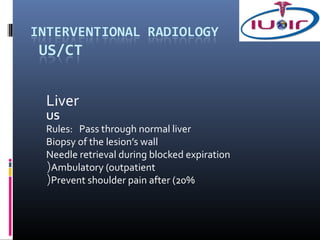
The document discusses biopsy and drainage procedures. It provides details on:
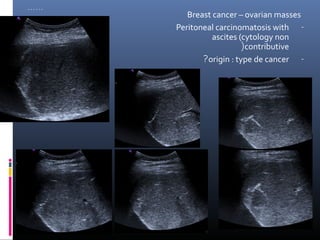
1) Biopsy results being positive 70-100% of the time, with the lowest success for lymphoma.
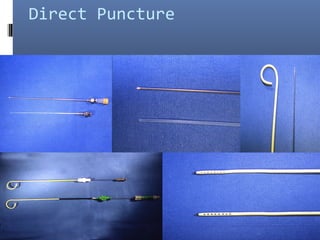
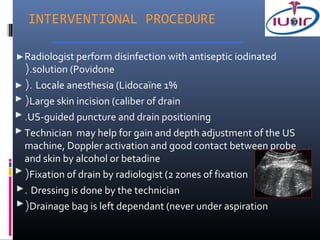
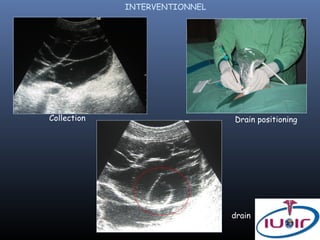
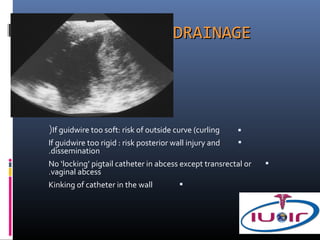
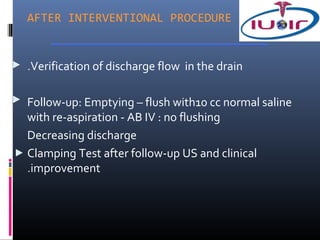
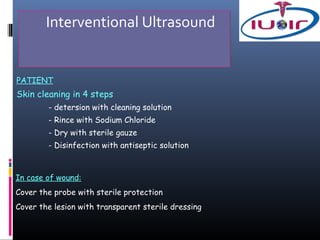
2) Techniques for abdominal drainage including direct puncture and the Seldinger technique using various sterile materials.
3) Precautions for drainage including using a fine needle to determine fluid characteristics and never fully emptying before draining.