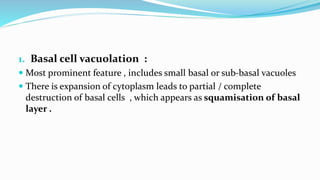
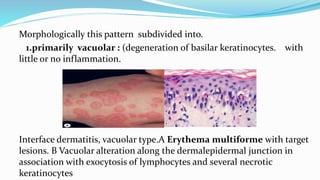
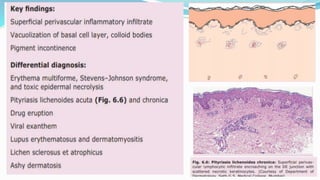
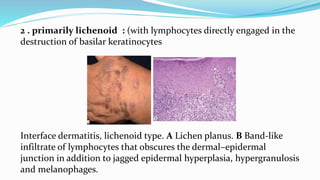
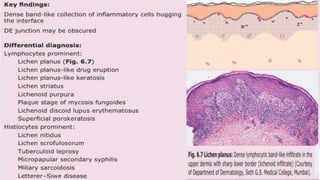
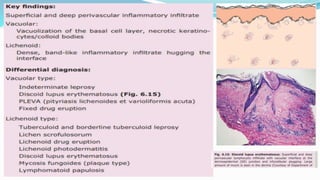
This document defines and describes interface dermatitis. It notes that interface dermatitis involves inflammation along the dermoepidermal junction associated with vacuolation of basal keratinocytes. The key morphological changes include basal cell vacuolation, apoptotic keratinocytes, obscuring of the dermoepidermal junction, various epidermal changes, and papillary dermal changes. Interface dermatitis can be subdivided into a primarily vacuolar type with little inflammation or a primarily lichenoid type with lymphocytes directly destroying basal keratinocytes.