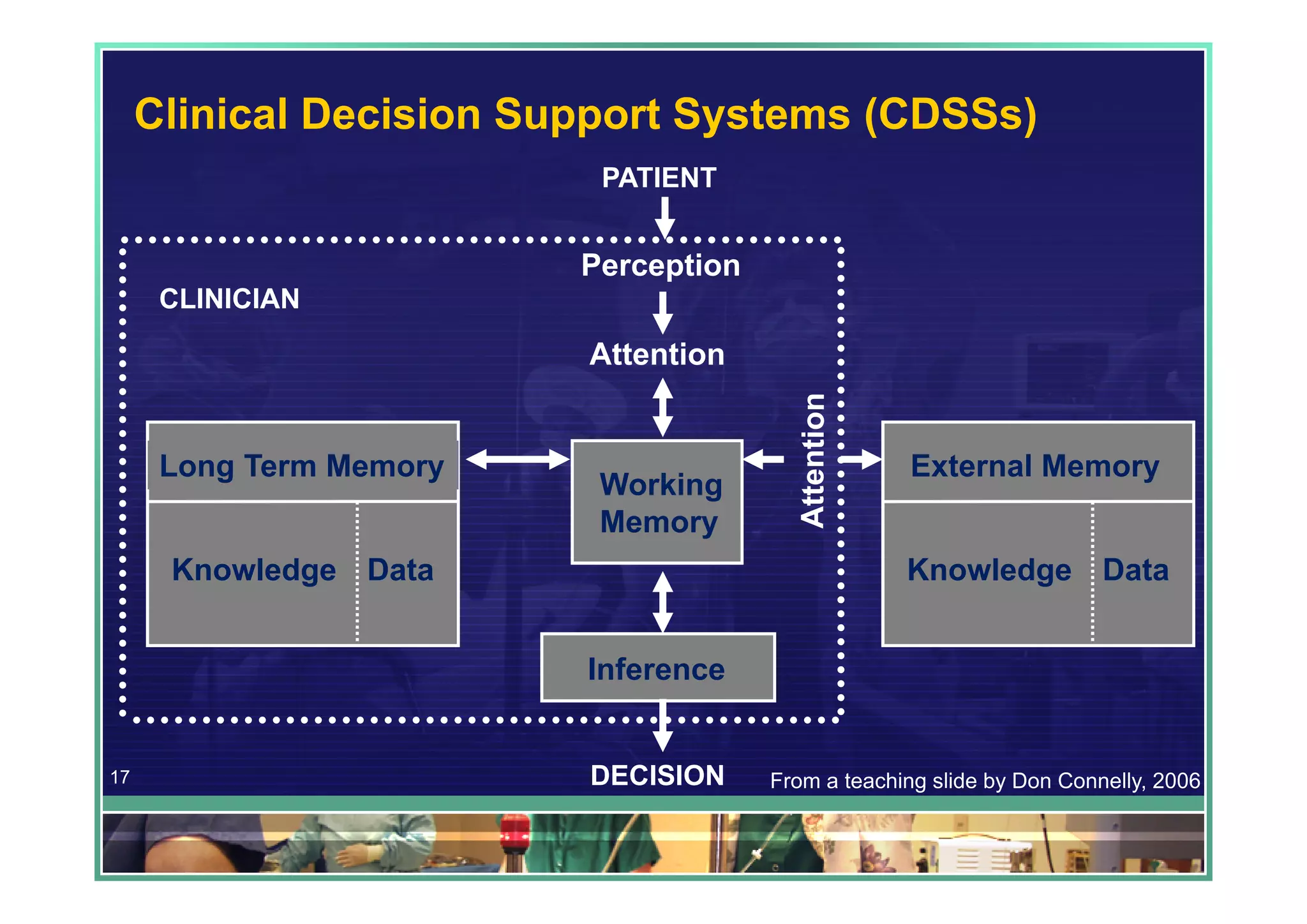
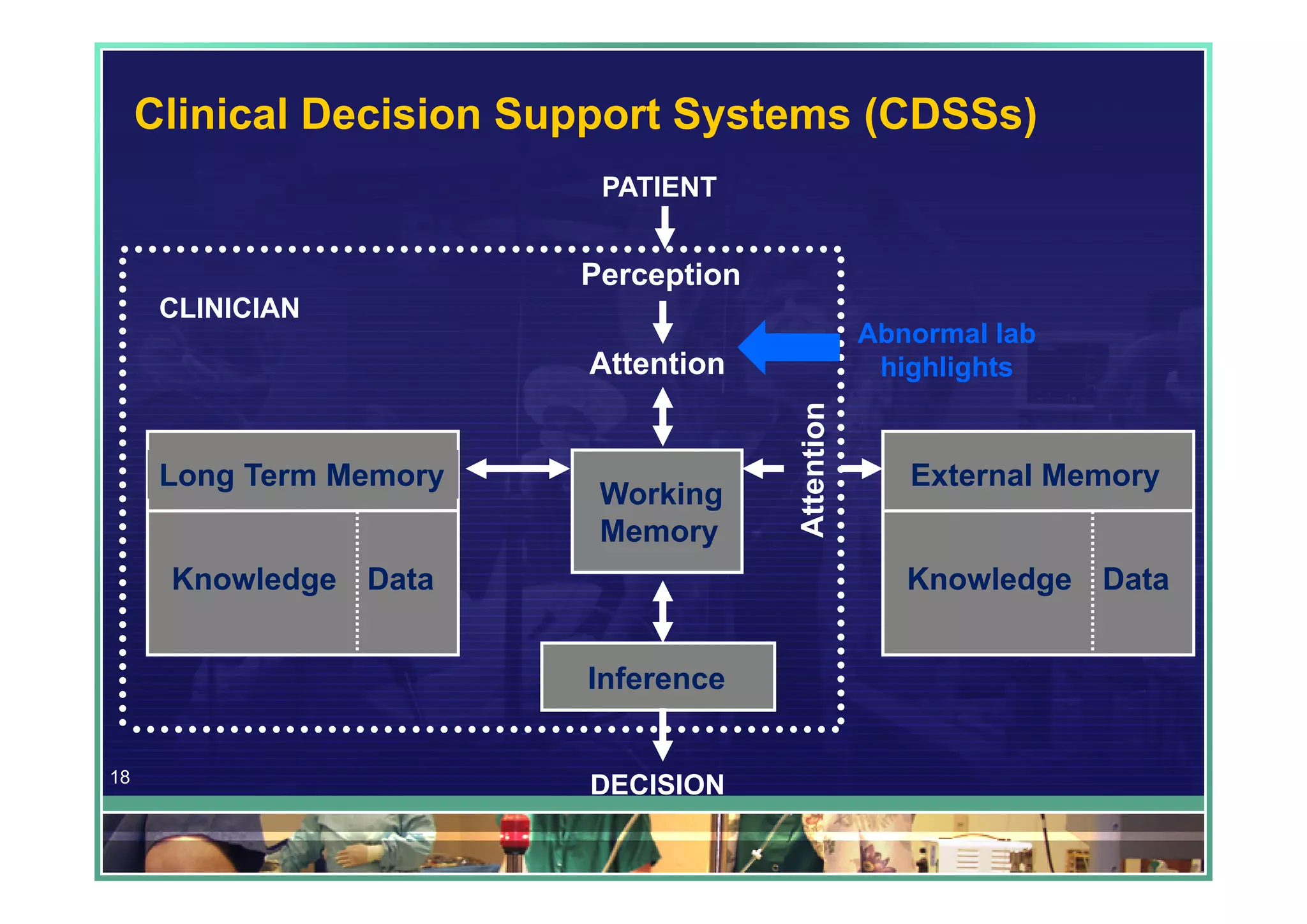
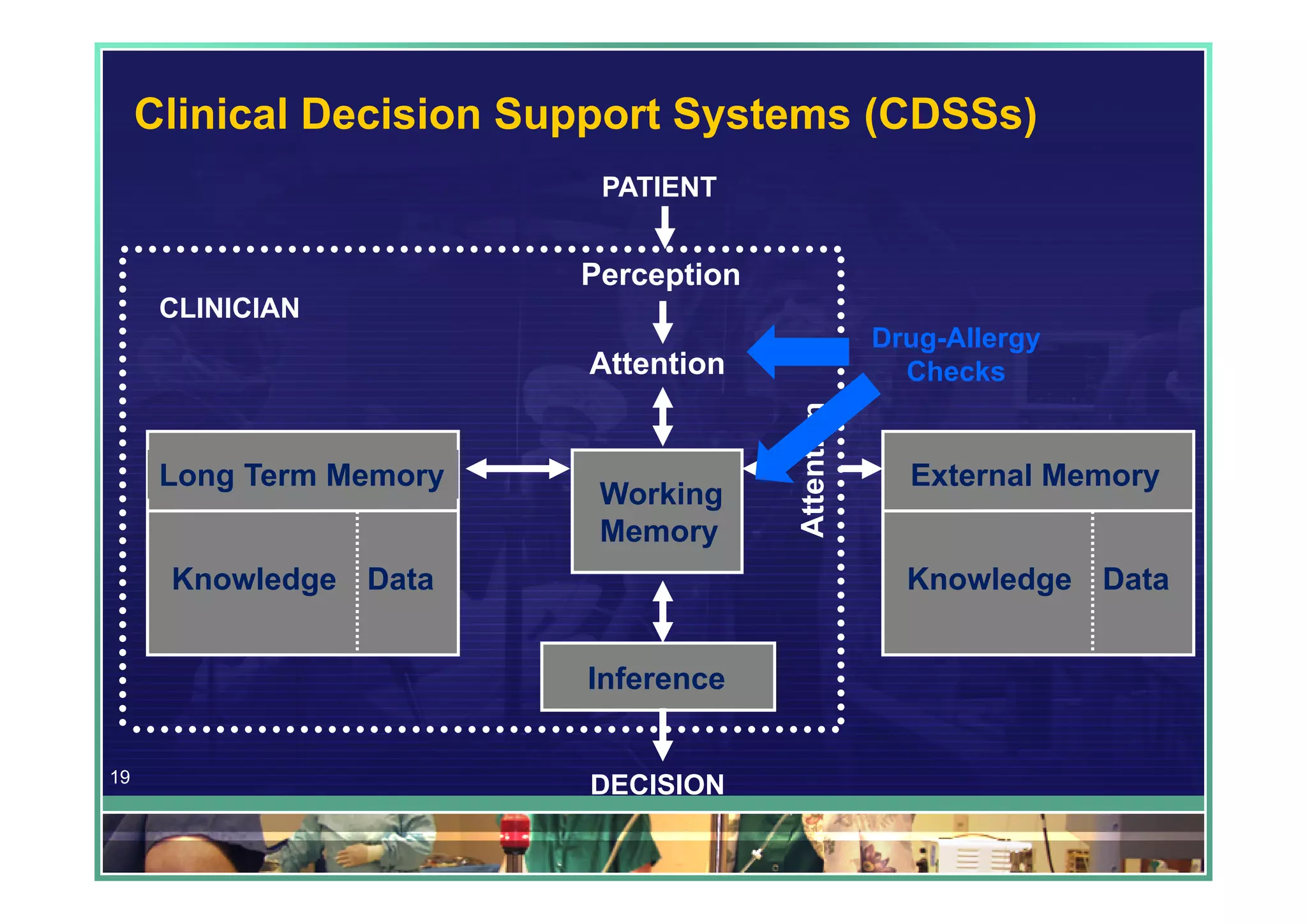
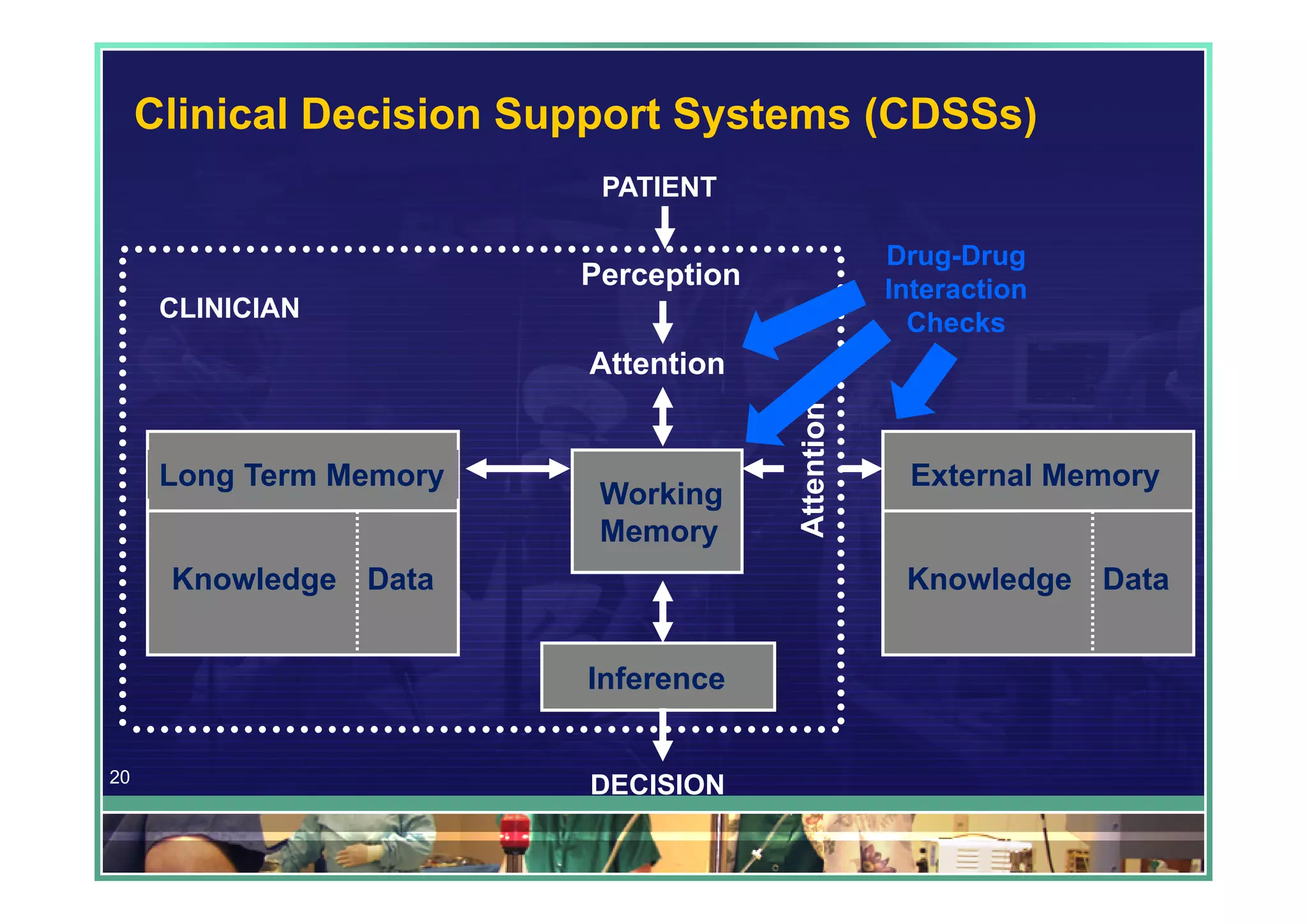
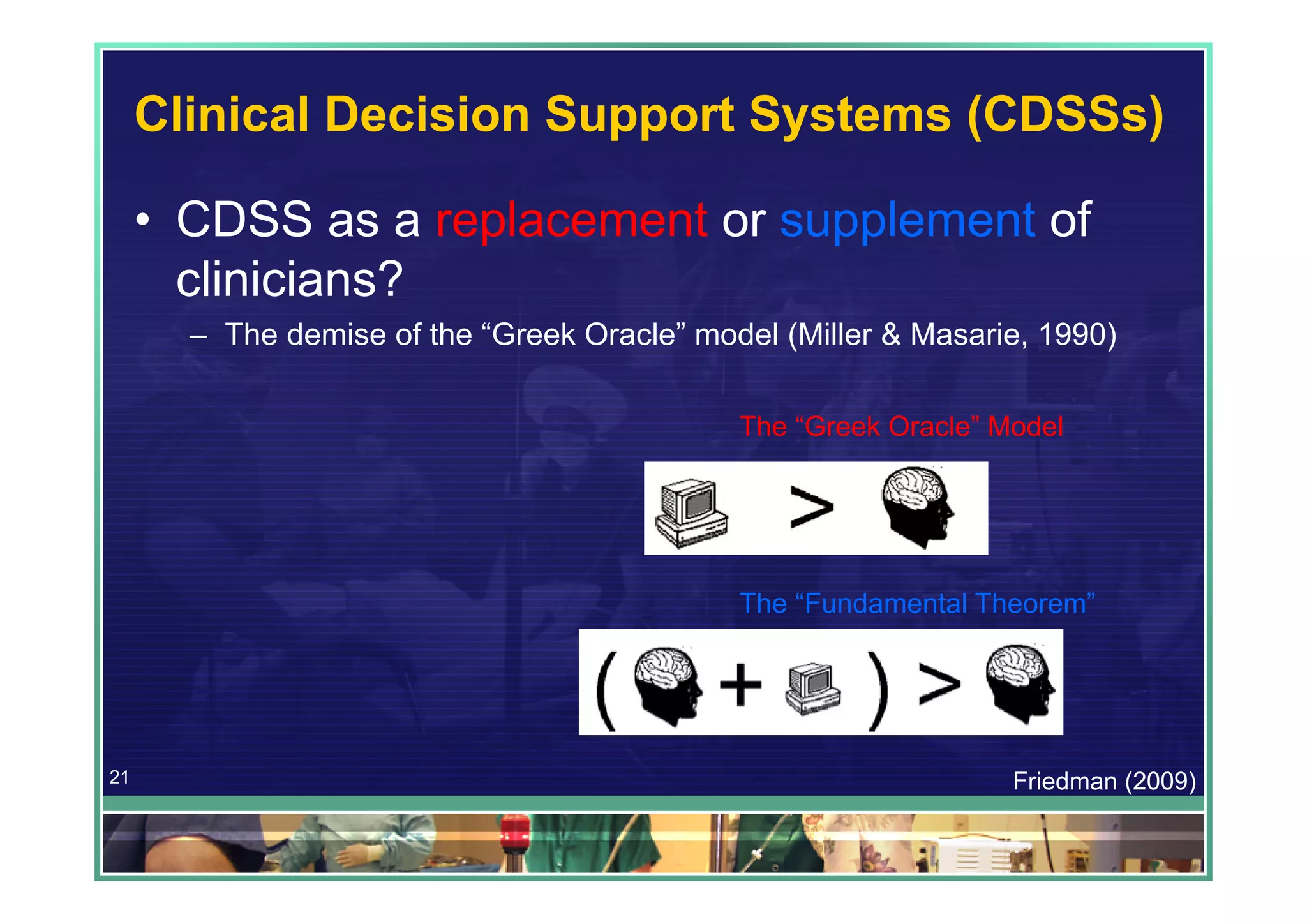
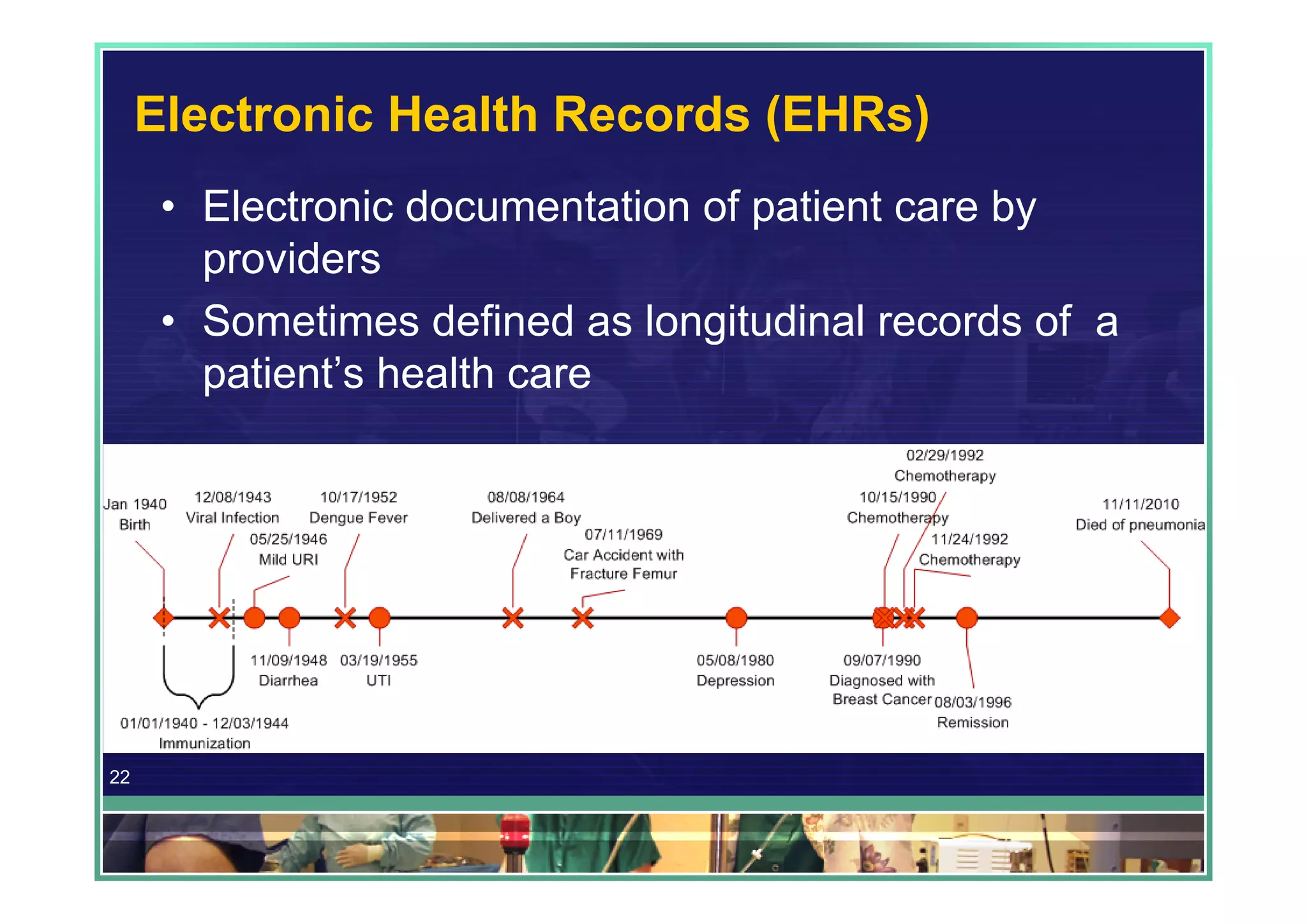
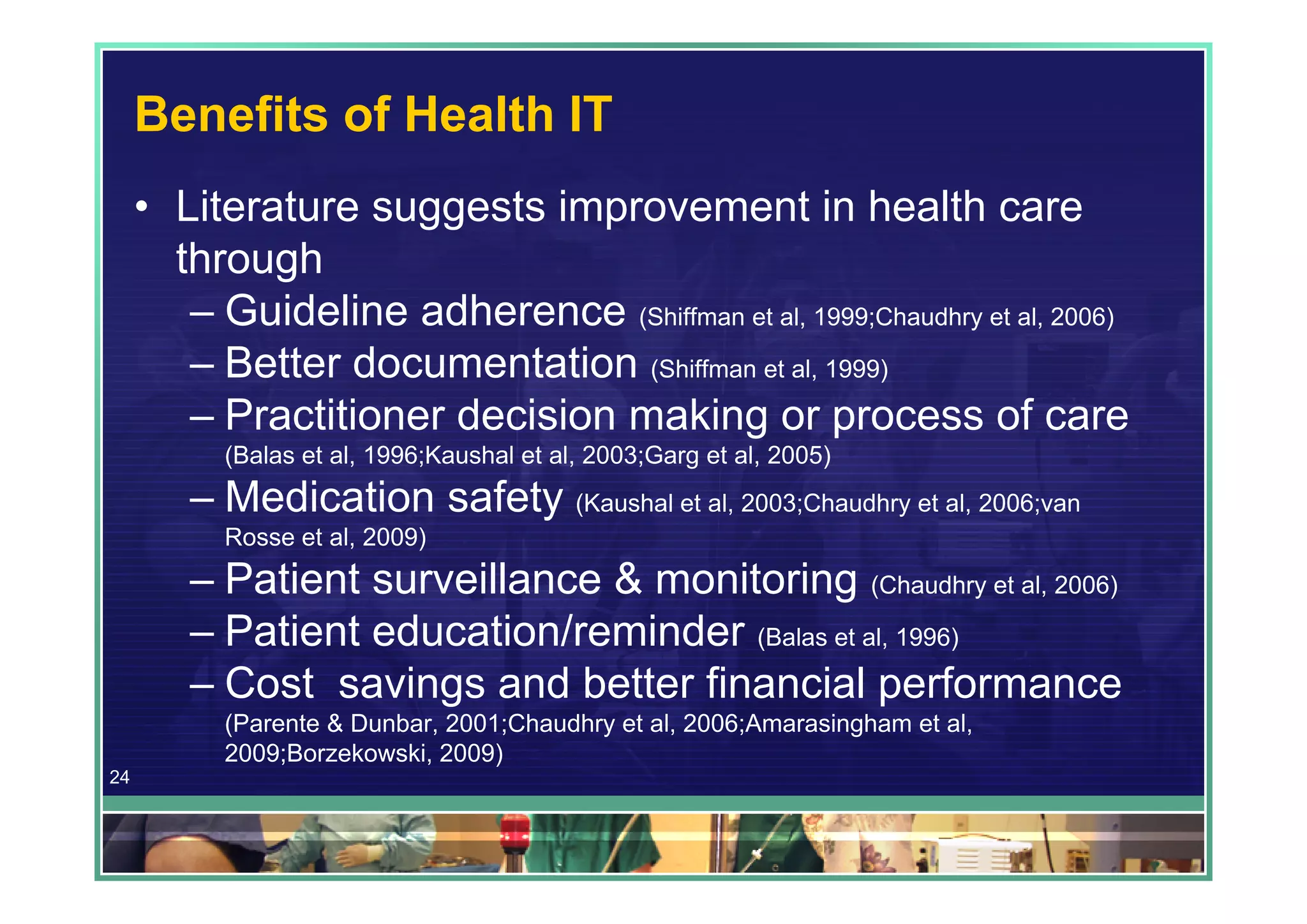
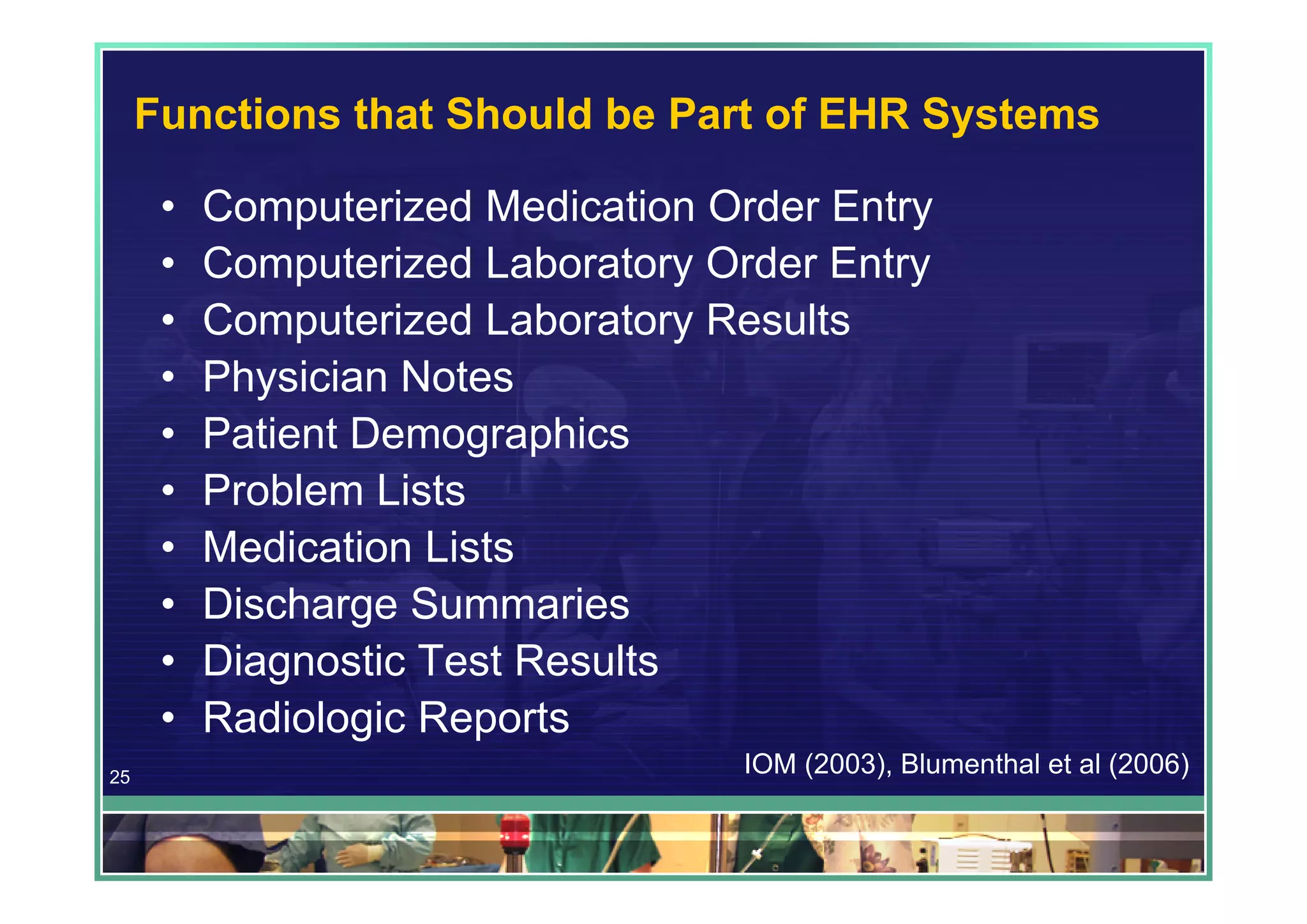
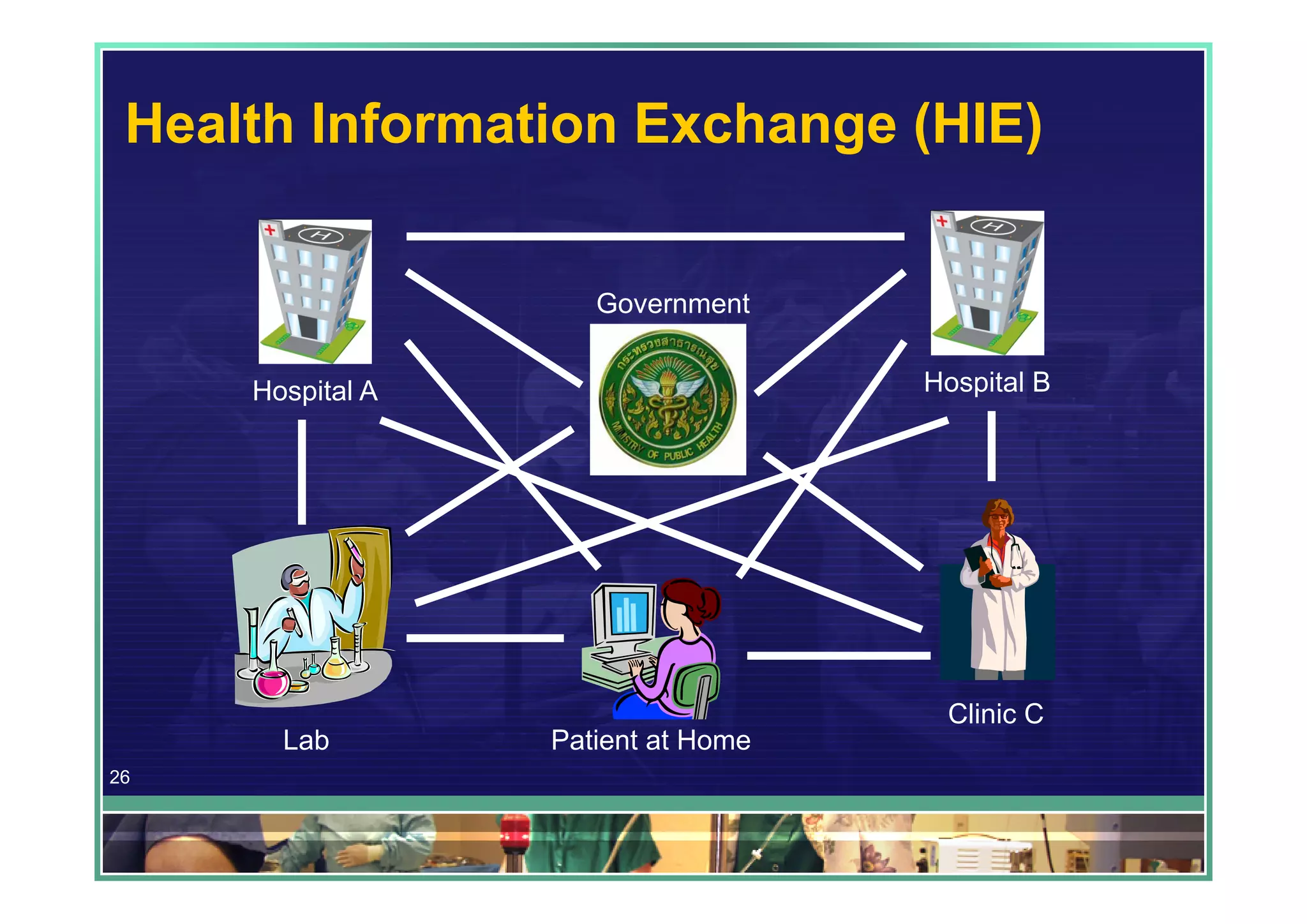
The document discusses the significance of informatics in emergency medicine, highlighting its role in improving patient care through enhanced information management and technology use. It covers various applications such as electronic health records (EHRs), clinical decision support systems (CDSS), personal health records (PHRs), and mobile health (mHealth), emphasizing their transformative potential for healthcare processes. The conclusion stresses the necessity of integrating health IT and informatics to better manage emergencies and enhance care quality.
![Biomedical & Health Informatics
• “[T]he field that is concerned with the optimal
use of information, often aided by the use of
technology, to improve individual health, health
care, public health, and biomedical research”
(Hersh, 2009)
• “[T]he application of the science of information
as data plus meaning to problems of
biomedical interest” (Bernstam et al, 2010)
3](https://image.slidesharecdn.com/informaticsinemergencymedicine-abriefintroductionpresentation-120131092323-phpapp01/75/Informatics-in-Emergency-Medicine-A-Brief-Introduction-Presentation-3-2048.jpg)
![Personal Health Records (PHRs)
• “An electronic application through which individuals can
access, manage and share their health information,
and that of others for whom they are authorized, in a
private, secure, and confidential environment.” (Markle
Foundation, 2003)
• “A PHR includes health information managed by the
individual... This can be contrasted with the clinician’s
record of patient encounter–related information [a
paperchart or EHR], which is managed by the clinician
and/or health care institution.” (Tang et al., 2006)
27](https://image.slidesharecdn.com/informaticsinemergencymedicine-abriefintroductionpresentation-120131092323-phpapp01/75/Informatics-in-Emergency-Medicine-A-Brief-Introduction-Presentation-27-2048.jpg)