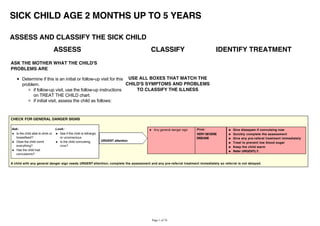
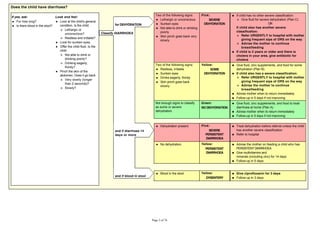
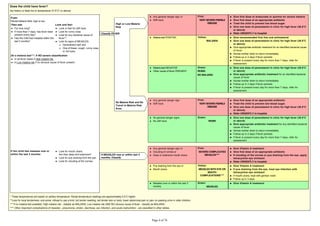
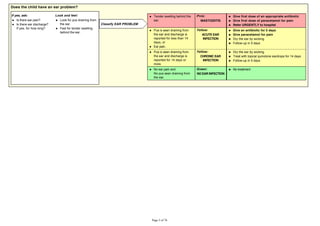
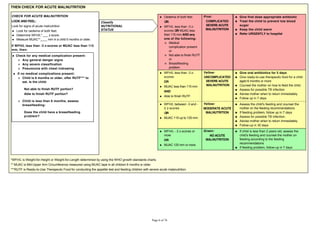
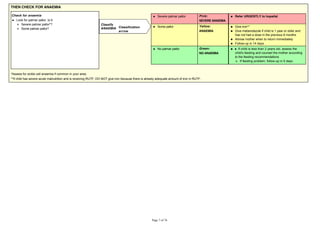
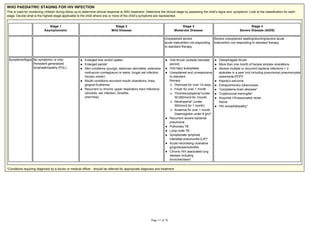
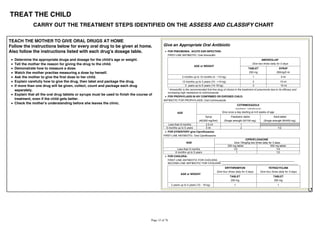
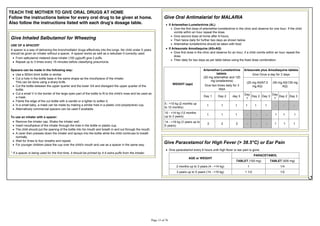
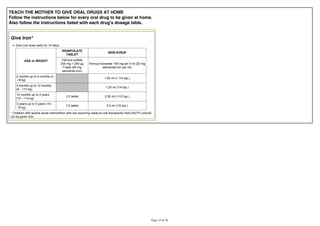
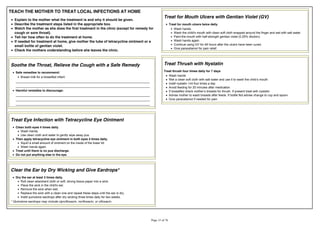
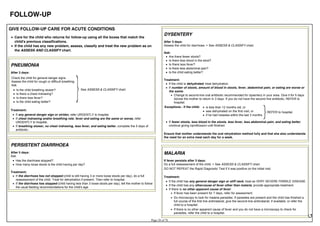
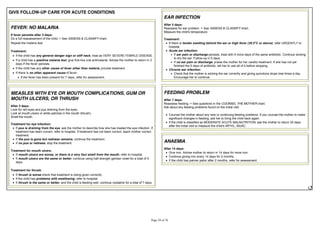
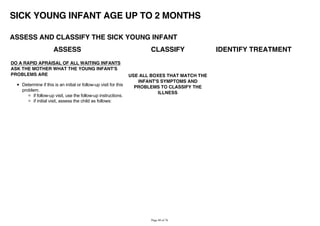
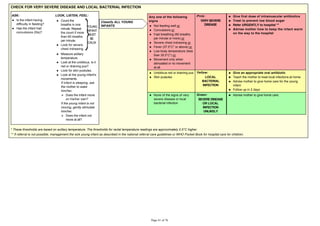
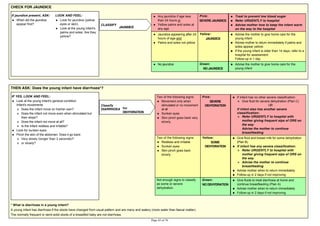
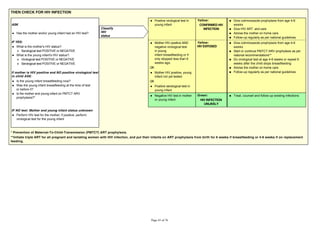
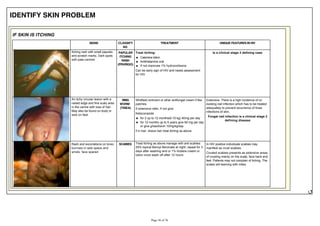
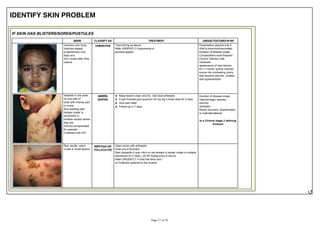
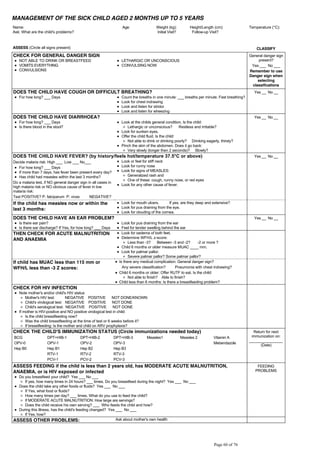
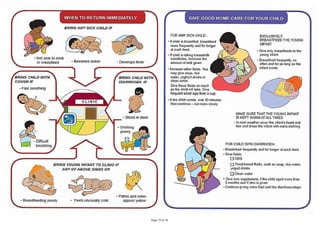
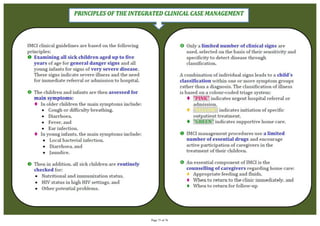
This document provides guidance on assessing and classifying sick children between the ages of 2 months and 5 years based on their symptoms. It outlines steps to determine danger signs, main symptoms of cough/difficult breathing, diarrhea, and fever. For each symptom, the guide describes how to classify the child's condition as very severe, severe, or not severe based on examination findings. It then provides treatment recommendations according to the illness classification to treat the child, advise the caregiver, or refer the child for further care. The purpose is to help health workers promptly manage common childhood illnesses.