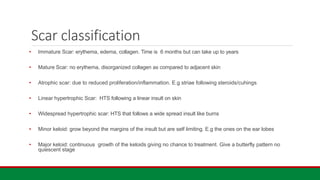
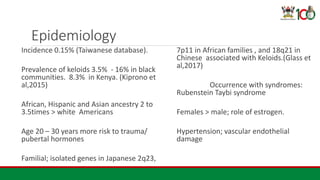
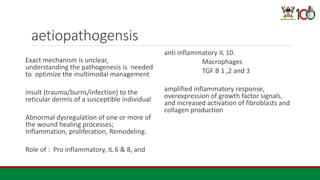
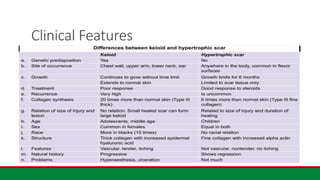
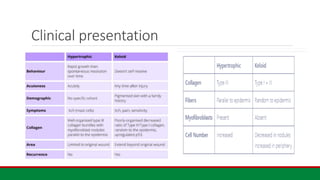
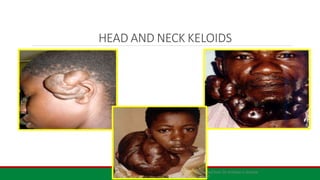
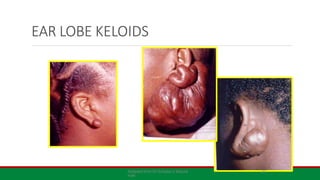
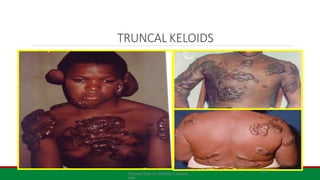
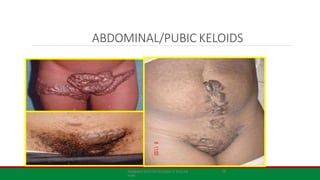
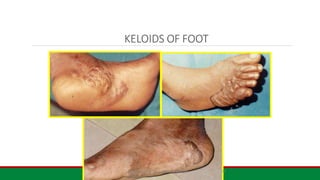
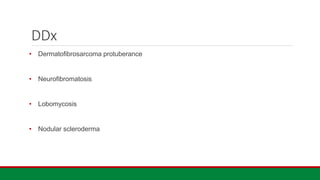
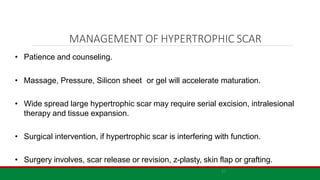
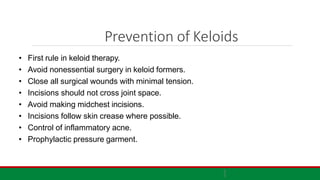
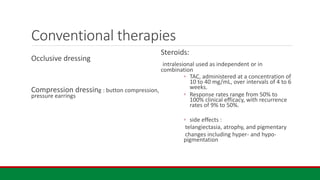
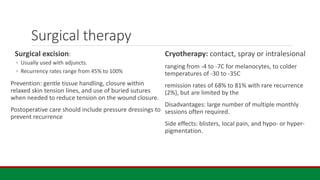
The document provides an overview of keloids and hypertrophic scars, detailing their definitions, epidemiology, aetiology, clinical presentations, and management options. Keloids are defined as scars that extend beyond the original injury site, while hypertrophic scars remain within the boundaries and may be treated using various multimodal approaches. The text emphasizes the importance of understanding risk factors and treatment strategies to prevent and manage these fibroproliferative disorders effectively.






![References
1. Kassi, Komenan et al. “Quality of life in black African patients with keloid
scars.” Dermatology reports vol. 12,2 8312. 22 Oct. 2020, doi:10.4081/dr.2020.8312
2. Davis, Scott A et al. “Management of keloids in the United States, 1990-2009: an analysis
of the National Ambulatory Medical Care Survey.” Dermatologic surgery : official publication
for American Society for Dermatologic Surgery [et al.] vol. 39,7 (2013): 988-94.
doi:10.1111/dsu.12182
3. Glass, Donald A 2nd. “Current Understanding of the Genetic Causes of Keloid
Formation.” The journal of investigative dermatology. Symposium proceedings vol. 18,2
(2017): S50-S53. doi:10.1016/j.jisp.2016.10.024](https://image.slidesharecdn.com/kelloidsandhts-240704081242-69b7fc86/85/keloids-and-Hypertrophic-Scars-Presentation-and-management-options-29-320.jpg)