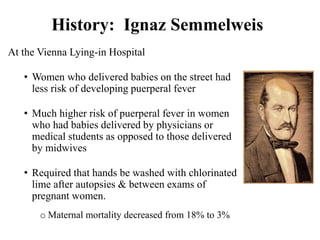
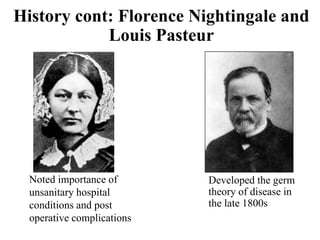
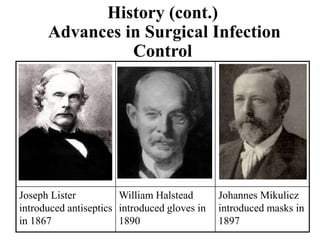
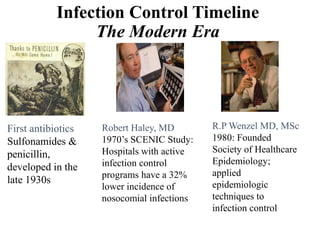
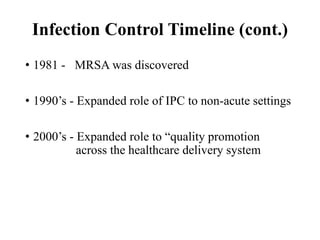
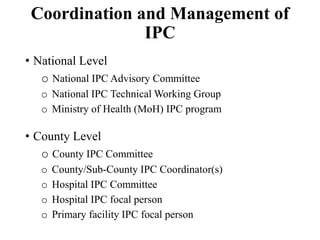
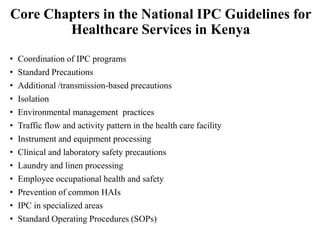
This document provides an introduction to infection prevention and control (IPC) in healthcare settings. It defines IPC and healthcare-associated infections (HAIs), describes the historical evolution of IPC practices from Semmelweis to Nightingale to modern standards, and outlines current IPC structures and practices including standard and additional precautions to prevent transmission of infections in healthcare facilities. The benefits of adhering to IPC practices include improved quality of care, reduced risk to healthcare workers, and lower healthcare costs.