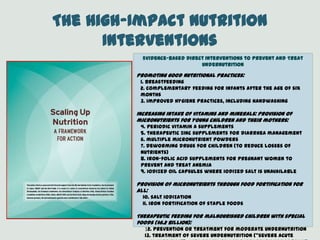
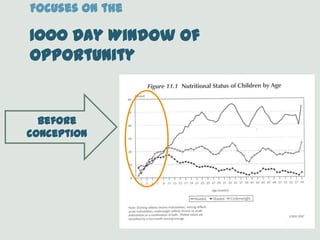
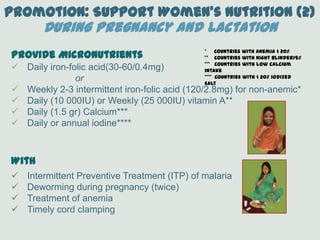
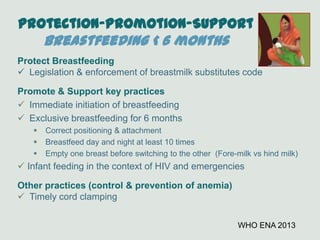
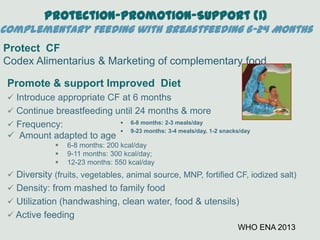
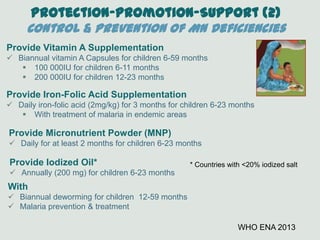
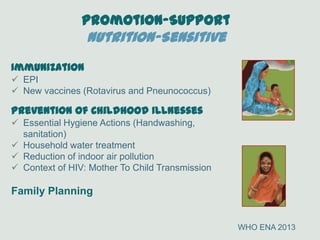
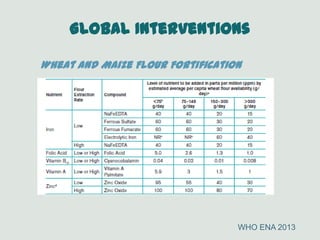
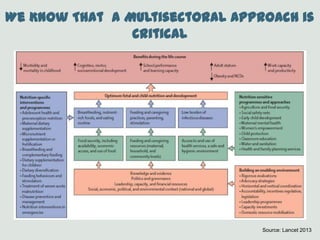
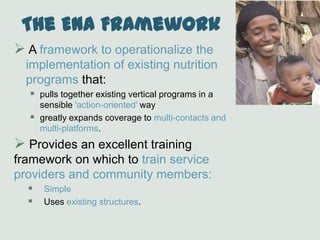
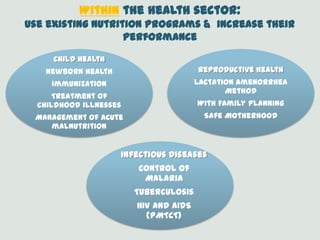
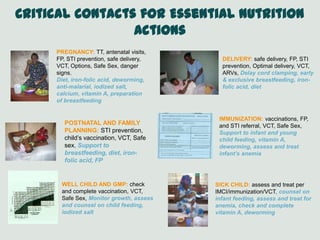
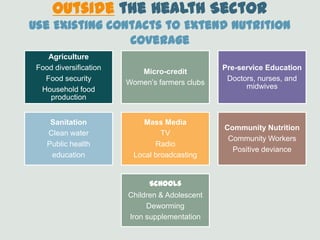
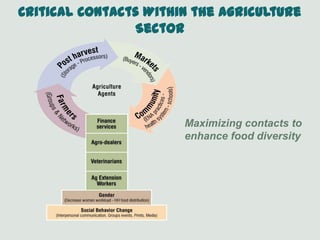
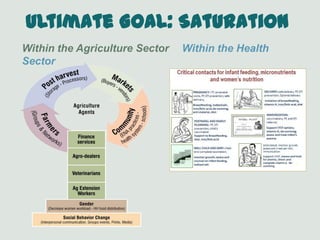
The ENA Framework provides guidance for implementing high-impact nutrition interventions at scale. It is based on interventions with proven impact in women's nutrition, infant and young child feeding, and micronutrients. The framework takes a life cycle approach, focusing on the 1000 day window of opportunity from conception to a child's second birthday. It outlines 13 evidence-based direct nutrition interventions to prevent and treat undernutrition, organized by promotion of good practices, increasing intake of vitamins and minerals, and therapeutic feeding for malnourished children. The ENA framework leverages multiple sectors like health, agriculture, education, and media to maximize coverage of essential nutrition actions through existing community contacts.