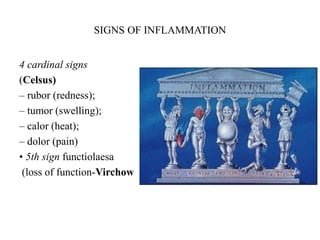
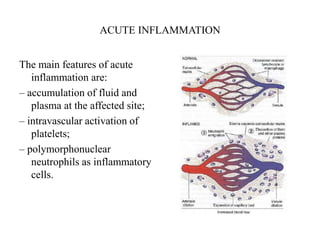
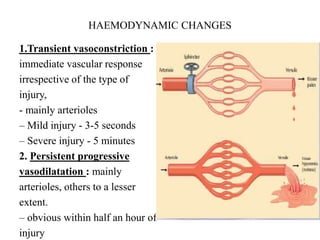
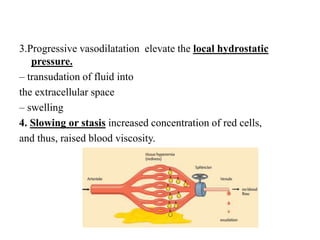
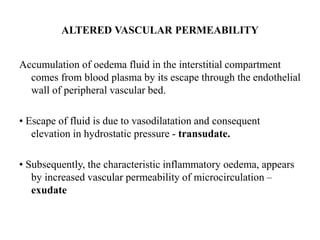
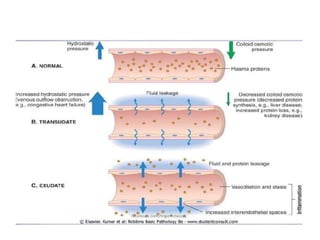
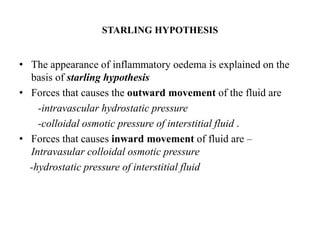
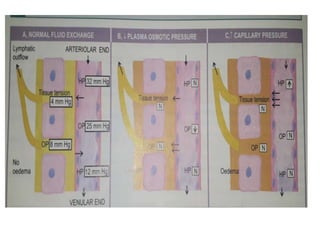
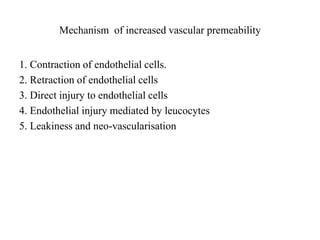
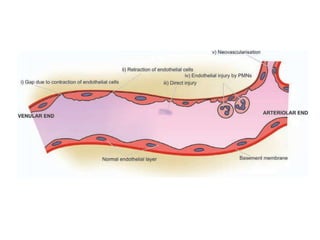
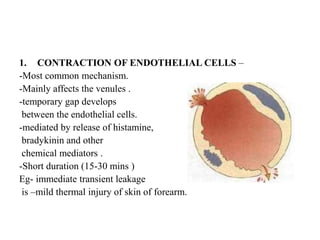
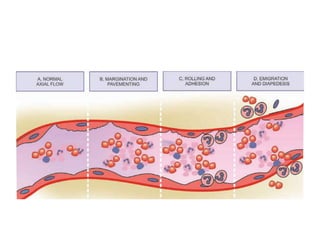
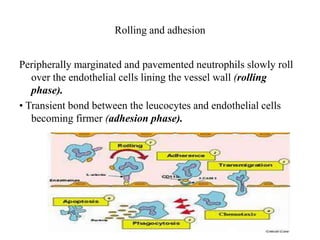
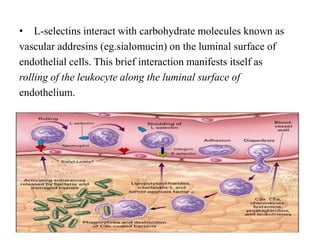
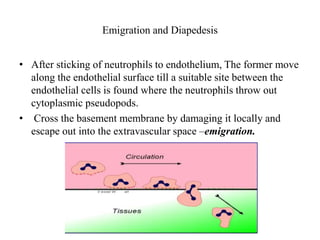
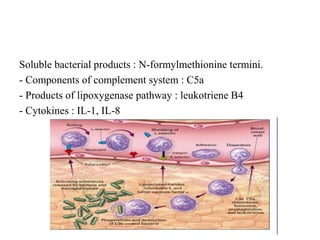
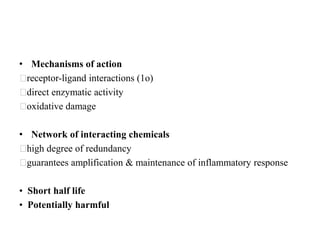
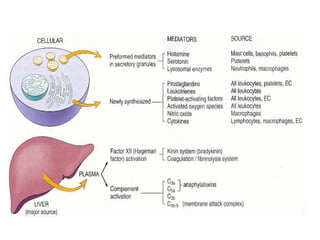
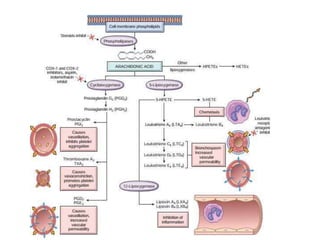
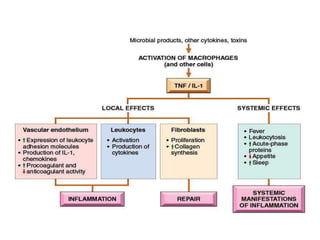
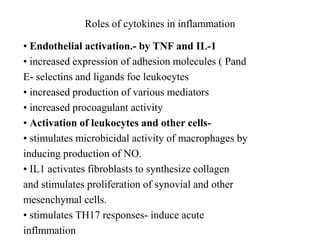
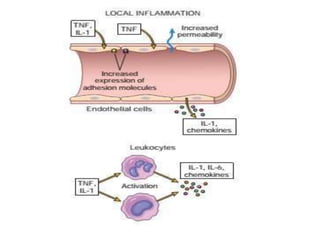
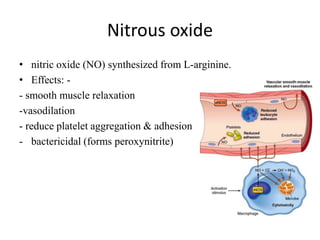
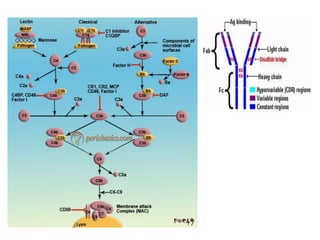
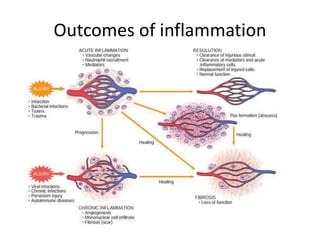
This document provides an overview of inflammation and the mediators involved. It defines inflammation and describes the causes and types. The key events of acute inflammation are discussed, including vascular changes like increased permeability and cellular events like chemotaxis and phagocytosis. Finally, it outlines several important mediator classes derived from arachidonic acid that are involved in regulating the inflammatory response, such as prostaglandins, leukotrienes, and thromboxanes. These mediators stimulate vascular and cellular reactions to initiate and propagate the inflammatory cascade.



![Inflammation [autosaved]](https://image.slidesharecdn.com/inflammationautosaved-180806124543/85/Inflammation-autosaved-86-320.jpg)