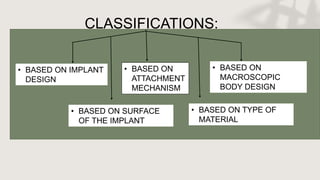
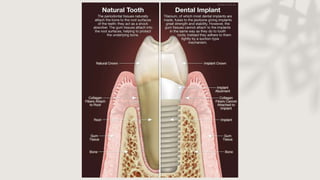
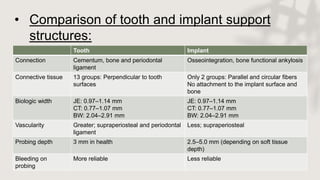
Implants provide an overview of basic implant concepts including classifications based on design, attachment mechanism, material, and surface characteristics. Key points include:
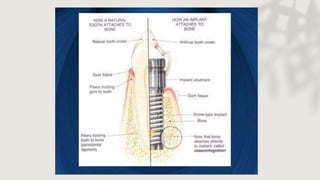
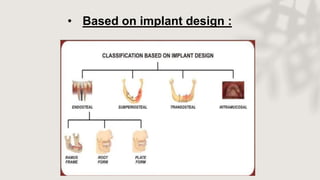
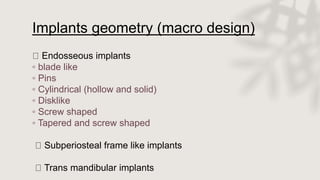
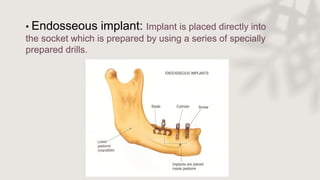
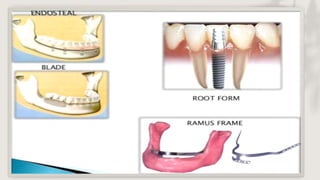
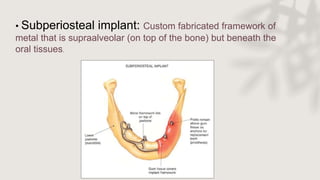
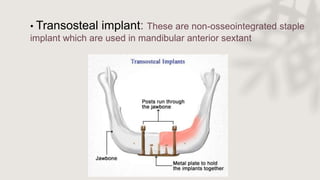
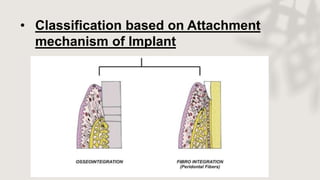
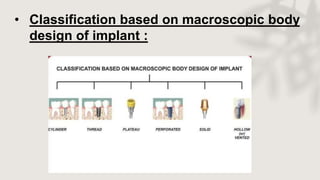
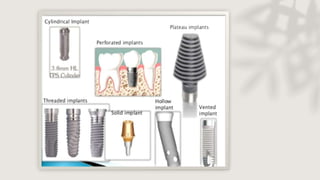
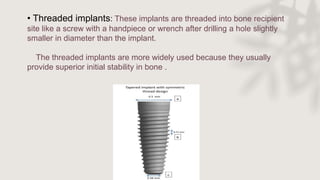
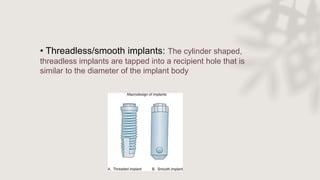
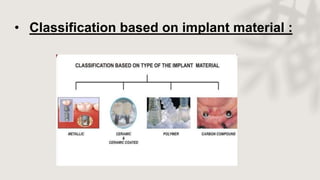
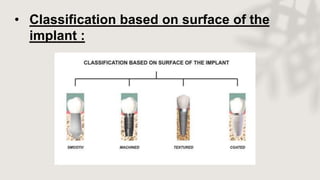
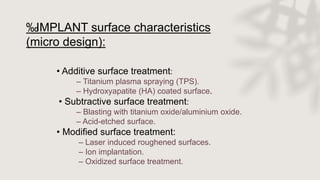
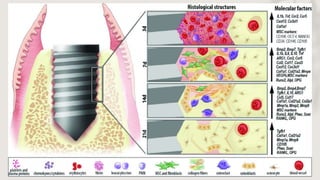
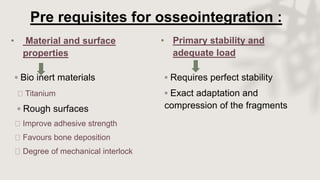
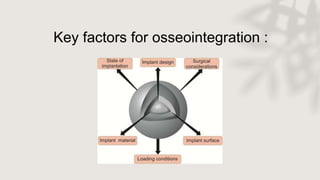
- Implants are classified based on their macro design (endosseous, subperiosteal), attachment mechanism (threaded, threadless), material (titanium, zirconia), and surface characteristics (acid-etched, plasma sprayed).
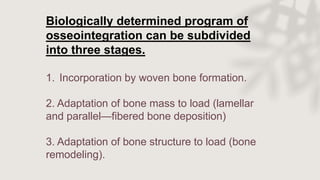
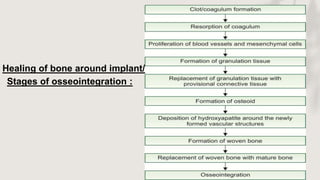
- Osseointegration is the direct structural and functional connection between living bone and the implant without soft tissue interference. It occurs in three stages: woven bone formation, lamellar bone deposition, and bone remodeling.
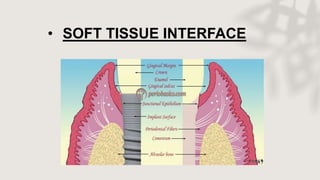
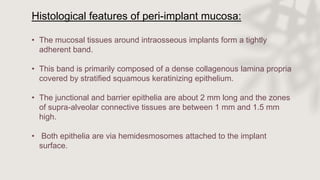
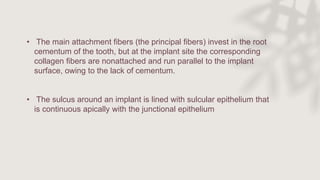
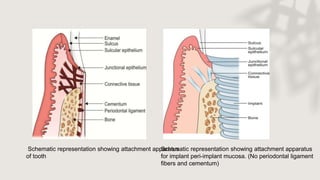
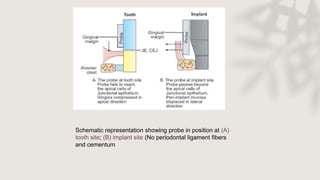
- The peri-implant mucosa forms an attachment to the implant