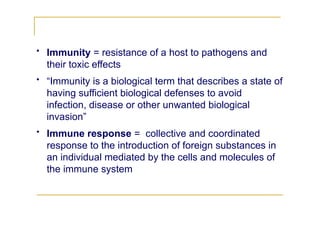
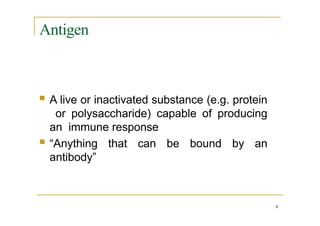
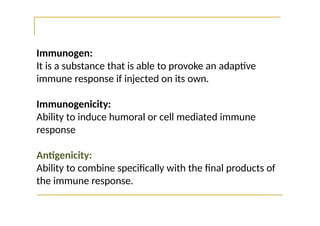
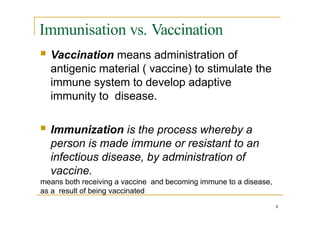
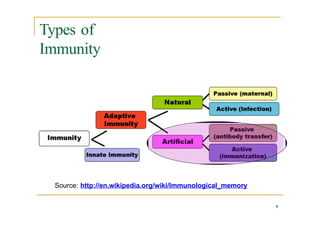
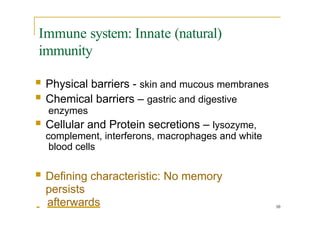
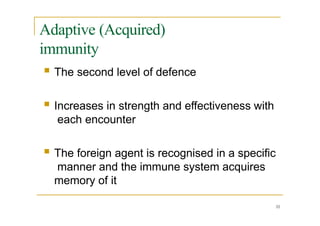
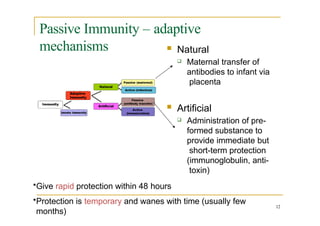
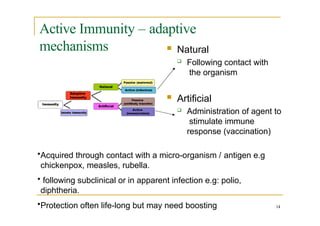
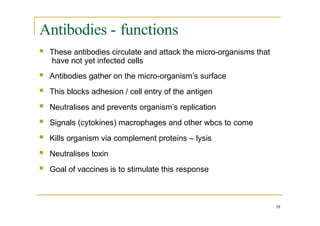
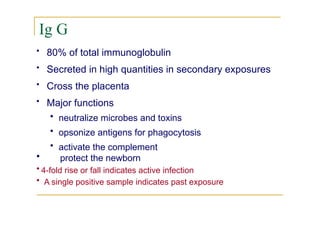
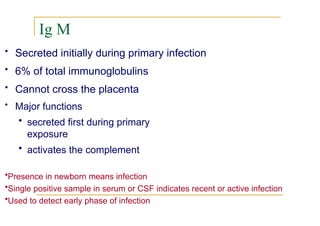
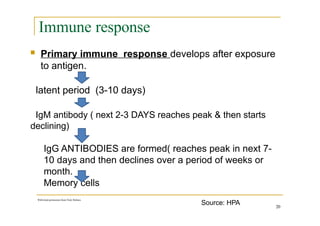
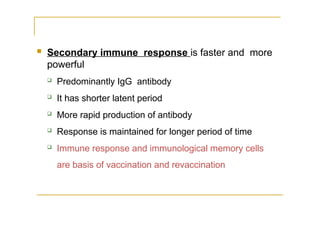
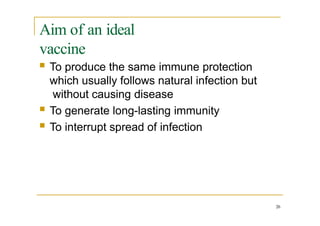
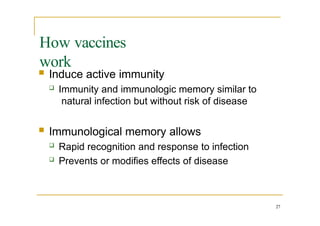
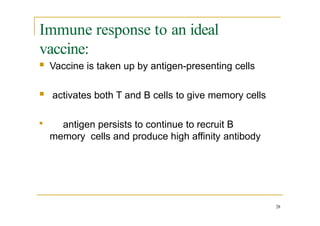
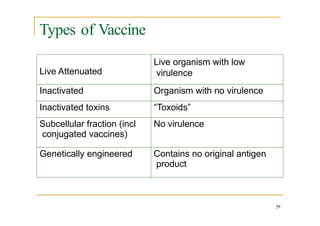
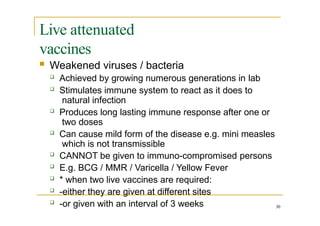
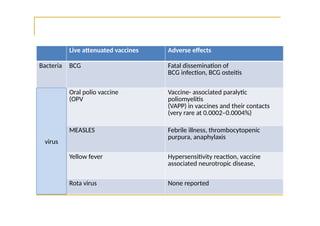
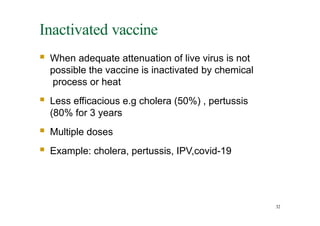
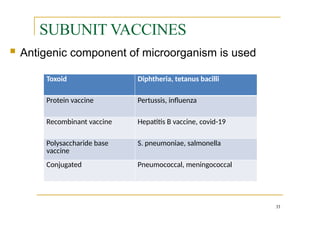
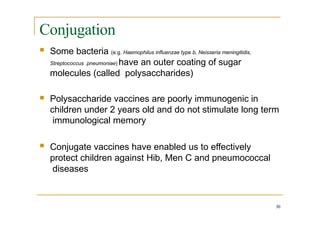
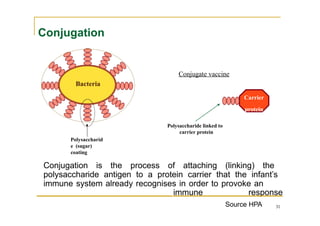
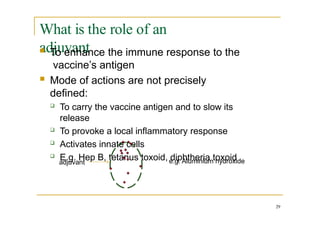
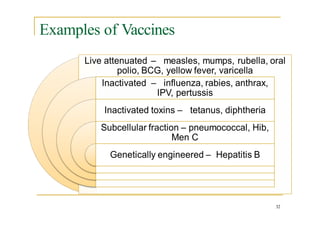
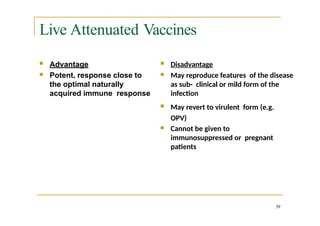
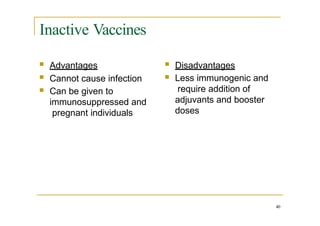
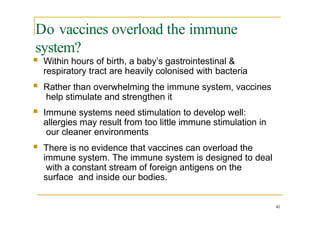
The document outlines the principles of immunity and how vaccines function, covering key concepts such as active and passive immunity, types of vaccines, and the immune response elicited by vaccination. It emphasizes the importance of herd immunity in protecting vulnerable populations and explains the mechanisms behind various vaccine types including live attenuated, inactivated, and conjugate vaccines. The goal of vaccination is to provide long-lasting immunity without causing disease, ensuring a strong immune response to future infections.