1. Biopsy results have a positive diagnosis rate between 70-100%. Performance is least for lymphoma biopsies.
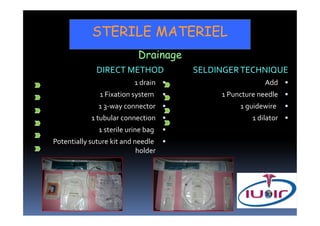
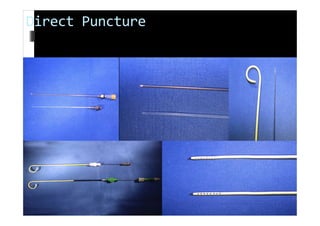
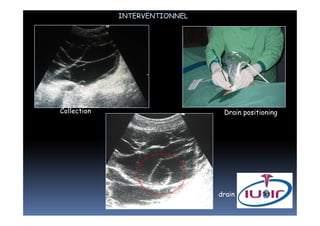
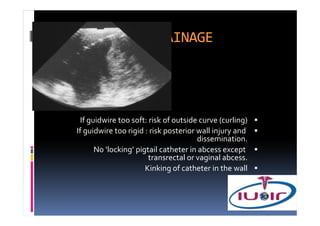
2. Abdominal drainage procedures can be performed via direct puncture or the Seldinger technique using sterile materials including drains, fixation systems, and drainage bags.
3. After drainage procedures, the drain output is checked and patients are monitored for improvement before conducting clamping tests if drainage decreases and removing the drain. Follow up involves emptying and flushing the drain with saline.