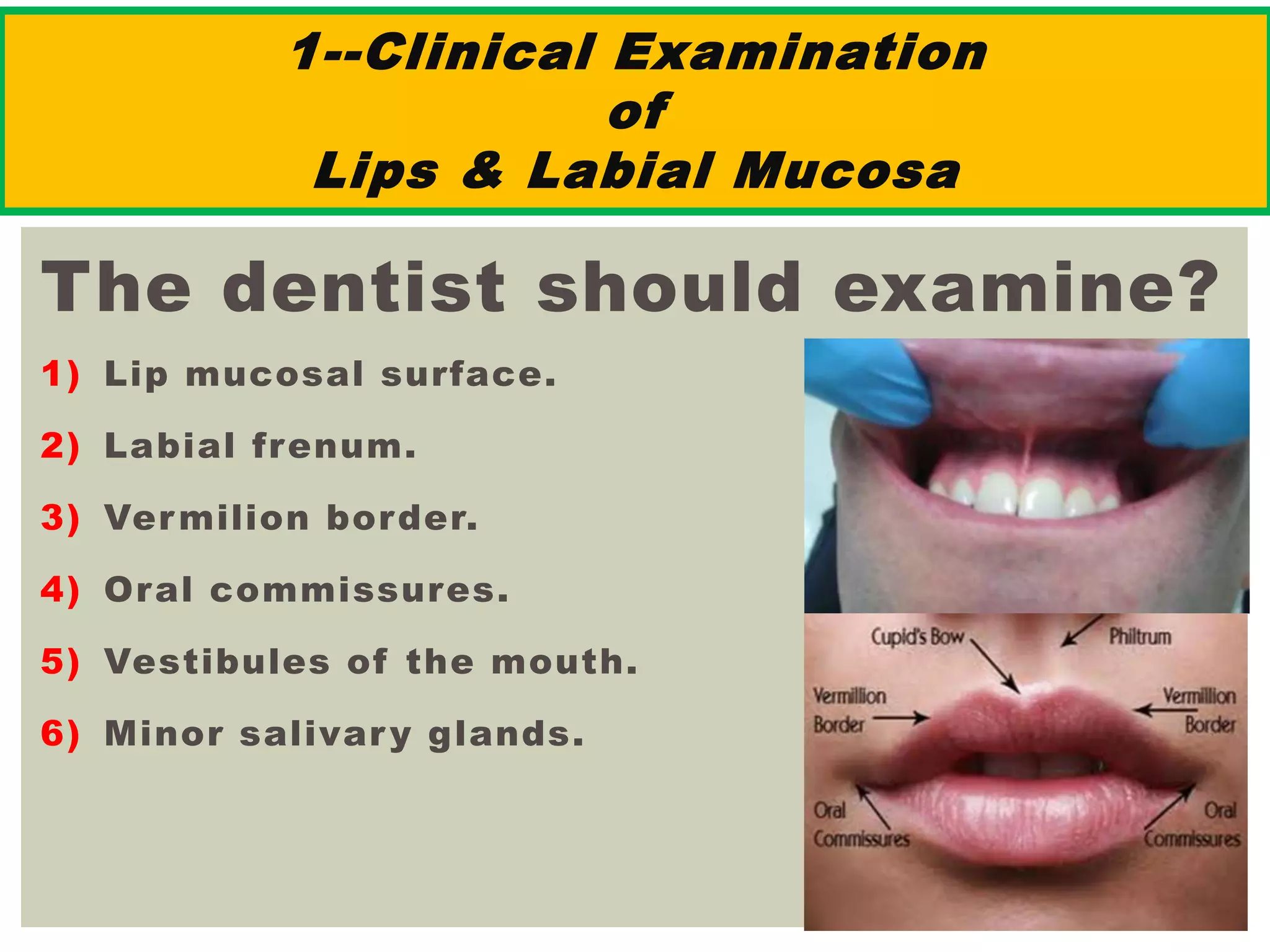
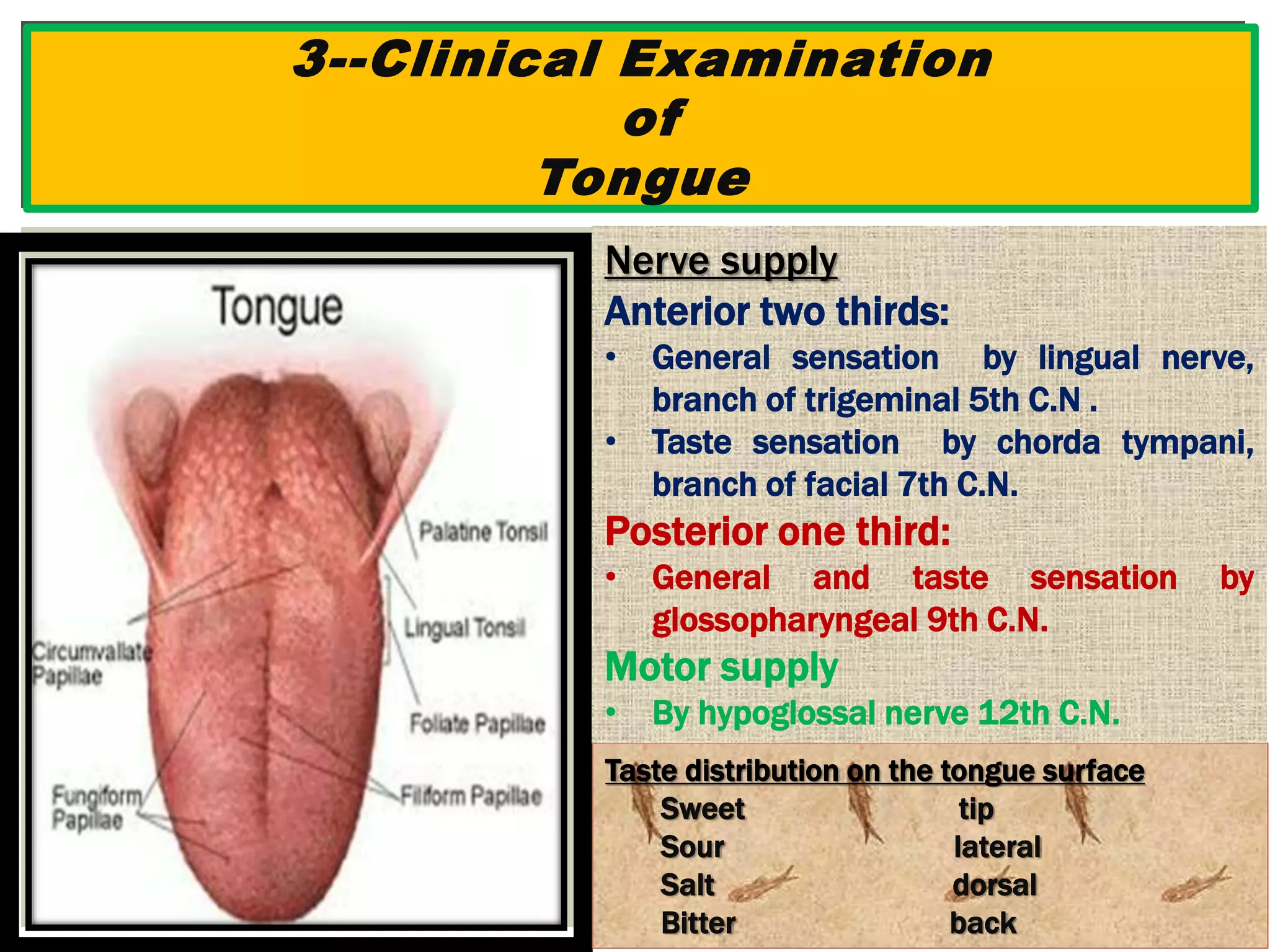
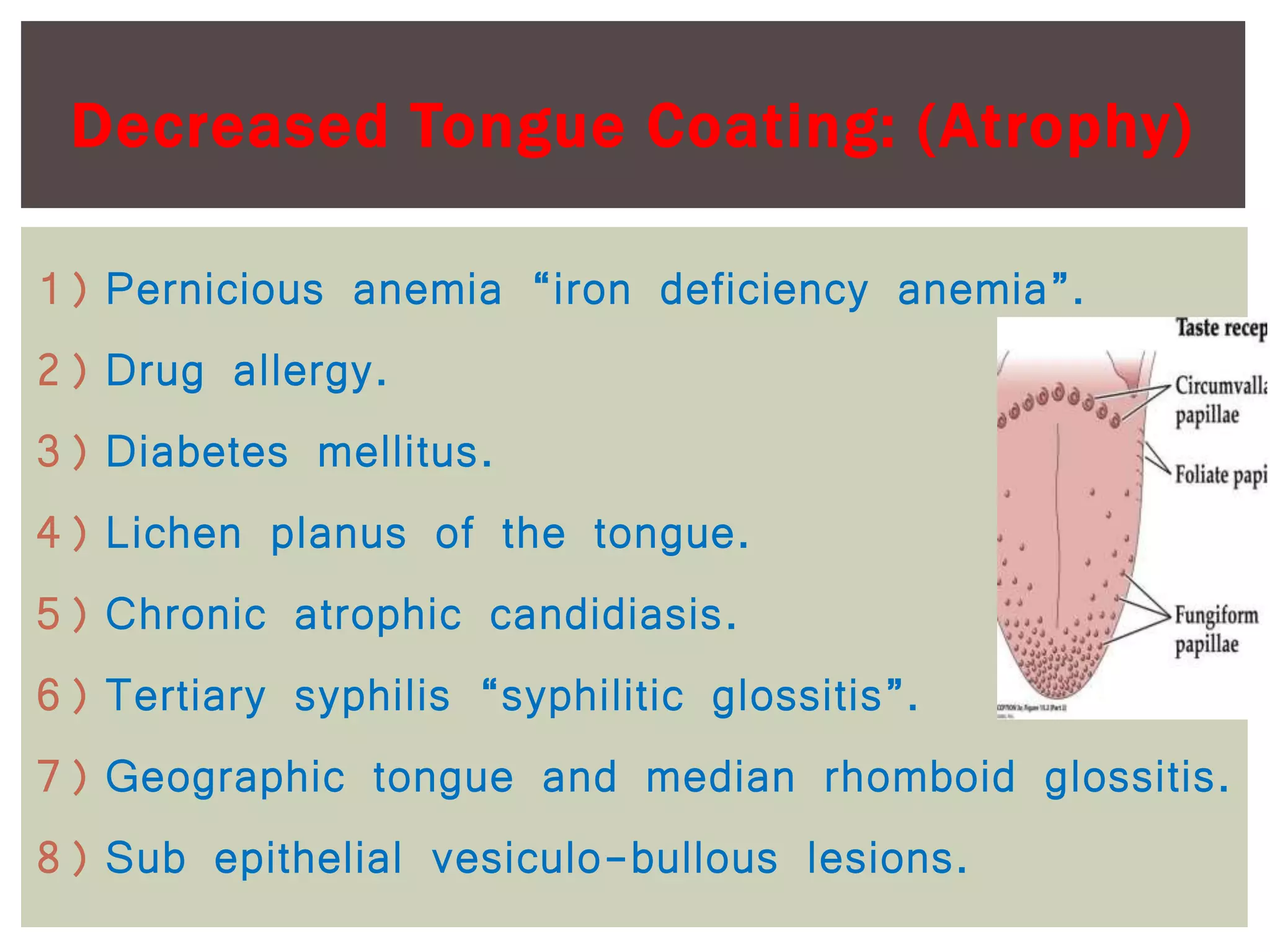
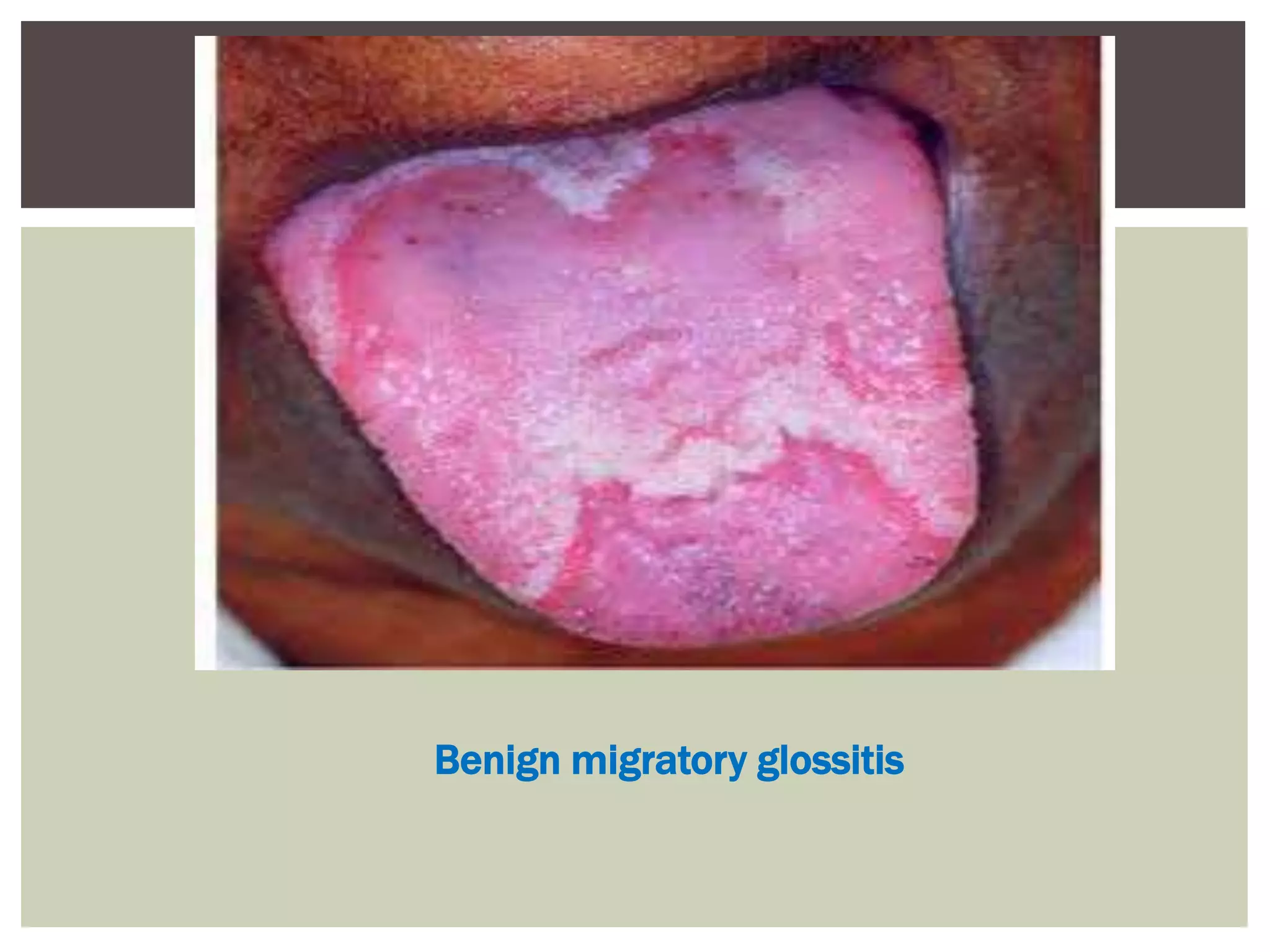
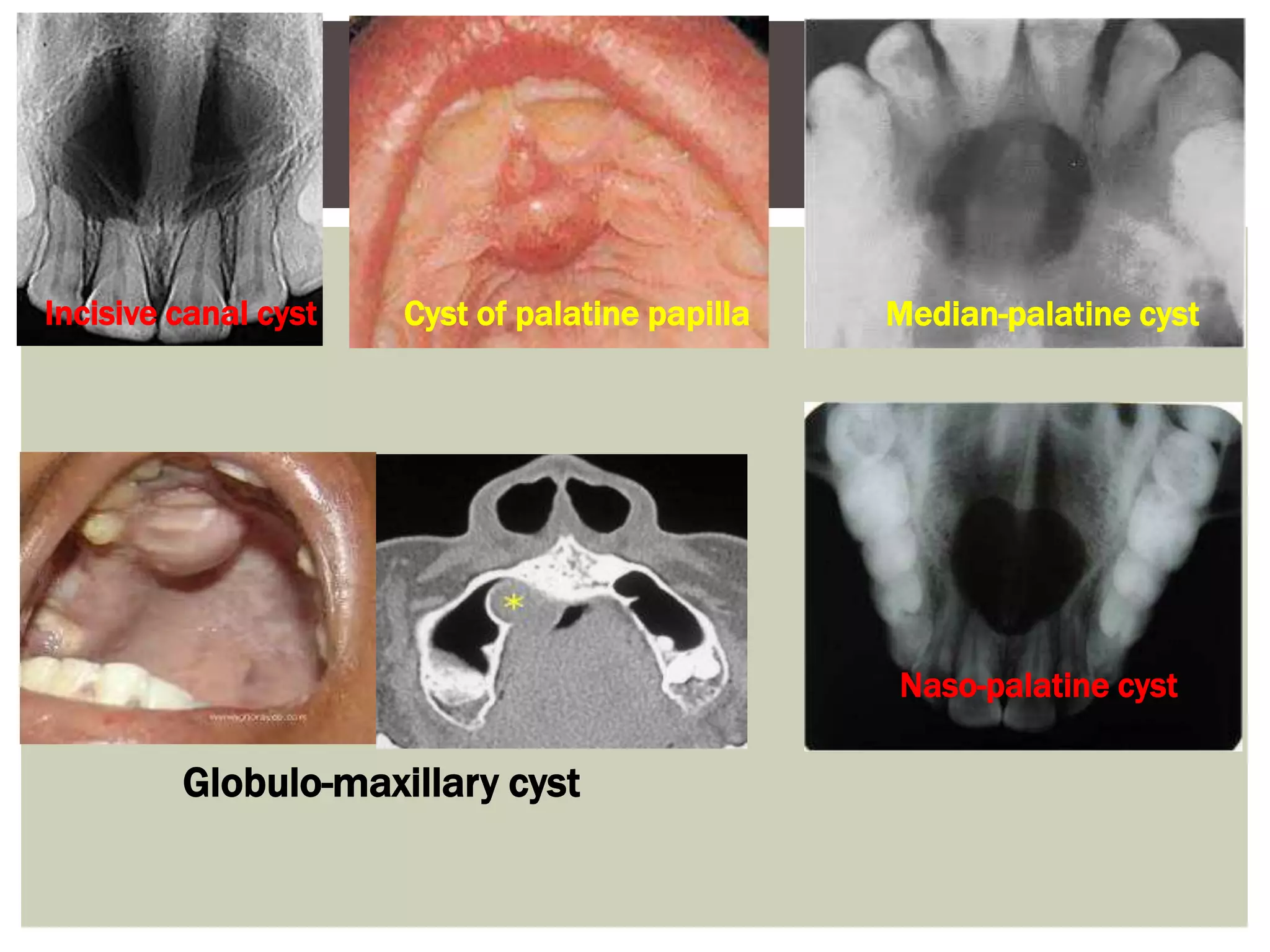
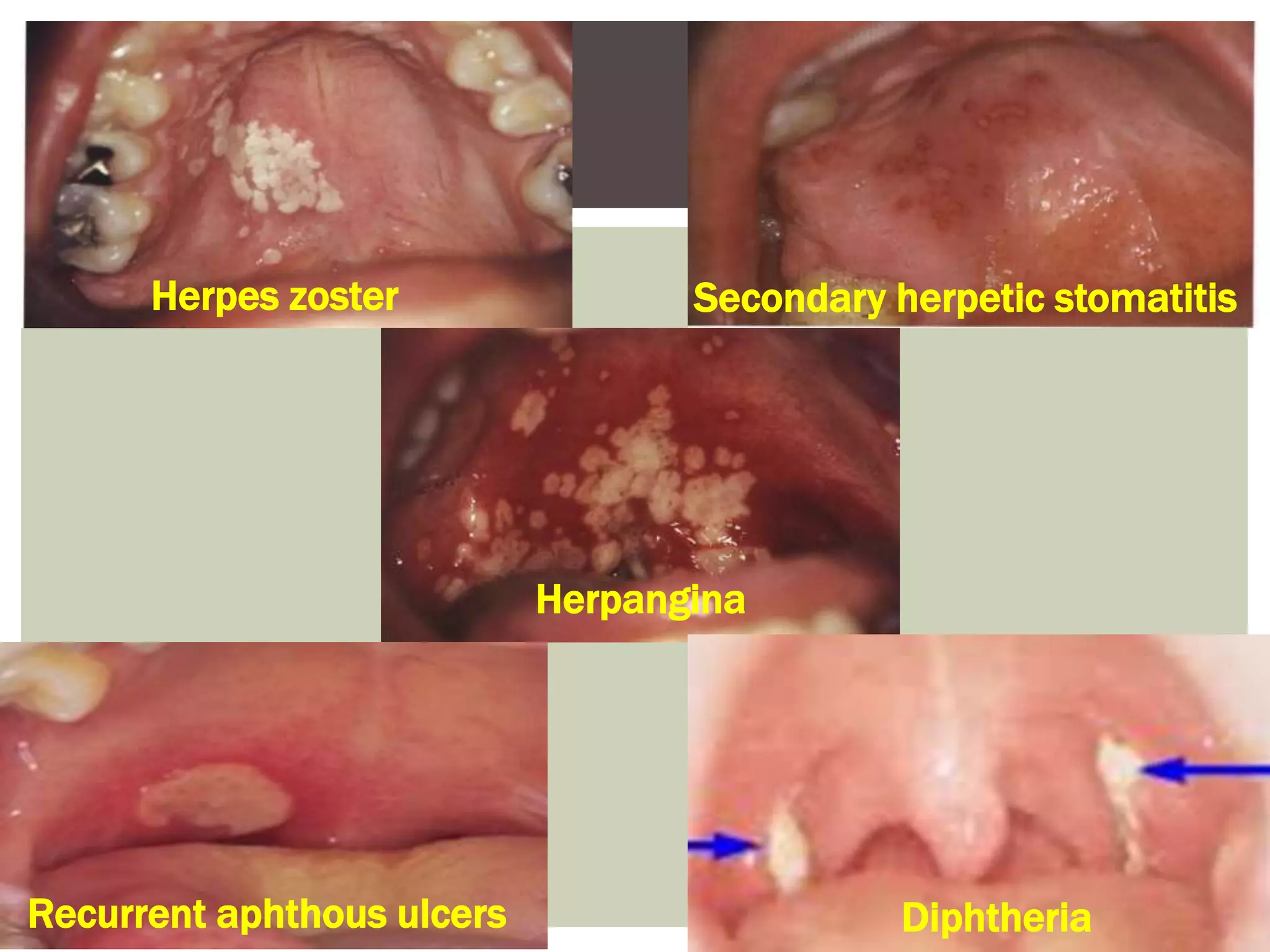
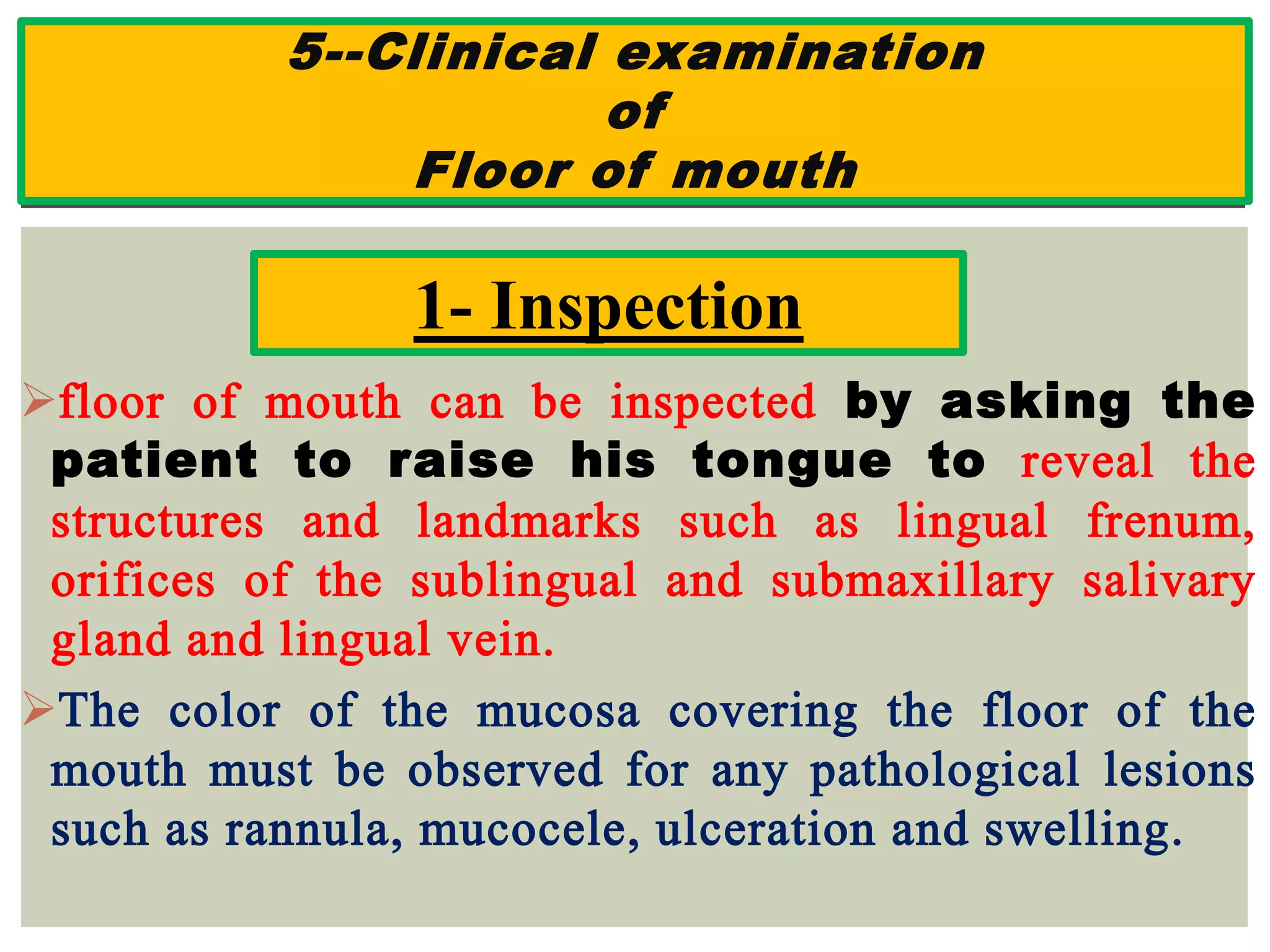
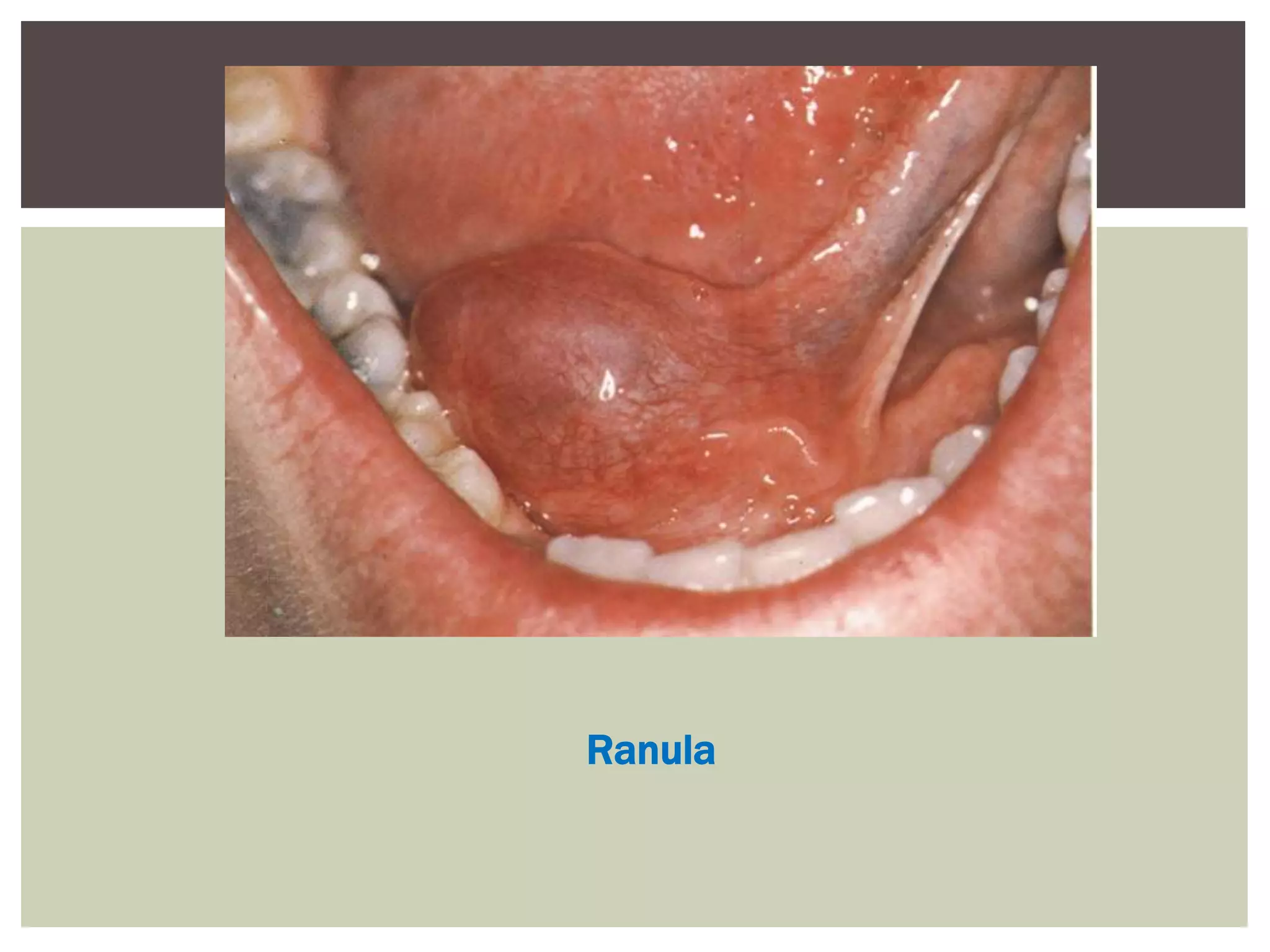
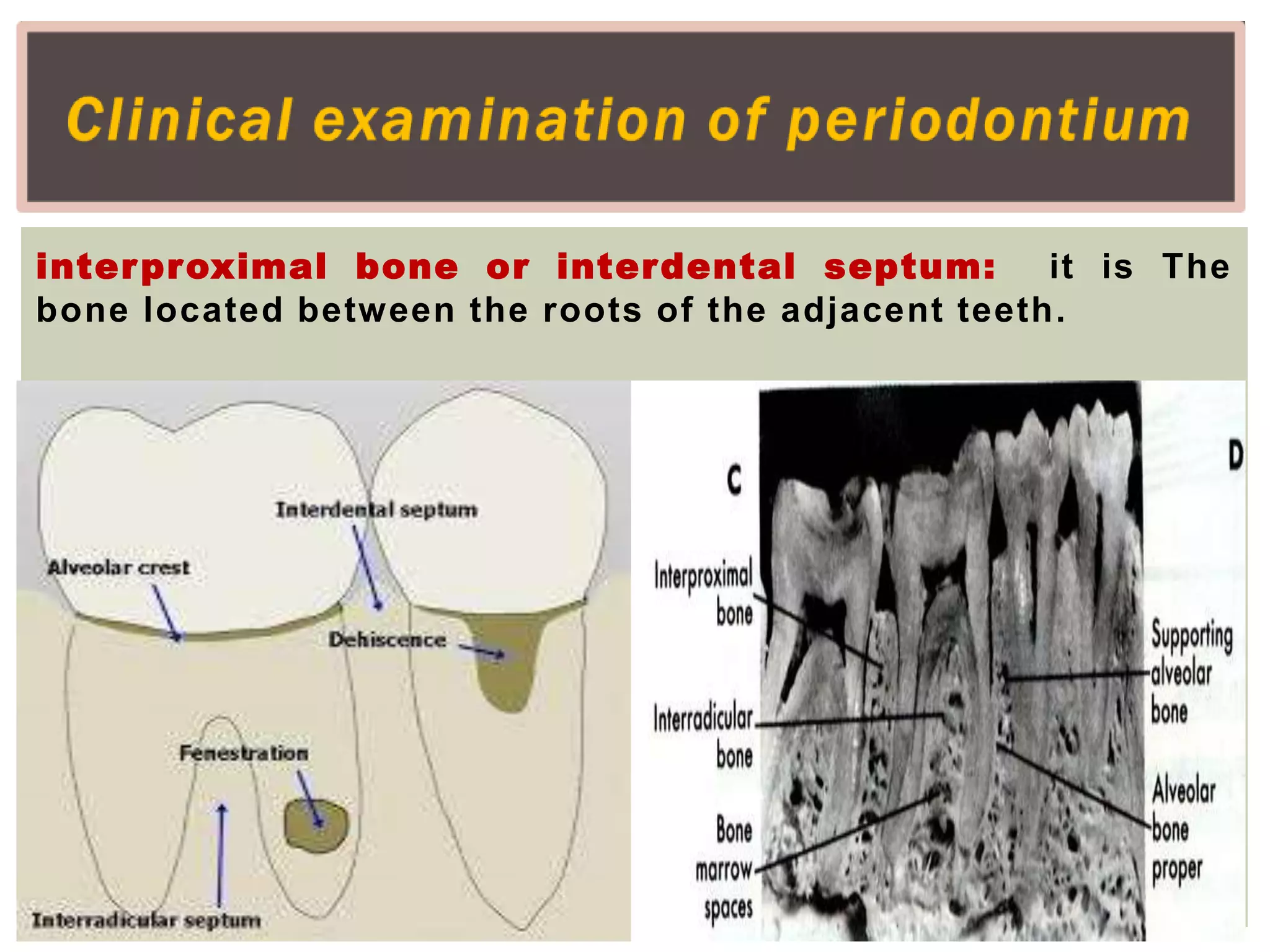
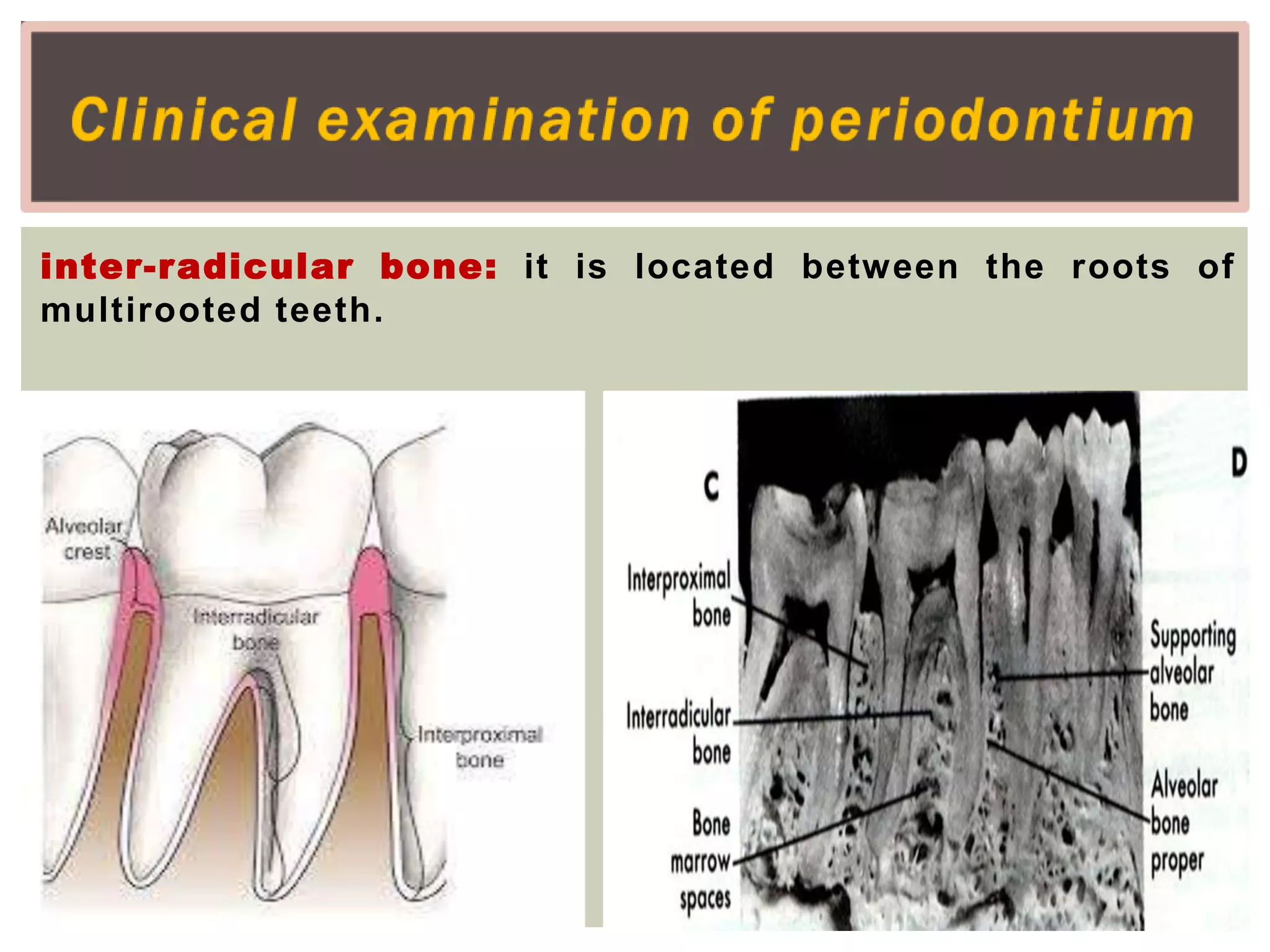
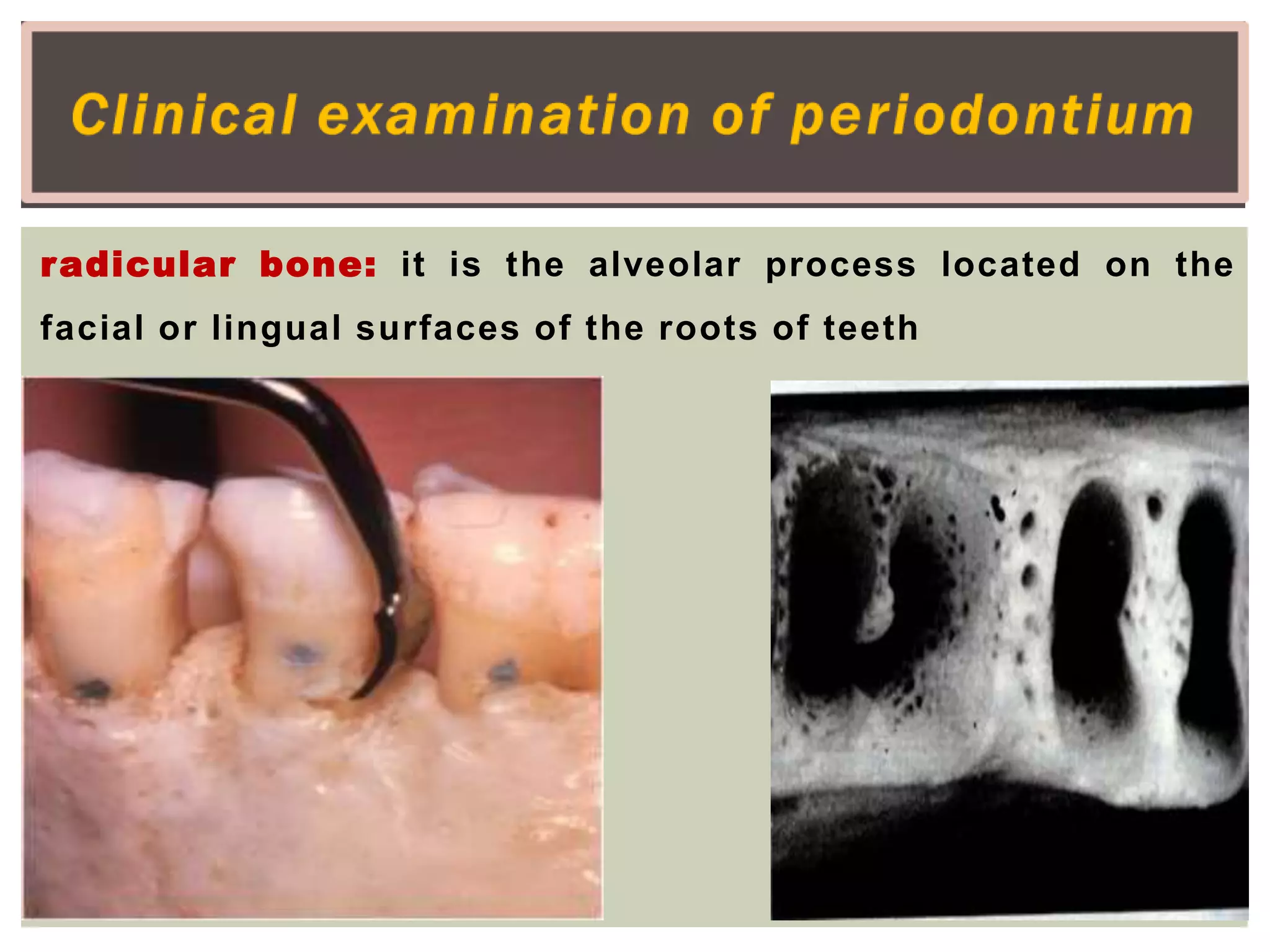
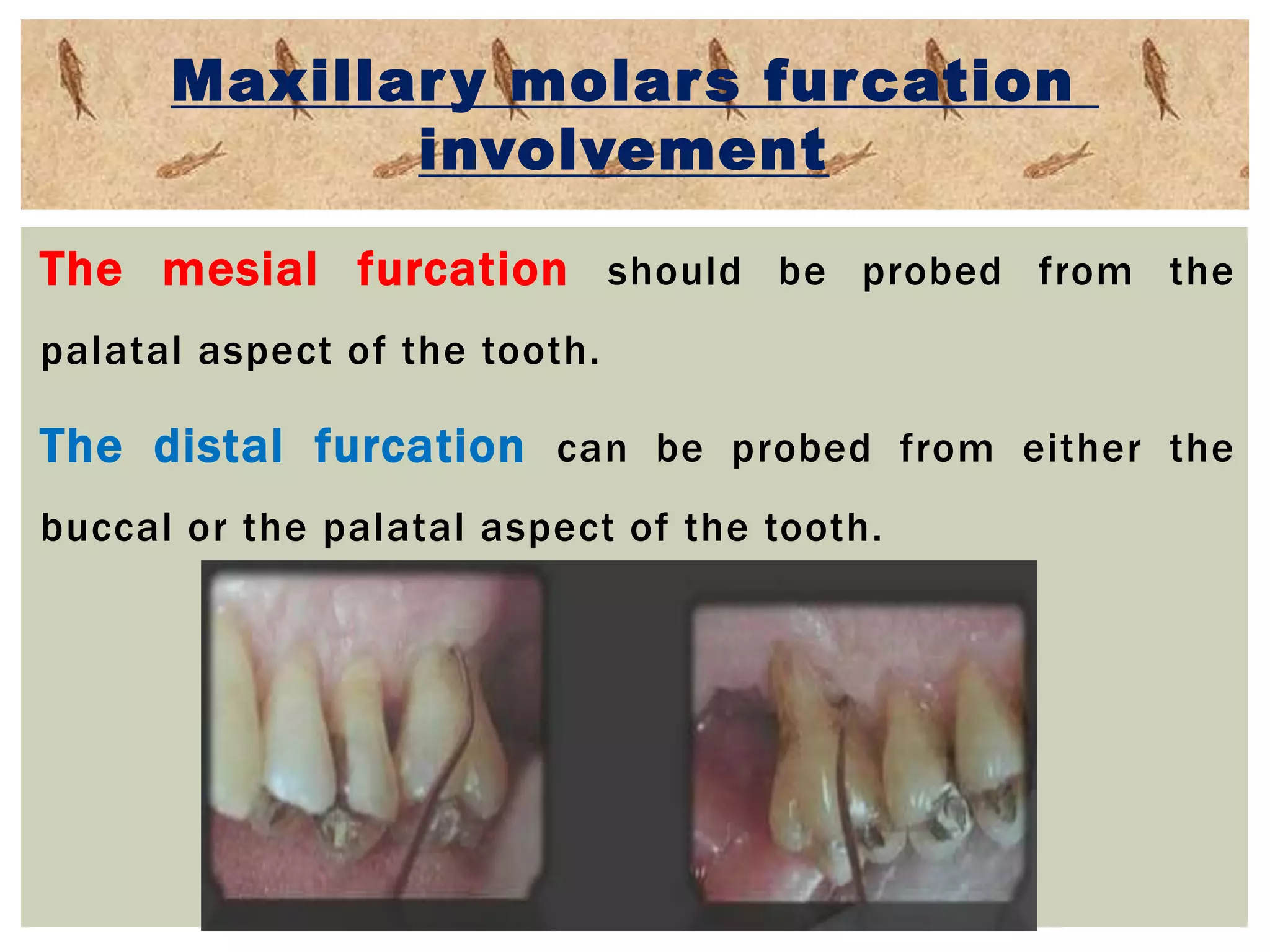
This document provides guidance on performing an intraoral examination. It discusses examining the lips, labial mucosa, buccal mucosa, tongue, hard palate, soft palate, floor of mouth, and periodontium. For each structure, it describes the clinical examination steps of inspection and palpation to identify any abnormalities, lesions, or signs of disease. Common pathological conditions are also listed for each intraoral site. The document emphasizes performing a thorough intraoral soft tissue and periodontal examination to diagnose any oral diseases or issues.