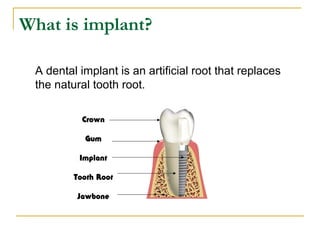
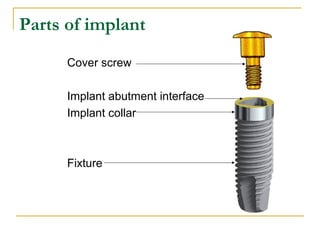
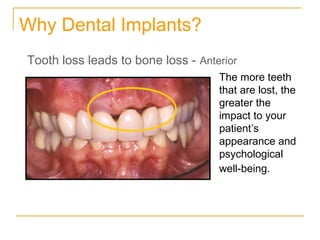
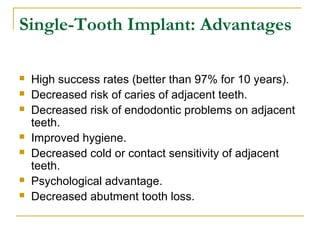
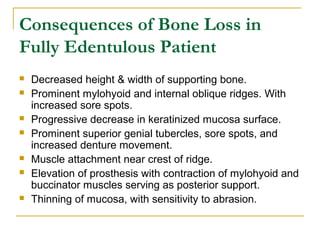
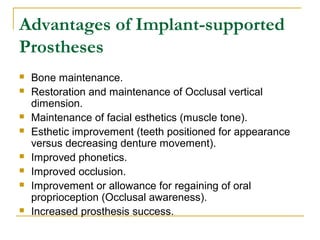
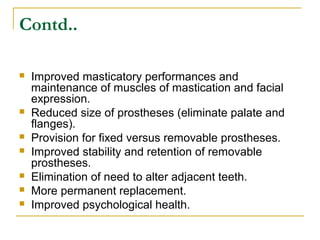
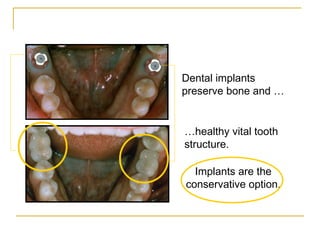
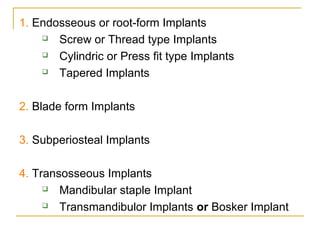
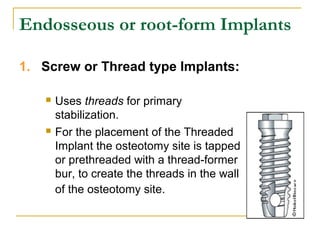
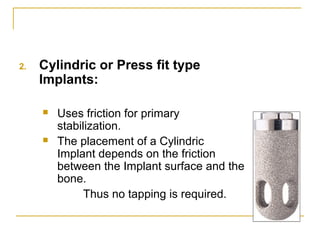
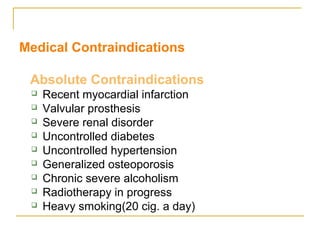
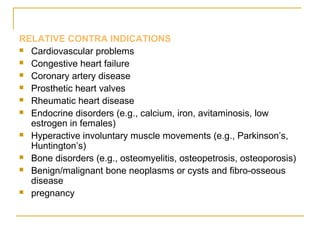
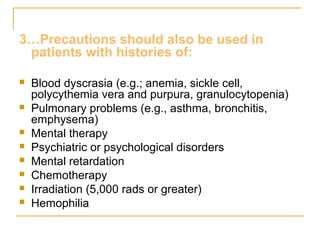
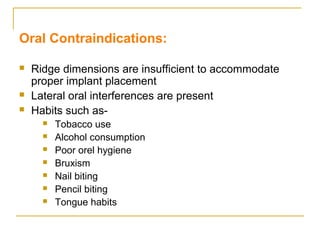
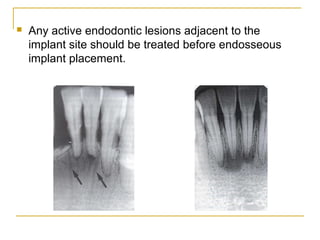
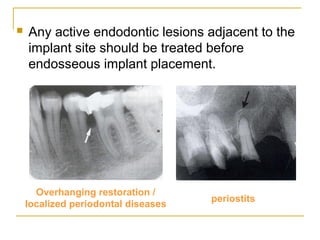
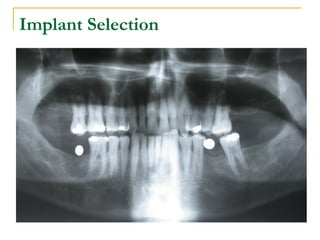
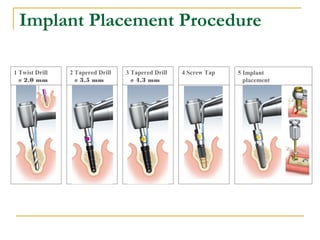
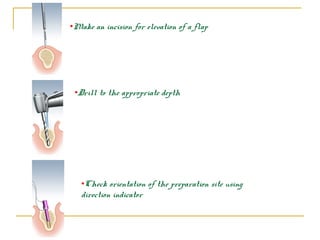
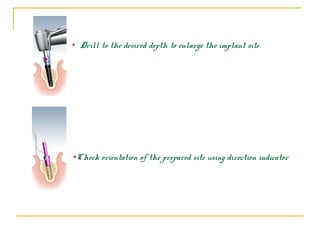
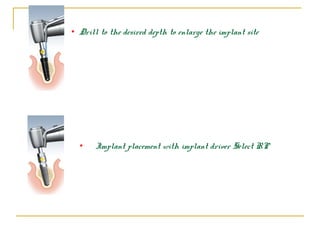
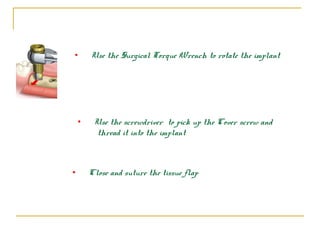
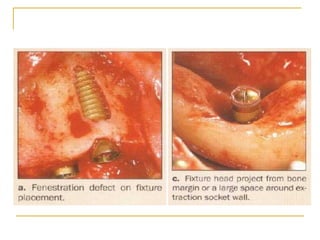
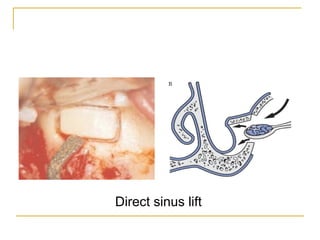
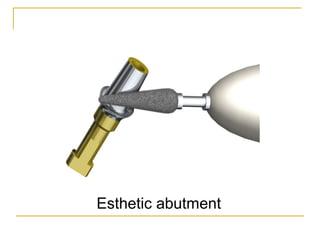
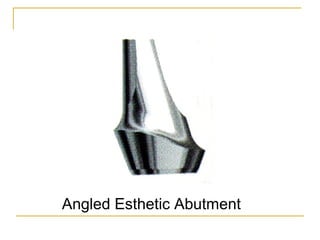
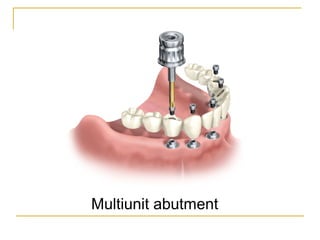
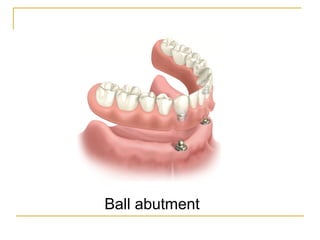
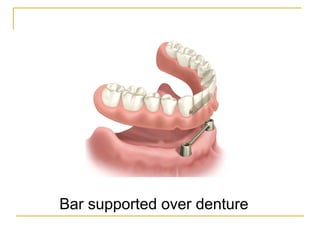
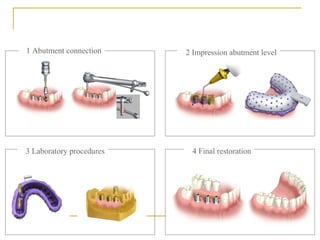
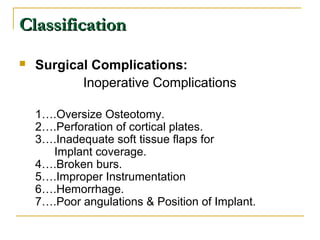
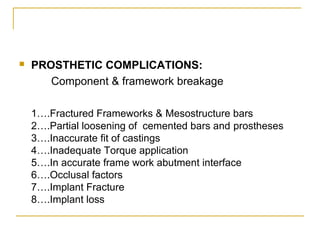
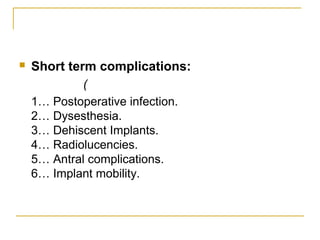
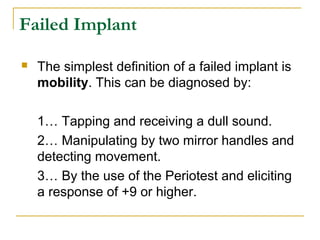
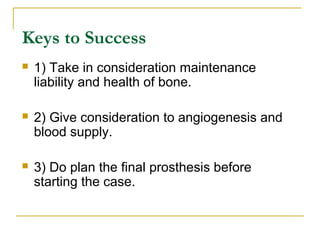
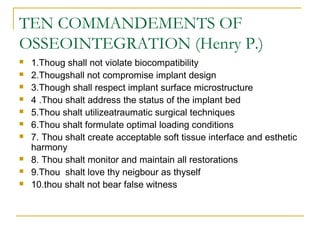
This document discusses dental implants and their use in dentistry. It defines what an implant is, describes the different parts and types of implants. It also outlines the implant placement procedure and discusses factors to consider for pre-surgical planning like medical/oral contraindications and patient selection. Complications of sinus lift procedures are mentioned. The document emphasizes the importance of osseointegration between implants and bone. Finally, it briefly introduces the prosthetic phase including different types of abutments and restorative solutions like cement-retained and screw-retained restorations.