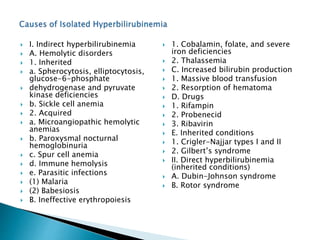
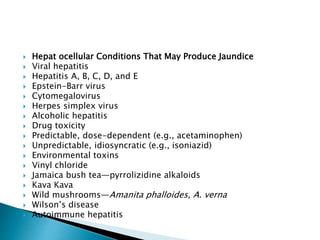
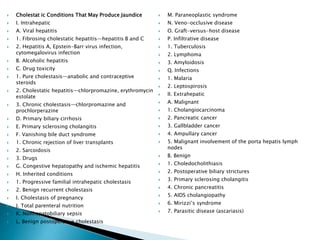
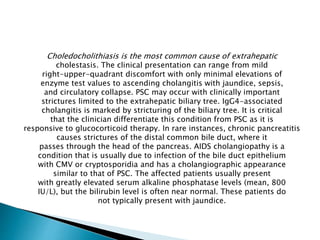
This document summarizes jaundice and hyperbilirubinemia. It describes how jaundice results from the deposition of bilirubin in tissues due to high bilirubin levels in the blood. Bilirubin levels can be estimated by examining the skin and mucous membranes for a yellow color. Higher bilirubin levels result in darker urine. The document then discusses the production, metabolism, and excretion of bilirubin, how liver disease or other issues can cause hyperbilirubinemia, and how to evaluate patients with jaundice.

![Laboratory Tests A battery of tests are helpful in the
initial evaluation
of a patient with unexplained jaundice. These include
total and
direct serum bilirubin measurement with fractionation;
determination
of serum aminotransferase, alkaline phosphatase, and
albumin
concentrations; and prothrombin time tests. Enzyme
tests (alanine
aminotransferase [ALT], aspartate aminotransferase
[AST], and
alkaline phosphatase [ALP]) are helpful in
differentiating between
a hepatocellular process and a cholestatic processA](https://image.slidesharecdn.com/jaundice-200530210420/85/Jaundice-23-320.jpg)