indicators suggesting the need for urgent medical
attention and
Nonpharmacologic and pharmacologic options for
treatment
The International Headache Society (IHS) classifies
primary headaches as:
Migraine,
Tension-type,
Cluster and Other trigeminal autonomic cephalalgias
2/3/2023
3](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-3-320.jpg)
![Migraine headache [2]
Gender differences in migraine prevalence have been
linked to menustration ,
However, these differences persist beyond menopause.
Prevalence is highest in both men and women between
the ages of 30 and 49 years.
The usual age of onset is 12 to 17 years of age for
females and 5 to 11 years for males.
About 93% of those with migraine reported some
headache-related disability,
2/3/2023
5](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-5-320.jpg)
![Migraine headache [3]
And 54% were severely disabled or needed bed rest
during an attack
A number of neurologic and psychiatric disorders as
well as CVD show increased comorbidity with migraine.
Whether this relationship is causal or representative of
a common pathophysiologic mechanism is unknown.
The economic burden of migraine is substantial;
The indirect costs from work-related disability far
exceed the direct costs associated with treatment.
2/3/2023
6](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-6-320.jpg)
![Migraine headache [4]
Etiology and Pathophysiology
“Vascular hypothesis,” it was thought that focal
neurologic symptoms preceding or accompanying the
headache were caused by vasoconstriction and
reduction in cerebral blood flow.
The headache was thought to be caused by a
compensatory vasodilation with displacement of pain
sensitive intracranial structures.
Although blood flow is decreased during the aura of
migraine, other observations do not support the vascular
hypothesis
2/3/2023
7](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-7-320.jpg)
![Migraine headache [5]
Negative neuroimaging evidence for such vascular
changes and
The effectiveness of medications with no vascular
properties make this contention untenable.
A neuronal etiology has emerged as the leading
mechanism for the development of migraine pain.
More recent evidence suggests that the pain of migraine
is generated centrally
2/3/2023
8](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-8-320.jpg)
![Migraine headache [5]
Which involves episodic dysfunction of neural
structures that control the cranial circulation (the
trigeminovascular system)
This area may represent an endogenous “migraine
generator.”
Sporadic dysfunction of the nociceptive system and the
neural control of cerebral blood flow is hypothesized
These trigger migraine headache via their effects on
the trigeminovascular system
2/3/2023
9](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-9-320.jpg)
![Migraine headache [5]
It is believed that depressed neuronal electrical activity
spreads across the brain,
This produce transitory neural dysfunction.
Headache pain is likely due to compensatory
overactivity in the trigeminovascular system of the brain.
Activation of trigeminal sensory nerves leads to the
release of vasoactive neuropeptides :
Eg, calcitonin gene-related peptide, neurokininA,
substance P
These produce inflammatory response around vascular
structures in the brain, provoking the sensation of pain
2/3/2023
10](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-10-320.jpg)
![Migraine headache [5]
Continued sensitization of CNS sensory neurons can
potentiate and intensify headache pain as an attack
progresses.
Bioamine pathways projecting from the brainstem
regulate activity within the trigeminovascular system.
The pathogenesis of migraine is most likely due to an
imbalance in the modulation of nociception and blood
vessel tone by serotonergic and noradrenergic neurons
2/3/2023
11](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-11-320.jpg)
![Migraine headache [6]
Abnormalities in serotonin (5-HT) activity are also thought to
play a role in migraine headache.
Plasma 5-HT levels decrease by nearly half during a
migraine attack,
And a corresponding rise in the urinary excretion of 5-
hydroxyindoleacetic acid, the primary metabolite of 5-HT.
Also, reserpine, a drug that depletes 5-HT from body stores,
has been found to induce a stereotypical headache in
migraineurs and
It induce a dull discomfort in patients not prone to migraine
2/3/2023
12](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-12-320.jpg)
![Migraine headache [7]
In summary, the pathophysiology of migraine probably
involves dysfunction of the trigeminal neurons that
provide sensory innervation and modulate blood flow to
intracranial blood vessels.
The endogenous stimulus causing this dysfunction may
arise from a “migraine generator” in the brainstem.
Disturbances in 5-HT activity are also probably involved
It is this feature that serves as the target for many
migraine-specific therapies
2/3/2023
13](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-13-320.jpg)
![Migraine headache [8]
Clinical presentation
General
Migraine is a common, recurrent, severe headache that
interferes with normal functioning.
Symptoms
Migraine is characterized by:
Recurring episodes of throbbing head pain,
Frequently unilateral, with gradual onset
when untreated can last from 4 to 72 hours.
2/3/2023
14](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-14-320.jpg)
![Migraine headache [9]
IHS Diagnostic Criteria for Migraine
Migraine without aura
At least five attacks
Headache attack lasts 4-72 hours (untreated or
unsuccessfully treated)
Headache has at least two of the following
characteristics:
Unilateral location
Pulsating quality
Moderate or severe intensity
Aggravation by or avoidance of routine physical activity
2/3/2023
15](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-15-320.jpg)
![Migraine headache [10]
During headache at least one of the following:
Nausea, vomiting, or both
Photophobia and phonophobia
Not attributed to another disorder
Migraine with aura (classic migraine)
At least two attacks
Migraine aura fulfills criteria for typical aura, hemiplegic
migraine, retinal migraine or brainstem aura
Not attributed to another disorder
2/3/2023
16](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-16-320.jpg)

![Migraine headache [11]
Treatment
Desired Outcome
Treat migraine attacks rapidly and consistently without
recurrence
Restore the patient’s ability to function
Minimize the use of backup and rescue medications
Optimize self-care for overall management
Be cost-effective in overall management
Cause minimal or no adverse effects
2/3/2023
18](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-18-320.jpg)
![Migraine headache [12]
Non-pharmacologic therapy of acute migraine
headache is limited but can include:
application of ice to the head and periods of rest or sleep,
usually in a dark, quiet environment.
Preventive management of migraine should begin with the
identification and avoidance of factors that consistently
provoke migraine attacks in
Behavioral interventions, such as relaxation therapy, and
cognitive therapy, are preventive treatment options for
patients who prefer nondrug therapy
2/3/2023
19](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-19-320.jpg)
![Migraine headache [13]
Commonly Reported Triggers of Migraine
Food triggers : Alcohol Caffeine/caffeine withdrawal
Chocolate Fermented and pickled foods
Environmental triggers: Glare or flickering lights
High altitude, Loud noises ,Strong smells and fumes ,Tobacco
smoke
Behavioral–physiologic triggers: Excess or insufficient sleep,
Fatigue, Menstruation, menopause
2/3/2023
20](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-20-320.jpg)
![Migraine headache [14]
Non opiate analgesics
Simple analgesics and NSAIDs are effective
medications for the management of many migraine
attacks
They offer a reasonable first-line choice for
treatment of mild to moderate migraine attacks or
Severe attacks that have been responsive in the past
to similar NSAIDs or nonopiate analgesics.
2/3/2023
21](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-21-320.jpg)
![Migraine headache [15]
Of the NSAIDs, aspirin, ibuprofen, naproxen sodium,
tolfenamic acid, and the combination of acetaminophen plus
aspirin and caffeine have demonstrated the most consistent
evidence of efficacy.
Evidence for other NSAIDs is either limited or inconsistent.
Metoclopramide can speed the absorption of analgesics and
alleviate migraine-related nausea and vomiting.
NSAIDs should be avoided or used cautiously in patients with
previous ulcer disease, renal disease, or hypersensitivity to
aspirin.
Acetaminophen alone is not generally recommended for
migraine because the scientific support is not optimal
2/3/2023
22](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-22-320.jpg)
![Migraine headache [16]
Opiate Analgesics
Narcotic analgesic drugs (e.g., meperidine,
butorphanol, oxycodone, and hydromorphone) are
effective
But generally should be reserved for patients with:
moderate to severe infrequent headaches in whom
conventional therapies are contraindicated
or as "rescue medication" after patients have failed to
respond to conventional therapies.
2/3/2023
23](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-23-320.jpg)
![Migraine headache [17]
Corticosteroids
Can be considered as rescue therapy for status migrainous
Status migrainous is severe, continuous migraine that can
last up to 1 week.
Intravenous or intramuscular dexamethasone at a dose of
10 to 25 mg has also been used as an adjunct to abortive
therapy
2/3/2023
24](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-24-320.jpg)
![Migraine headache [18]
Ergot Alkaloids and Derivatives
Ergotamine tartrate ,dihydroergotamine
Can be considered for the treatment of moderate to
severe migraine attacks
Are nonselective 5-HT1 receptor agonists
Constrict intracranial blood vessels
Then inhibit the development of neurogenic inflammation in
the trigeminovascular system
2/3/2023
25](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-25-320.jpg)
![Migraine headache [19]
Ergotamine tartrate is available for oral, sublingual,
and rectal administration.
Oral and rectal preparations contain caffeine to
enhance absorption and potentiate analgesia.
Ergotamine use is limited because of issues of efficacy
and side effects.
Dihydroergotamine is available for intranasal and
parenteral administration.
Mixing with 1% or 2% lidocaine can reduce burning at
the injection site.
2/3/2023
26](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-26-320.jpg)
![Migraine headache [20]
Nausea and vomiting
Resulting from stimulation of the chemoreceptor trigger zone
Are among most common adverse effects of the ergotamine
derivatives.
Pretreatment with an antiemetic agent should be considered
Other common side effects include:
Abdominal pain, weakness, fatigue, paresthesias,
muscle pain, diarrhea, and chest tightness.
Rarely but severe Side effects:
Symptoms of severe peripheral ischemia (ergotism),
2/3/2023
27](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-27-320.jpg)
![Migraine headache [21]
Ergotamine derivatives are contraindicated in patients:
Renal or hepatic failure;
Coronary, cerebral, or peripheral vascular disease;
Uncontrolled hypertension; and sepsis; and
In pregnant or nursing women
2/3/2023
28](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-28-320.jpg)
![Migraine headache [22]
Serotonin Receptor Agonists (Triptans)
Introduction of the serotonin receptor agonists, or
triptans, represented a significant advance in migraine
pharmacotherapy.
The first member of this class, sumatriptan, and
The second-generation agents zolmitriptan,
naratriptan, rizatriptan, almotriptan, frovatriptan, and
eletriptan
2/3/2023
29](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-29-320.jpg)
![Migraine headache [22]
Are selective agonists of the 5-HT1B and 5-HT1D receptors.
The triptans are appropriate first-line therapy for patients
with mild to severe migraine
And are used for rescue therapy when nonspecific
medications are ineffective.
Selection of a triptan is based on characteristics of the
headache, convenience of dosing,
At all marketed doses, the oral triptans are effective and
well tolerated.
The triptans differ in their pharmacokinetic and
pharmacodynamic profiles
2/3/2023
30](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-30-320.jpg)
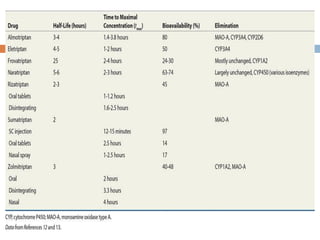
![Migraine headache [23]
In general, triptans can be divided into:
faster onset and higher efficacy and slower onset and low
efficacy
Triptans like frovatriptan and naratriptan have the longest
half lives, the slowest onset of action, and less headache
recurrence.
This may make them more suitable for patients who have
migraine attacks of a slow onset and longer duration
Faster-acting triptans are more efficacious when a rapid
onset is necessary.
Subcutaneous, intranasal, or orally dissolving tablets may be
useful in patients with prominent early nausea or vomiting .
2/3/2023
32](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-32-320.jpg)
![Migraine headache [24]
Side effects to the triptans are common but usually mild
to moderate in nature and of short duration.
Adverse effects are consistent among the class and
include
paresthesias, fatigue, dizziness, flushing,
warm sensations, and somnolence.
One forth of patients receiving a triptan consistently
report “triptan sensations,”
These include: tightness, pressure, heaviness, or pain in
the chest, neck, or throat.
2/3/2023
33](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-33-320.jpg)
![Migraine headache [24]
The triptans are contraindicated in patients with:
History of ischemic heart disease
Uncontrolled hypertension
cerebrovascular disease
hemiplegic and basilar migraine
Should not be used routinely in pregnancy.
The triptans should not be given within 24 hours of the
ergotamine derivatives.
MAOIs use is not recommended with in 2 weeks of triptans
therapy
Concomitant use of SSRI may result in Serotonin syndrome
2/3/2023
34](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-34-320.jpg)
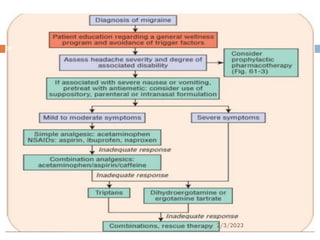
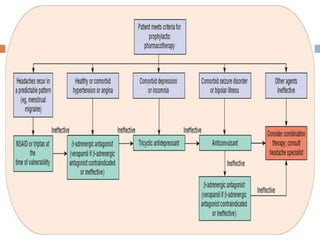
![Migraine headache [25]
Prophylactic drug therapy
Preventive migraine therapies are administered on a
daily basis to reduce the frequency, severity, and
duration of attacks
Preventive therapy should be considered in the setting
of:
Recurring migraines that produce significant disability
despite acute therapy;
Frequent attacks occurring more than twice per week with
the risk of developing medication-overuse headache;
2/3/2023
36](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-36-320.jpg)
![Migraine headache [26]
Symptomatic therapies that are ineffective or
contraindicated, or produce serious side effects
patient preference to limit the number of attacks
Preventive therapy also may be administered preemptively
or intermittently when headaches recur in a predictable
pattern
The evidence to support the various agents used for
migraine prophylaxis has recently been reviewed
2/3/2023
37](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-37-320.jpg)
![Migraine headache [27]
Beta -Adrenergic Antagonists
are among the most widely used drugs for migraine
prophylaxis.
drugs Propranolol, nadolol, timolol, atenolol, and metoprolol
They have proven efficacy in controlled clinical trials,
reducing the frequency of attacks by 50% in 60% to 80% of
patients
Selection of a -blocker can be based on -selectivity,
convenience of the formulation, and tolerability.
Can be considered in healthy or hypertension or angina
comorbidity
Used cautiously in : CHF, PVD, Asthma, DM
2/3/2023
38](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-38-320.jpg)
![Migraine headache [28]
Antidepressants
Amitriptyline, the most widely studied antidepressant for
migraine prophylaxis,
Has demonstrated efficacy in placebo-controlled and
comparative studies.
Use of other antidepressants is based primarily on clinical
and anecdotal experience
Especially in comorbid depression
2/3/2023
39](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-39-320.jpg)
![Migraine headache [29]
Anticonvulsants
Anticonvulsant medications have emerged as important
therapeutic options for migraine prophylaxis with
valproate, divalproex, topiramate, and gabapentin all
demonstrating efficacy.
Anticonvulsants are particularly useful in migraineurs with
comorbid seizures, anxiety disorder, or manic-depressive
illness.
2/3/2023
40](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-40-320.jpg)
![Migraine headache [29]
Nonsteroidal antiinflammatory drugs
Are modestly effective for reducing the frequency, severity, and
duration of migraine attacks,
But potential GI and renal toxicity limit the daily or prolonged use
of these agents.
Consequently, NSAIDs have been used intermittently to prevent
headaches that recur in a predictable pattern, such as menstrual
migraine.
Administration of NSAIDs in the perimenstrual period can be
beneficial in women with true menstrual migraine.
NSAIDs should be initiated up to 1 week prior to the expected
onset of headache and continued for no more than 10 days.
2/3/2023
41](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-41-320.jpg)
![Migraine headache [30]
Calcium Channel Blockers
The calcium channel blockers generally are considered
second or third-line options for preventive treatment
Used when other drugs with established clinical benefit are
ineffective or contraindicated.
Verapamil is the most widely used calcium channel blocker
for preventive treatment,
2/3/2023
42](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-42-320.jpg)

![Tension–type headache [2]
Pathophysiology
The mechanism of pain in CTT headache is thought to
originate from myofascial factors and peripheral
sensitization of nociceptors.
Central mechanisms also are involved, with heightened
sensitivity of pain pathways in the CNS
The following may be initiating stimulus:
Mental stress, nonphysiologic motor stress,
a local myofascial release of irritants, or a combination of
these
2/3/2023
45](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-45-320.jpg)
![Tension–type headache [3]
Following activation of supraspinal pain perception
structures, a self-limiting headache results in most
individuals
CTT headache can evolve from ETT headache in
predisposed individuals due to a change in central
circuits and nociceptors
It is likely that other pathophysiologic mechanisms also
contribute to the development of tension-type headache
2/3/2023
46](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-46-320.jpg)
![Tension–type headache [4]
Clinical Presentation
The pain usually is mild to moderate in intensity
Often is described as a dull, nonpulsatile tightness or
pressure.
Bilateral pain is most common, but the location can vary
The pain is classically described as having a "hatband"
pattern.
Associated symptoms generally are absent, but mild
photophobia or phonophobia may be reported.
The disability associated with tension-type headache
typically is minor
2/3/2023
47](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-47-320.jpg)
![Tension–type headache [5]
Treatment
General Approach to Treatment
The vast majority of episodic tension-type headache
sufferers self-medicate with OTC medications
Simple analgesics and NSAIDs are the mainstay of acute
therapy.
Most agents used for tension-type headache have not been
studied in controlled clinical trials
2/3/2023
48](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-48-320.jpg)
![Tension–type headache [6]
Nonpharmacologic Therapy
Psychophysiologic therapy and physical therapy have
been used in the management of tension-type
headache.
Behavioral therapies can consist of reassurance and
counseling, stress management, relaxation training,
and biofeedback.
These therapies (alone or in combination) can result in
a 35% to 50% reduction in headache activity.
2/3/2023
49](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-49-320.jpg)
![Tension–type headache [7]
Pharmacologic Therapy
Simple analgesics (alone or in combination with caffeine) and
NSAIDs are effective for the acute treatment of most mild to
moderate tension-type headaches.
the following have demonstrated efficacy in placebo
controlled and comparative studies.
Acetaminophen, Aspirin,
Ibuprofen, naproxen,
ketoprofen, and ketorolac
2/3/2023
50](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-50-320.jpg)
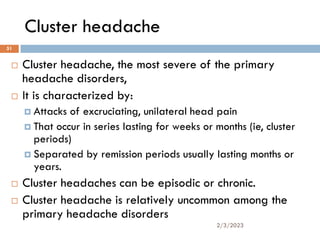
![Cluster headache [2]
The male-to-female ratio for cluster headache is
approximately 4:1
Age of onset typically in the third to fifth decade.
Up to 85% of patients with cluster headache are
tobacco smokers or have a history of smoking.
Tobacco cessation does not, however, seem to improve
the course of cluster headaches.
Recent genetic epidemiologic surveys support a
predisposition for cluster headache can exist in certain
families. 2/3/2023
52](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-52-320.jpg)
![Cluster headache [3]
Cluster headache is one of a group of disorders
referred to as trigeminal autonomic cephalalgias.
This autonomic nervous system dysfunction is
characterized by SNS underactivity coupled with PNS
activation
The pain is believed to be the result of vasoactive
neuropeptide release and neurogenic inflammation.
The exact cause of trigeminal activation in this
intermittently manifest syndrome is unclear
2/3/2023
53](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-53-320.jpg)
![Cluster headache [4]
Hypothalamic dysfunction, occasioned by diurnal or
seasonal changes in neurohumoral balance, may
responsible for headache periodicity
Serotonin affects neuronal activity and may play a role
in the pathophysiology of cluster headache.
The precipitation of cluster headache by high-altitude
exposure also implicates hypoxemia in the pathogenesis
Hypothalamus-regulated changes in cortisol, prolactin,
testosterone, growth hormone, leuteinizing hormone,
endorphin, and melatonin have been found during
periods of cluster headache attack.
2/3/2023
54](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-54-320.jpg)
![Cluster headache [5]
Neuroimaging studies performed during acute cluster
headache attacks have demonstrated activation of the
ipsilateral hypothalamic gray area,
Implicating the thalamus as a cluster generator.
Significant cranial autonomic activation occurs
ipsilateral to the pain
2/3/2023
55](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-55-320.jpg)
![Cluster headache [6]
Patients experiencing “cluster headache” may display
the following headache symptoms and characteristics:
At least one or more of the following symptoms:
Lacrimation
Nasal congestion and/or rhinorrhea
Eyelid edema
Forehead or facial sweating/flushing
Sensation of fullness in the ear
Miosis and/or ptosis
Or a sense of restlessness or agitation
2/3/2023
56](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-56-320.jpg)
![Cluster headache [7]
Duration of pain: 15–180 minutes (untreated)
Frequency of attacks: One every other day and/or
up to 8 per day for more than half the time the
disorder is active
Criteria for diagnosis: Five or more attacks
fulfilling the above criteria
2/3/2023
57](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-57-320.jpg)
![Cluster headache [8]
Treatment
As in migraine, therapy for cluster headaches involves
both abortive and prophylactic therapy.
Abortive therapy is directed at managing the acute
attack.
Prophylactic therapies are started early in the cluster
period in an attempt to induce remission.
Patients with chronic cluster headache can require
prophylactic medications indefinitely
2/3/2023
58](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-58-320.jpg)
![Cluster headache [9]
Abortive Therapy
Oxygen
The standard acute treatment of cluster headache is
inhalation of 100% oxygen by non breather facial mask at
a rate of 7 to 10 L/min for 15 to 30 minutes.
Repeat administration can be necessary because of
recurrence, as oxygen appears to merely delay, rather than
abort, the attack in some patients.
No side effects have been reported with the use of oxygen,
but caution should be used for those who smoke or have
COPD
2/3/2023
59](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-59-320.jpg)
![Cluster headache [10]
Ergotamine Derivatives
All forms of ergotamine have been used in cluster
headaches,
But no controlled clinical trials support their use.
In clinical use, intravenous dihydroergotamine results in the
quickest response,
Repeated administration for 3 to 7 days can break the cycle
of frequent attacks.
2/3/2023
60](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-60-320.jpg)
![Cluster headache [11]
Ergotamine tartrate also has provided effective relief
of cluster headache attacks when administered
sublingually or rectally,
But the pharmacokinetics of these preparations
frequently limit their clinical utility.
Dosing guidelines are similar to those for migraine
headache therapy
2/3/2023
61](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-61-320.jpg)
![Cluster headache [12]
Triptans
The quick onset of subcutaneous and intranasal triptans make
them safe and effective abortive agents for cluster
headaches
Subcutaneous Sumatriptan (6 mg) is the most effective agent.
Nasal sprays are less effective but may be better tolerated
in Some patients.
Adverse events reported in cluster headache patients are
similar to those seen in migraineurs.
Orally administered triptans have limited use in cluster
attacks because of their relatively slow onset of action;
2/3/2023
62](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-62-320.jpg)
![Cluster headache [13]
Prophylactic Therapy
Verapamil, the preferred calcium channel blocker for the
prevention of cluster headaches,
It is effective in approximately 70% of patients.
The beneficial effects of verapamil often appear after 1
week of therapy.
A typical suggested dosage range is from 360 to 720
mg/day,
Some patients requiring up to 1,200 mg/day.
2/3/2023
63](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-63-320.jpg)
![Cluster headache [13]
Lithium
Lithium carbonate is effective for episodic and chronic
cluster headache attacks
Can also be used in combination with verapamil.
A positive response is seen in
Up to 78% of patients with chronic cluster headache,
And in up to 63% of patients with episodic cluster
headache.
The usual dose is 600 to 1,200 mg/day, with a
suggested starting dose of 300 mg twice daily..
2/3/2023
64](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-64-320.jpg)
![Cluster headache [14]
Initial side effects are mild and include :
Tremor, lethargy,
Nausea, Diarrhea, and
Abdominal discomfort.
Thyroid and renal function must be monitored during
lithium therapy
2/3/2023
65](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-65-320.jpg)
![Cluster headache [15]
Ergotamine
Is efficacious for prophylactic as well as abortive therapy of
cluster headaches.
A 2-mg bedtime dose is often for the prevention of nocturnal
headache attacks.
Daily use of 1 to 2 mg ergotamine alone or in combination
with verapamil or lithium
Can provide effective headache prophylaxis in patients
refractory to other agents
Risk of ergotism or rebound headache little with this regimen
2/3/2023
66](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-66-320.jpg)
![Cluster headache [16]
Corticosteroids are useful for inducing remission.
Therapy is initiated with 40 to 60 mg/day prednisone
and tapered over approximately 3 weeks.
Relief appears within 1 to 2 days of initiating therapy.
To avoid steroid-induced complications, long-term use
is not recommended.
Headaches can recur when therapy is tapered or
discontinued
2/3/2023
67](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-67-320.jpg)
![Therapeutic outcome evaluation [2]
Patients using acute therapies should be monitored to
identify potential medication-overuse headache.
Patient counseling is necessary to allow for proper
medication use
Strict adherence to dosing guidelines should be stressed
to minimize potential toxicity.
Patterns of abortive medication use can be documented
to establish the need for prophylactic therapy.
Prophylactic therapies also should be monitored closely
(every 3-6 months until stable) 2/3/2023
69](https://image.slidesharecdn.com/headachedisordersmubarik-241005224720-e4dfaf1b/85/Headache-Disorders-used-for-all-pharmacy-student-69-320.jpg)