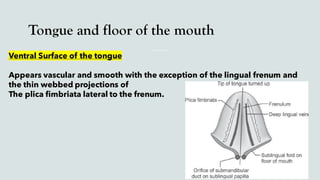
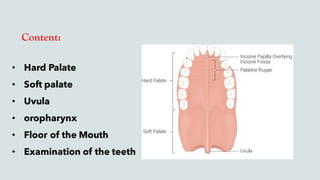
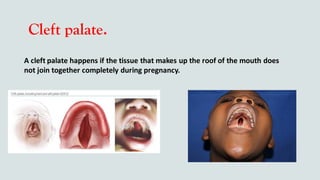
This document provides guidance on performing an intra-oral examination. It discusses examining different areas of the mouth including the lips, labial mucosa, buccal mucosa, buccal vestibule, tongue, hard palate, soft palate, uvula, oropharynx, floor of the mouth, and teeth. Common lesions, abnormalities, and examination techniques are described for each area. The document also provides details on evaluating the dental pulp through tests like heat, cold, and electrical pulp testing as well as using transillumination to examine for cracked teeth.