This dissertation examines the role of family counseling in managing obesity and overweight among children and adolescents in India, highlighting the rising prevalence of these issues, which is expected to reach 17 million obese children by 2025. The study reveals that parental involvement and counseling are instrumental in combating obesity, with various research indicating successful weight loss when parents are engaged in interventions. The impact of obesity on health, social dynamics, and the environment at home is emphasized, stressing the need for comprehensive strategies that include family support to address this public health challenge.






![17
implement policies and programmes to promote a positive environment for health; more
specifically changes in diet, and physical activity patterns.
Obesity is a very complex problem as it involves genetic, biological, developmental,
environmental as well as behavioural factors. It is becoming a major health problem and has
been recognised as such all over the world now. The reason of obesity in childhood and
adolescence is mainly an inequity in energy balance. Which means an excess of calorie intake
without an appropriate calorie expenditure. The increasing prevalence of obesity in childhood
and adolescence is associated with a rise in co-morbidities which were earlier seen only in
adults, e.g Type 2 Diabetes Mellitus, Hypertension, Non-alcoholic Fatty Liver Disease
(NAFLD), Obstructive Sleep Apnea (OSA), and Dyslipidemia. [2]
Also, obesity increases the risk of early puberty in children, menstrual irregularities in
adolescent girls (PCOS), high Cholesterol levels, Metabolic Syndrome.
Additionally, obese children and adolescents can suffer from psychological issues such as
Depression, Anxiety, Poor Self-esteem, body image issues, Peer relationships, and eating
disorders like Bulimia Nervosa (BN), Binge-eating disorder (BED), Night Eating Syndrome
(NES). Sometimes to be healthy and restrict their diet they may cross the extreme and suffer
from Anorexia Nervosa (AN)
Statement Of The Problem:
The Role of Family Counselling in Obese and Overweight Children and Adolescents.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-17-320.jpg)
![18
To understand this topic, we first need to be clear about the meaning of overweight and
obesity.
Definition Of Overweight and Obesity and its Measurement:
Obesity is defined as a condition of abnormal or excessive fat accumulation in adipose
tissue, to the extent that health may be impaired (WHO consultation on obesity, 2000)
It has to be pointed out here that the terms overweight and obesity are often used
somewhat loosely and interchangeably. However, standardisation is necessary for
international and secular comparisons.
Measurement of Obesity;
There are many methods of measuring body fat of a person, for e.g.,
1.BMI (Body mass index), There are two BMI charts that can be used for Indian Children as
of now :
(1)The NCHS/ CDC charts from USA. The American Obesity Association uses the 85th
percentile of BMI for age and sex as a reference point for overweight and the 95th
percentile for obesity in children. Bhave.S, et al,(2004) [12]. These charts can be readily
downloaded from the internet sites, but are based on well off populations from USA.
(2)Recently, new BMI standards in children using a large internationally representative
sample from six different countries (not India), with widely differing prevalence rates for
obesity have been published. Age and sex-specific BMI cut-off points for defining
overweight and obesity in children have been derived by identifying percentiles in](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-18-320.jpg)






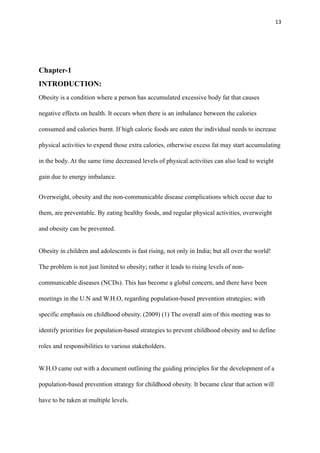
![25
Chapter-2
REVIEW OF LITERATURE
Studies published previously as well as reviewed by other scientists and published as review
articles were studied, to understand what others have done and found regarding the role of
parents in controlling overweight and obesity in children and adolescents.
Foreign Studies
1. Study in Australia:
Rebecca Golley.R, Anthea M. Magarey, Louise A. Baur, Katherine S. Steinbeck, Lunne A. Daniels,
(2007)[13], The Objec
ti
ve of this study was to evaluate the rela
ti
ve e
ff
ec
ti
veness of paren
ti
ng skills
training as a key strategy for the treatment of overweight children.
The Sample consisted of an assessor binded, randomized, controlled trial involving 111(64% female)
overweight, prepubertal children 6 to 9 years of age. They were randomly assigned to paren
ti
ng skills
training plus intensive lifestyle educa
ti
on, paren
ti
ng skills training alone, or a 12 month waitlisted
control. Height, BMI and waist circumference z score and metabolic pro
fi
le were assessed at
baseline, 6 months and 12 months, with an inten
ti
on to treat.
Aim of this study was to evaluate the rela
ti
ve e
ff
ec
ti
veness of paren
ti
ng skills training as a key
strategy for the treatment of overweight children. It tests the hypothesis that prepubertal children
whose parents par
ti
cipate in a family focused child weight management program, comprising
parental skills training and intensive lifestyle modi
fi
ca
ti
on educa
ti
on , will have BMI and waist
circumference z scores and metabolic pro
fi
les a
ft
er 12 months that will be :
(1) Improved when compared to wait listed children and](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-25-320.jpg)
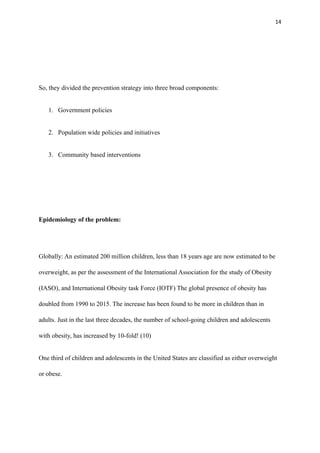
![26
(2) No di
ff
erent from children whose parents par
ti
cipate in a program that focused on paren
ti
ng skills
training alone.
Design: A single - blinded, randomized, controlled trial(Australian Clinical Trial Register
00001103[ www.actr.org.au]) was used to determine the e
ff
ec
ti
veness of 2 child weight-
management interven
ti
ons, namely paren
ti
ng-skills training with intensive lifestyle educa
ti
on
(P+DA),and paren
ti
ng- skills training alone(P). These interven
ti
ons were compared with each other
and with a control group wait-listed for interven
ti
on for 12 months (WLC).
Parents in the P and WLC groups received a general ‘ healthy- lifestyle’ pamphlet.
The study was conducted at 2 metropolitan teaching hospitals in Adelaide, South Australia. It was
approved by Flinders Clinical Research Ethics, and Women’s and Childrens’ Hospitals Ethics
commi
tt
ees. The design, conduct, and repor
ti
ng of this study followed the guidance outlined in The
Consolidates Standards of Repor
ti
ng Trials (CONSORT) statement.
The Randomiza
ti
on schedules were computer generated using a three block design. Individual group
alloca
ti
ons were sealed in opaque envelopes, with the next envelope opened on a child’s comple
ti
on
of baseline measurements. Researchers involved in the recruitment, par
ti
cipant alloca
ti
on, and
interven
ti
on or data collec
ti
on, were not involved in the randomiza
ti
on process.
Dr. Golley had developed the lifestyle educa
ti
on component a
ft
er undertaking accredited training for
the paren
ti
ng component. All interven
ti
on sessions were conducted by him only.
The Interven
ti
on sessions were based en
ti
rely on the mode of parent-only. Parents were supposed to
have the sole responsibility for a
tt
ending program sessions and implemen
ti
ng family lifestyle change.
Children did not a
tt
end any educa
ti
on sessions. The family was encouraged to implement change at
family level and not only the child level.
Interven
ti
on Descrip
ti
ons:
P -Group: For Paren
ti
ng skills training the parents par
ti
cipated in a standardized and evaluated
general paren
ti
ng program—Triple P( Posi
ti
ve Paren
ti
ng Program); which is based on Child](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-26-320.jpg)



![30
not powered for studying a gender di
ff
erence in weight loss; but a signi
fi
cant di
ff
erence was
observed between them, and further studies are recommended to include gender di
ff
erence also.
An unan
ti
cipated reduc
ti
on in BMI z scores in the control group produces the poten
ti
al for type II
error.
The Ar
ti
cle concludes that a Family focused interven
ti
on using paren
ti
ng skills training and promo
ti
ng
a healthy lifestyle may be an e
ff
ec
ti
ve approach to weight management in prepubertal children. Both
Paren
ti
ng skills training and lifestyle educa
ti
on are poten
ti
ally important components. This approach
addresses family and parental factors in
fl
uencing childrens’ ea
ti
ng and ac
ti
vity behaviours and
achieves a moderate reduc
ti
on in adiposity a
ft
er 12 months.
2.Angelina Fowler Brown, (2002)[14]. The candidate ar
ti
cles and the data sources were iden
ti
fi
ed
through searches of Cochrane Database of Systema
ti
c Reviews, and Websites of the Na
ti
onal
Ins
ti
tutes of Health, the CDC, and the Na
ti
onal Guideline Clearing house. Other sources of ar
ti
cles
included bibliographies of review ar
ti
cle that speci
fi
cally addressed overweight preven
ti
on or
treatment in children and adolescents. Studies were included only if their primary aim was
overweight preven
ti
on ot treatment, and were large observa
ti
onal studies, or randomized controlled
trials(RCTs), using more than 50 pa
ti
ents. Studies were not considered if they did not use outcomes
that included weight or BMI measurements. Seven studies that used a popula
ti
on approach to the
preven
ti
on of overweight in preschool or school aged children and adolescents were iden
ti
fi
ed.
These studies used a no-interven
ti
on control excep
ti
ng one cohort study. Most of these were
randomized. Only one of these studies had been undertaken outside of the United States. These
studies were heterogenous and had mixed results. Four of the studies used a mul
ti
component
school based interven
ti
on program, involving nutri
ti
on and physical ac
ti
vity. One of them also
involved educa
ti
on to reduce sedentary behaviours. They found that school-based preven
ti
on
programs are generally not successful in reducing the prevalence of obesity. Even extra sessions of
physical ac
ti
vity in school were not successful. A study which had focused on nutri
ti
on educa
ti
on
showed moderate success. Treatment interven
ti
ons required, like behavioural therapy, reduc
ti
on in
sedentary behaviour, nutri
ti
on and physical ac
ti
vity educa
ti
on are moderately successful, but may
not be generalised to the primary care se
tti
ng. The ar
ti
cle concludes that rather than focusing on](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-30-320.jpg)
![32
• 3.Kittiya Rattanamanee, and Chintana Wacharasin, (2021)[5] A Quasi
Experimental Study, conducted for 7-weeks found that the group I which
received a Family based behavioural counselling program ,had significantly
better healthy eating habits at the end as compared to Group II which received
group based counselling and the Control Group III which received only a
usual program. The findings indicated that this program could enhance healthy
eating behaviour and physical activity and decrease BMI in children with
obesity.
• 4.A Systematic Review, conducted by Saravana Kumar Kothandan, (2014)[6],
identified 1231 articles, out of which 13 met the criteria. Out of 13 studies, eight were
Family based interventions (n=8) and five were school based (n=5), with total
participants (n=2067). The participants were aged between 6 and 17 and the study
duration ranged between one month and three years.
Family based interventions demonstrated effectiveness for children under the age of
twelve; and School based interventions were most effective for children in 12 to 17
age group, with differences for both long-term and short-term results.
5.Nicholas D Spence, Amanda S Newton, Rachel A. Keaschuk, and Geoff D Ball, in
(2022)[16], conducted a research on basis of the fact that Obesity interventions for
parents of children with obesity can improve children’s weight and health.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-32-320.jpg)
![34
0.01(95% Cl=-0.08 to 0.06, p=0.80) Similar results were found across all Secondary
outcomes.
The CBT based intervention for parents of children with Obesity was not found to be superior
in reducing BMIz scores vs PEP based intervention.
It was concluded that both therapies showed almost equal results and the results were not
significantly different in the two approaches used.
We have considered this study to highlight the importance of parental involvement and
counselling in the management of overweight and obese children. This study confirms that
both methods of counselling CBT and PEP are equally effective in solving the problem,
and once again it confirms that counselling parents has a very important role in helping
overweight and obese children and adolescents in reducing their weight.
• 6.An article published in American Psycologist,(2020) [25] by
The Guideline Development panel for Treatment Of Obesity, American Psycological
Association (2020); provided the recommendations intended for psycologists, Health and
Mental health professionals, patients,families and policy makers. The guideline
development panel (GDP), used a systematic review conducted by Kaiser Permanente
Research Affiliates Evidence-based practice center as its primary evidence base.
(O’Conner, Burda, Eder, Walsh,& Evans,2016). The GDP consisted of researchers and
clinicians psycology, nursing, nutrition and medicine. They had also involved adult
community members who had childhood and adolescent experience with obesity.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-34-320.jpg)
![35
The Criteria they used were for critically rating the evidence and formulating their
recommendations were; change in body mass index (BMI or zBMI) and serious adverse
events. Their recommendations were as follows:
The GDP strongly recommended that children and adolescents from age 2 to 18 years with
overweight and obesity, should receive family based, multicomponent behavioural
interventions; with a minimum of 26 contact hours. These should be initiated at the earliest
age possible. GDP has not as yet made any recommendations about specific forms of familty
based multicomponent behavioural interventions with respect to their comparative
effectiveness, due to lack of sufficient evidence.
The above guidelines based on evidence based research strengthen our view; that family
counselling has a very important role to play in controlling childhood and adolescent
overweight and obesity.
• 7. David M. Janicke, Ric G.Steele, Laurie A. Gayes, MS et al, (2014), (17)
The study was a meta-analysis of randomized controlled trials examining the efficacy of
comprehensive behavioural family lifestyle interventions (CBFLI) for pediatric obesity. They
searched the common research databases for articles. Their inclusion criteria were met by 20
articles of different studies with 42 effect sizes and 1671 participants. They conducted an
assessment for risk bias, and rating of quality of the evidence.
Results of this study were as follows: The overall effect size for CBFLIs as compared with
passive control groups over all time points was statistically significant (Hedge’s g = 0.473,
95% confidence interval [.362,.584]) and suggestive of a small effect size. Duration of
treatment, number of treatment sessions, the amount of time in treatment, child age, format of](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-35-320.jpg)


![38
➢ Strategies including differential attention and contingency management
➢ Stimulus control
The review analysis goes further and mentions:
“ Parents are often considered a critical agent of change in bahavioural lifestyle interventions,
as they exercise significant control over children’s eating and physical environment, and
ultimately behaviours.”
This is more so in our country, India, as children and adolescents are groomed in a
dependent style, and are very close to and also live together until they get married and
have to move out of town for a job.
Thus this study statistically proves our viewpoint, that Parental counselling to involve
them in overall behavioural and lifestyle change towards healthy living for the whole
family have an important role to play in controlling the weight of overweight and obese
children and adolescents.
This study, also provides references of many other evidence based studies reinforcing our
point in clear terms.
• 8. David M. Janicke,PhD, Ric G.Steele, PhD, Laurie A. Gayes, MS, Ishadi R, Azizi-
Soleiman F. (2014);[18]
In their Review article said, the epidemic of childhood obesity is no more limited to high-
income countries and has become one of the most important global health problems of the
21st century.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-38-320.jpg)

![42
It came out that researchers all over the world are finding that family based programs for
controlling overweight and obesity in children and adolescents are even better than school
based programs or clinic based programs.
This confirmed with what we had set out to study.
• 9. Kirsten Weir, (April 2019) [19], in her review article writes,
“ Both Wilfley and Raynor were among a panel of obesity experts who develpoed
a new APA (American Psychology Association) clinical practice guideline to
provide recommendations on treatment of overweight and obesity in children
and adolescents”. (Clinical Practice Guideline for Multicomponent Behavioural
Treatment of Obesity and Overweight in Children and Adolescents( h
tt
ps://
www.apa.org/obesity-guideline/clinical-prac
ti
ce-guideline.pdf) March 2018)
After reviewing the literature the guideline panel found strong evidence to
recommend Family- based behavioural interventions, to treat obesity in children 2-18
years old. They focus not only on the children but the whole family to engage in a
healthier lifestyle by improving the diet, physical activities, and by reducing sedentary
behavoiur.
They also focus on behaviour change, teaching strategies to parents for Goal setting,
problem solving, monitoring their childrens’ behaviours,and. also by modelling
positive parental behaviours.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-42-320.jpg)

![44
session group. Just 48% of the children in the control group had reached the weight
loss targets after one year. ( JAMA Pediatrics (h
tt
ps://www.ncbi.nlm.nih.gov/pmc/
ar
ti
cles/PMC6169780/),Vol.171, No.12, 2017)
APA’s Clinical guideline recommends a minimum of 26 contact hours for family-
based behavioural weight management interventions.
Changing Lifestyle habits that are deeply rooted in cultures and different regions can
be really tough and expensive. Moreover Obesity and Overweight treatment expenses
are usually not covered by any Insurance companies. These pose as barriers to
treatment and training both.
• 10.William H. Dietz and Steven L. Gortmaker, [20] in a review article, write
“families and schools represent the most important foci for preventive efforts
in children and adolescents. Anticipatory guidance by pediatricians may offer
an effective mechanism by which to change parental attitudes and practices
leading to change in sedentary habits like television viewing which affect both
energy intake, and energy expenditure.”
According to the data provided by the National Health Surveys II (1980) and III
(1994) NHANES; the number of children and adolescents considered overweight,
defined as a body mass index (BMI) equal to or > 95th percentile for children of the
same age and gender, had increased by 100% in the United States. At the time of the
survey III, 10-15% of children and adolescents were found to be overweight.
Substantial weight increase was found in all age,gender, and ethnicity groups](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-44-320.jpg)

![47
appropriate strategy is not to purchase these foods, rather than to have them in the
house and restrict access to them.
ix) Another strategy should focus on ways to increase physical activity as part of daily
routine of children and adolescents.
x) Next, the article covers some school based strategies, which we are not covering in
our study.
We selected this study to include in ours, for various reasons. Firstly, it is a very
important study based on a National Health Survey of U.S.A, as well as on the
comparison of the data of the latest survey with the data of National Health Survey
done 15 years ago.
Secondly, It brings home very important issues related to our study. It focuses on
counseling of parents to prevent and control primary and secondary overweight and
obesity.
Thirdly, the study also mentions the issues to be taken up for counseling the
parents, by health personnale, or pediatricians.
• 11. Meghan l. Reubal, Kate A. Heelan, Todd Bartee, and Nancy Foster, in their
original research ,(2011)[21] observed, that children and their parents lost
significant body mass after an intervention of 12 weeks. There were also decreases
in the child participants’ intake of high fat, high calorie foods. They concluded that
family based pediatric obesity programs may offer significant benefits and lead to
healthier lifestyles for obese children and their parents. (22)](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-47-320.jpg)








![57
if only they have the right knowledge about it. obesity in children and how they can
help their children lead a healthier life.
Now let us look at some Indian Studies related to our Topic:
12. Medha Mi
tt
al, and Vandana Jain, (2021) [7]: in their review ar
ti
cle, found that the
mainstay of management of Obesity and its complica
ti
ons in children and adolescents is a
holis
ti
c lifestyle modi
fi
ca
ti
on that must be adopted by the family. It involves dietary changes,
regular physical ac
ti
vity, and behavioural changes that favour a healthy way of life. Regular
follow-up, and a
tt
en
ti
on to keeping up the mo
ti
va
ti
on of the child and family achieves good
results.
The ar
ti
cle presents a stepwise approach to preven
ti
on and management of overweight and
obesity in children and adolescents, adapted to the Indian scenario.
Since our focus here is on parental counseling and the role of parents in the control, we may
remain focused to our topic and may not give details of other management steps men
ti
oned
in this ar
ti
cle. The authors have suggested a stepwise approach similar to the 2007
guidelines given by The American Academy of Pediatrics, but contexualized to our se
tti
ng as
in India.
Firstly, they take up the Level 1: Preven
ti
on of Overweight /Obesity and Management of
Overweight without Complica
ti
ons. Keeping in mind the phrase,’Preven
ti
on is be
tt
er than
cure’, the authors recommend key strategies to be ins
ti
tuted early and con
ti
nued through
childhood and adolescence. Any child who is crossing the percen
ti
le lines needs close
observa
ti
on and monitoring.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-57-320.jpg)


![60
crucial motivation. The pediatrician has the overall responsibility of guiding the family and
the child, along with a dedicated multidisciplinary team. Pharmacotherapy has limited role
and bariatric surgery may be an option for those with severe obesity or significant
complications, refractory to diet and lifestyle modification.
We selected this article on guidelines on prevention and management of overweight and
obesity in children and adolescents, because:
It is a study conducted in a premier research Institute of our country AIIMS Delhi, and
research quality they follow is stringent and of high standards.
Moreover, the guidelines prepared by the premier Institution regarding prevention and
treatment of overweight as well as obesity, clearly highlight the importance of family
involvement, and parental counseling at every level.
The authors summarise the article as follows:
It reaffirms our belief that parents have an important role to play in controlling overweight
and obesity in children and adolescents, and that all health care providers should be made
aware of it, and start to counsel parents as soon as possible, to prevent overweight or obesity
in the child population, which seems to be rising to enormous proportions rapidly!
• 13. Sheila Bhave, Ashish Bavdekar, Madhumati Otiv, IAP National Task Force for
Childhood Prevention of Adult Diseases: Childhood Obesity: (2004), [8]observed that,](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-60-320.jpg)


![63
foods or drinks. Counseling of parents also comes in when and how to reduce the sedentary
activities of their children.
In fact Sheila Bhave et al, conducted a school based study with controls, and followed up the
participants over a 5 year period. They faced many problems, as to limited size of school
grounds for activities, academic curriculum pressures to restrict their counseling sessions to
students and teachers, they could provide healthy food to only those who did not bring tiffins,
and had to remove all hawkers from outside school premises, change the kitchen pattern of
school canteen, but after a period of 5 years, although some change was noticed in waist
circumference of participants, overall there was no significant decrease in BMIs. This again
shows that involvement of parents and regular counseling of parents regarding healthy foods,
and physical activities by healthcare providers is essential. This can be done by the school
teachers too.
• 14. Anjali Mahajan, Prakash C. Negi, Sunita Gandhi, Dinesh Sharma, Neelam
Grover, : (2022) [22] conducted a school based cluster randomized study, to study the
‘Impact of School based Health Behavioural Intervention on Awareness, Practice Pattern of
Healthy Lifestyle, and Cardiometabolic Risk Factors among School Children of Shimla’
where they studied 3707 students of 13-18 yrs.from 12 senior secondary schools of Shimla,
over a period of 10 months; and trained teachers to impart health and nutrition related
knowledge to adolescents to control overweight and obesity. The Intervention was. Found
to be ineffective in improving the knowledge and food habit scores after adjusting for
cluster level baseline measures. Physical activity was slightly found to have increased after
intervention, but it did not differ significantly from the control groups. Secondary outcomes
such as anthropometric measurements and biochemical profile also did not differ in the two](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-63-320.jpg)
![64
groups, except for low density lipoprotein (LDL) cholesterol, which was significantly less
in the intervention groups. The Intervention also did not have any significant effect on
physical activity levels and screen time.Many other studies have also reported similar
results.
We have taken reference of these school based, evidence based, Indian intervention Studies
here, to bring home the point, that so much work and community and social work is done
by healthcare providers and policy makers at the school level, but significant results cannot
be seen by studies. Whereas, involvement and counselling of parents for the same
consistently provides evidence of significant change. This is important and more and more
family based programs should be designed to control this rising epidemic.
Further evidence based carefully planned researches should also be conducted to ensure
easier and more feasible methods of parental counseling at a large scale.
• 15. Sitanshu Shekhar Kar, and Subhranshu Shekhar Kar,(2015) [9] in their review
article “Prevention of Childhood Obesity in India: Way Forward” , wrote that to
effectively address the problem of childhood obesity, a sustained multisectoral response is
required. These strategies should be initiated at home and in pre-school institutions, and
involve health care professionals and non-governmental sectors. Preventing obesity in the](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-64-320.jpg)


![69
Therefore, this important review article confirms our belief that parental
counseling is a very important aspect in controlling overweight and obesity
among children and adolescents.
• 16.Arunachalam Samundeeswari, Kandasami Maheshwari, (2019) [23]
conducted a study which intended to identify the attitude of mothers having
obese children, about the cause and prevention of childhood obesity.
‘Mothers’Attitude on Childhood Obesity and its Prevention’.They felt that
mothers are the primary caregivers and therefore their perception about child
health have a great influence on childrens’ nutrition, and physical activity.
They play a vital role in sculpting the knowledge, behaviour, and attitudes of
their children at early ages; help them in developing eating behaviours,
energy intake and food preferences. They felt that the primary prevention
inevitably involves good obesity related knowledge by parents as well as
proper attitudes leading to appropriate practices. Management of obesity
requires behaviour change including diet and physical exercise, or activity.
These are possible by health care professionals, and families who provide
adequate support and reinforcement of healthy lifestyles among children and
can help parents recognize obesity as a risk factor for future diseases in
children. The lack of knowledge of parents on childhood obesity presents a
challenge to any intervention because an underlying cause of poor health
(e.g.obesity) might be perceived as manifestation of good health.(23)
Materials and Methods used:](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-69-320.jpg)

![74
It signals, that healthcare providers need to give certain interventions like
counseling for both, child and parent, family based, school based intervention
program on healthy lifestyle practices and its importance.
We selected this study for our research purpose because it answers our main
research question: Can parental counselling help in controlling overweight and
obesity in children and adolescents?
It is a well planned, validated research, which helps to bring home the point
that parental counselling, which would be focused on enhancing their
knowledge and attitude towards healthy eating practices and living a healthy
lifestyle, and being a role model for their children at home regarding a healthy
lifestyle, can go a long way in controlling overweight and obesity in children
and adolescents in our country.
The study also shows that at parental knowledge and attitude towards this
rapidly increasing health problem is only moderate and they are confused over
various issues and do not realize the long term risks associated with this. This
study, therefore helps us to reinforce the importance of parental counselling in
controlling overweight and obesity in children and adolescents.
• 17.Rajesh Sagar, and Tanu Gupta, (2018) [24], in a review article
‘Psychological Aspects of Obesity in Children and Adolescents’ reviewed
various studies on psychopathology of obese children and adolescents. In the
Indian context they found that many studies highlighted the increased
prevalence of childhood obesity in India, however, very few studies target](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-74-320.jpg)















![101
Chapter-4
RESULTS & DISCUSSION:
Original Research Papers or Randomized Control Trials:
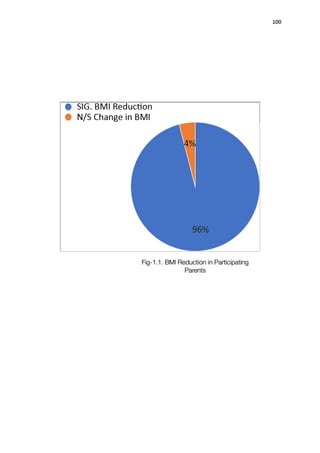
1. Reubal M et al, [21]‘ Outcomes of a Family based Pediatric Obesity Program-
Preliminary Results’ : BHF program, or the Building Healthy Program, had 22
participants of age group 7-12 years. They also had 20 mothers and 20 fathers as
participants. After 12 weeks , they found 72% children had decreased BMI scores,
96% parents had also decreased their BMI scores. The average weight change in
children was 4.52+- 3.82%, and that in the parents was 7.39=- 2.27%.
The study also found the z scores in children had decreased significantly. Also body
mass and fat percentage was also calculated in this study and these also decreased in
both children as well as parents.
The 12 week Intensive Intervention consisted of ;
-weekly sessions of Behaviour Modification
-Nutrition Education](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-101-320.jpg)
![102
-Family Lifestyle physical activities for 1.5 to 2 hours a week
-They encouraged participation by the entire family.
They concluded that the success of this study demonstrated that it is essential for the
entire family to be involved, so as to create an environment to support healthy
behaviours at home too.
Parents are typically targeted because they are the most influential to a child’s dietary
habits, as well as levels of physical activity; and this has been proven by numerous
studies now, as well as in ours.
This study also focused on the variables which are important to weight loss, as
different studies present variable amount of change.
Inclusion of this study in our research therefore strengthens our belief that Parental
Counselling has a very important role to play in controlling overweight and obesity in
children and adolescents.
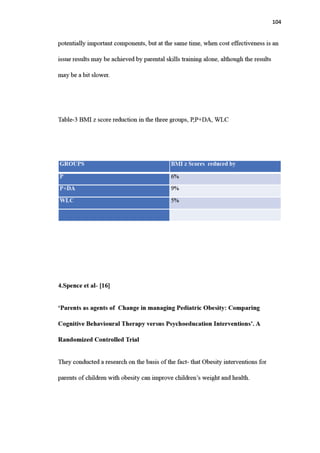
2.Golley.R et al, [13]‘Twelve month effectiveness of a parent led, family focused
weight management program for prepubertal children’ conducted in Australia,
had 111, participants out of which 64% were females. They all were overweight
prepubertal children 6-9 years of age.
The Measures used were: Parenting skills training, and intensive lifestyle
education(P+DA)Or parenting skills training alone (P); or a third group was of a](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-102-320.jpg)

![105
They evaluated whether a parent based intervention based on CBT principles was
superior to a parent based intervention based on Psychoeducation Programme PEP.
We included this study , because it was based on parent based interventions, and to
control the psychological problems it is imperative to control weight and obesity.
The study included 52 participant obese children of mean age 9.8 years, with a
baseline BMIz score of 2.2 (0.3).
The participants in CBNT group were n=27, and the PEP group n=25. The BMI z
scores in the two groups were similar at 0-4,10-,16- month follow up.
At 4 months, the BMI z scores had significantly reduced in both the groups, as
compared to the baseline- CBT- (-0.05,95% Cl=-0.09 to 0.00) and PEP (0.04, 95%
CL=0.09 to 0.01) The mean difference between the two groups was -0.01 (95% Cl=
-0.08 to 0.06, p=0.80). Similar results were found across all secondary outcomes.
Both therapies showed equal results at the scheduled follow ups.
As concerned with our research, this study shows that parental counselling is not only
effective in helping children and adolescents to reduce their weight, but also has a
very important role in managing the psychological and behavioural complications of
obesity. Any of the two therapies can be used CBT or PEP, both being equally
effective.
• 5. Brown A, et al [14] ‘ Prevention and Treatment of Overweight in Children and
Adolescents’, conducted a Review Article . They found that school-based
prevention programs are generally not successful in reducing the prevalence of](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-105-320.jpg)
![107
➢ The treatment program should help the family make small gradual changes
➢ The treatment program should include learning to monitor eating and activity
➢ A variety of experienced professionals can be involved in the weight
management program. (Adapted from permission from Barlow SE, Dietz WH.
Obesity evaluation and treatment: Expert Committee Recommendations.The
Maternal and child Health Bureau, Health Resources and Services
Administration and the Dept of Health and Human Services. Pediatrics
1998;102:E29(7)
• 6 Kothandan S et al, [6] describes in his review article that, 13 articles which met
the criteria from 1231 ; eight were Family based interventions (n=8), and five were
school based (n=5), with total participants (n=2067). The participants aged between
6-17 years, and the study duration between 1 month to 3 years. They found after a
systematic review that the family based interventions demonstrated effectiveness for
children under the age of twelve; and School based interventions were most
effective for children in 12-17 age group with differences for both long term and
short term results.
This study further strengths our belief that family based interven
ti
ons have a very
important role to play in decreasing weight in children and adolescents. This study
came out with an amazing
fi
nding which could not be seen in other studies we went
through. Children above 12 years were seen to responding be
tt
er to school based
interven
ti
ons. This is an interes
ti
ng fact and can be explained on the basis of
adolescent con
fl
ict with parents and more in
fl
uence of peers and teachers on them.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-107-320.jpg)
![108
If it is indeed so, this fact needs further research and could be u
ti
lized in weight
reduc
ti
on programmes in future !
• 7. Rattanamanee.K and Chintana Wacharasin, [5] in their Quasi experimental
study, ‘Effectiveness of a Family Based Behavioural Counselling Program among
school aged Children with obesity’which was conducted for 7 weeks; found that the
group I which received a Family based counselling program, had significantly better
healthy eating habits at the end as compared to Group II which received group
based counselling; and also when compared to Group III which received only a
usual program. The findings indicated that this Family based program could
enhance healthy eating bahaviour and physical activity and decrease BMI in
children with obesity.
• 9. Guidelines by the Guideline Development Panel for Treatment of Obesity,
American Psychological Association (2020) [15], ‘Multicomponent Behavioural
Treatment of Obesity in Children and Adolescents’; in this article we found, that
based on Systematic Review conducted by Kaiser Permanente Research Affiliates
Evidence based Practice Center, these recommendations were issued with
intentions for guiding Psychologists, Health and Mental Health Professionals,
Patients, Families, as well as Policy Makers, engaged in taking care of overweight
and obese children. The criteria they used for selection was BMI and BMI z scores
The GDP strongly recommended that children 2-18 years should receive Family
based, Multicomponent, Behavioural Intrventions., for controlling overweight and
obesity in children and adolescents. The minimum contact time should be 26 hours
with parents, These measures should be initiated at the earliest age possible](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-108-320.jpg)
![109
The above guidelines once again highlight our research topic : Role of Parental
counselling in controlling overweight and obesity in children and adolescents.
10.Janicke.D et al[17,18] in their Systematic Review and Meta analysis of 20
studies which were randomized Controlled Trials (RCT) analysed the
‘Comprehensive Behavioural Family Lifestyle Interventions Addressing Pediatric
Obesity (CBFLI)’. The participants in the studies were 1671. The results of this
analysis were as follows:
The overall effect size for CBFLI as compared with passive control groups over all
time points was statisticallysignificant (Hedge’s g=0.473), 95% confidence
interval[ .362,.584] and suggestive of a small effect size. Duration of treatment,
number of treatment sessions, the amount of time in treatment, child age,format of
therapy (individual vs group), form of contact, and study of intent to treat analysis
were all statistically significant moderators of effect size.
They concluded that CBFLI demonstrated efficacy for improving weight outcomes in
youths who are overweight or obese. The article analyses that “ Parents are often
considered a critical agent of change in behavioural lifestyle interventions, as they
exercise significant control over children’s eating and physical environment, and
ultimately their behaviours.”
The above statement is more true for our Indian Culture where there is a
collesctivistic culture and interdependence till late adolescence or even later till
adulthood. The Comprehensive program is given in detail in material and methods.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-109-320.jpg)
![110
11. Kelishadi R , Azizi- Soleiman F, in their Systematic Review on ‘ Controlling
Childhood Obesity: Strategies and Challenges’, conducted in Iran, [18]; agreed that
the epidemic proportion of childhood obesity is no more limited to developed
countries only and is rapidly engulfing the developing nations too.
Studies were included if they were conducted on 2-18 year old children, community,
family, school, and clinical interventions or, a combination of them, English language,
and conducted among obese or overweight children and adolescents.
They had 30 articles from school based programs, 26 family based articles.
The school based studies showed positive impact on eating and activity behaviours,
but could not elicit significant change in BMI levels.
The Family based programs found, that family is an applicable target for promoting
health care interventions. They found that engaging parents in childhood obesity
prevention programs will make weight loss easier for children, because they are the
agents who can provide conditions to help their children to choose healthy
behaviours. They are also important role models for their children.
It was found that parents find it difficult to accept that their child is overweight,
therefore they do not comprehend the necessity of obesity prevention.
The review studied n=26 family based studies and found that most of these programs
were successful in decreasing body mass index BMI, and BMI z scores, and some
health consequences of overweight too.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-110-320.jpg)
![111
overall, all the studies conducted in family setting had favourable results on obesity
criteria. A few had negligible effects, but it was probably because these studies did not
follow up for a longer period.
This study helped us to understand that not only in developed countries, but also
developing countries are being engulfed with this problem as is our own country,
India. This article also took up many studies and included three different methods of
interventions. It came out that involvement of the family is by far the time tested
method out of the three and should be pursued consistently in all countries. Clinic
based methods were very varied and did not provide with any consistent results, so
they are not being taken up in more detail here.
• 12.Kirsten Weir, authored a review article ‘ Family Based Behavioural Treatment
is Key to Addressing Childhood Obesity’. [19]The author writes that Wilfley and
Raynor were among a panel of obesity experts who developed a new Guideline for
American Psychology Association (APA) March 2018. Clinical Practice Guideline
for Multicomponent Behavioural Treatment of Obesity and Overweight in Children
and Adolescents. After reviewing all literature the panel found strong evidence to
recommend family based behavioural interventions, to treat obesity in children 2-18
years old. They focus not only on the children but the whole family to engage in a
healthier lifestyle by improving the diet, physical activities and by reducing
sedentary behaviour. They also focus on behaviour change, teaching strategies to
parents for goal setting, problem solving, monitoring their childrens; behaviours,
and also by modelling positive parental behaviours.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-111-320.jpg)

![113
• 13.Steven L Gortmaker, and William H.Dietz: [20] authored a Review Article in
which they addressed the natural history of obesity in children, the most promising
family based and school based approaches to its prevention, as also the barriers and
opportunities associated with secondary prevention. Their study showed that 60% of
the obese and overweight children above 5-10 years age, already had associated
cardiovascular disease risk factor, such as hyperlipidmia, elevated blood pressure,
or hyperinsulinemia. Also, 20% had two or more cardiovascular risk factors. The
incidence of Type II Diabetes had also increased dramatically among youth, which
until recently was thought to be an adult onset disease.
We selected this study to include in ours, for various reasons. Firstly, it is a very
important study based on a National Health Survey of U.S.A, as well as on the
comparison of the data of the latest survey with the data of National Health Survey
done 15 years ago.
They developed a logic model for Family based approaches to prevent primary or
secondary obesity in children and adolescents. The details of this model have been
given in detail in the materials and methods section.
Most of these approaches advise active involvement of parents in helping the
children, for which the parents need counselling and guidance at various levels so as
to implement them successfully and sustain the results over long term periods. This
involves a lifestyle change in eating, playing, sedentary and many other day to day
activities.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-113-320.jpg)
![114
This study brings home very important issues related to our research and strengthens
our research that parents have an important role to play in controlling and preventing
overweight and obesity in children and adolescents.
This study also gives us details of the issues to be taken up for counselling the
parents, by health personnale or pediatricians.
• 15. Indian Studies :
• Medha Mittal and Vandana Jain, ‘ Management of Obesity and its Complications
in Children and Adolescents’. [7]A review article found that
The mainstay of management of Obesity and its complications in children and
adolescents is a holistic lifestyle modification that must be adopted by the whole
family. It involves dietary changes, regular physical activity, as well as behavioural
changes that favour a healthy way of life. To achieve good and longterm results it is
essential to followup the cases regularly, and keep up the motivation of the child and
the family as a whole.
The article presents a stepwise approach to prevention and management of overweight
and obesity in children and adolescents, adapted to the Indian scenario, based on an
approach similar to the guidelines given by The American Academy of Pediatrics, but
contextual to our setting as in India. The guidelines involve the parents at all levels
namely- Individual and Family level steps; Physical activity; Behavioural
interventions. According to this study, family involvement and role modeling by](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-114-320.jpg)
![115
parents provide the crucial motivation required by the child.The Pediatrician has the
overall responsibility of guiding the family and the child, through these steps, along
with the help and support of a multidisciplinary team. Pharmacotherapy has limited
role and bariatric surgery may be an option for those with severe obesity or significant
complications, rfractory to diet and lifestyle modification.
The study was conducted in a premier institute of India, responsible for issuing
important guidelines for healthcare workers as well as population in general.
The authors concluded their study as follows: “It reaffirms oue belief that parents
have an important role to play in controlling overweight and obesity in children and
adolescents, and that all healthcare providers should be made aware of it, and start to
counsel parents as soon as possible, to prevent overweight or obesity in the child
population, which seems to be rising to enormous proportions rapidly!
This study further adds strength to our research topic about the important role of
parents in controlling and preventing overweight anf obesity in children and
adolescents.
• 16. Sheila Bhave, Ashish Bavdekar, Madhumati Otiv,: (2004)[8]‘IAP Taskforce
for Childhood Prevention of Adult Diseases: Childhood Obesity’ agreed that India is
in the midst of an escalating epidemic of lifestyle disorders associated with
childhood obesity.](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-115-320.jpg)
![117
This Indian study and guidelines support our research topic that parents really do have
an important role to play and involving them can keep the child motivated, as well as
create a desired environment for the child in all the fields- that of Diet, Food choices,
physical activities and resources for them, and behavioural modifications.
• 17. Anjali Mahajan, et al, [22] who conducted a Cluster, randomized, Intervention
,school based study ‘ Impact of A School Based Health Behavioural Intervention on
Awareness, Practice Pattern of Healthy Lifestyle, and Cardiometabolic Risk Factors
among School Children of Shimla’, where they studied 3707 students of 13-18 years
from 12 senior Secondary schools of Shimla, over a period of 10 months. They
trained teachers to impart health and nutrion related knowledge to adolescents to
control overweight and obesity. The intervention was found to be ineffective in
improving the BMIs and no significant change could be elicited at the end of the
study.
Although improved knowledge of students could be seen regarding healthy food
choices and nutrient value of foods, the implementation in preparing such foods at
home could not be enforced as mothers were not involved in the program, school
activities even though doubled could not elicit results, as at home the environment
continued to be sedentary, with no active and safe places for them to play after school,
or due to lack of resources.
This study indirectly supports our research topic as few other school based studies
also do. Thes are studies conducted in India, and similar results are seen from other](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-117-320.jpg)
![118
countries too. Except for one study which found that children above 12 years
responded better to school based interventions; and needs further research on larger
samples. This is important because if school based studies started showing results it
would be more cost effective and a faster method to deliver interventions to
adolescents who are the future of India.
• 18. Sitanshu Shekhar Kar et al, (2015)[9], in a review article ‘Prevention of
Childhood Obesity in India: Way Forward;’found a study that was conducted among
24,842 school children in India, and discovered that from 2003 to 2005, the
proportion of overweight children had increased from 4.94% to 6.57%. They also
found that according to the IOTF- International Obesity Task Force cutoffs, it was
found in a school based study in India, that prevalence of overweight was 14.4%,
and that of Obesity was 2.8%.
After researching methods of control and prevention of obesity and overweight from
all other countries Australia, Canada, Europe, USA, UK, they came out with certain
points of what India can learn from the developed Nations?
1. Surveillance- Periodic monitoring of nutritional and obesity status of children and
adults
2. Health Education: For all children and their Families
3. Community Mobilization: Information to parents about Nutrition, particularly
mothers, workshops for newly married women, Communications and interventions
to be family centered rather than focused on child alone, start right from the](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-118-320.jpg)
![119
pregnancy by educating the pregnant mother, exclusive breast feeding to be
encouraged as it reduces risk of later obesity,
4. Home based Interventions: Mandatory physical activity of atleast 60 minutes to be
supervised by parents, restricting junk foods storage at home, TV/Computer time to
be restricted by parents to a maximum of 2h/dy
5. School based Interventions
6. Policy Formulation.
Thus it can be clearly seen, that studies in India and guidelines in India are also
focusing on parental role in controlling and preventing overweight and obesity in
children and adolescents. More so, almost all studies we could find could not elicit
and significant results in school based studies but at the same time could present
evidence based data of a significant change when parents were involved in the
interventions.
• 19. Kandasami As,Et Al.(2019)[23] ‘Mothers’Attitude On Childhood Obesity And
Its Prevention’. (An Indian Study)The study was conducted with an intention to
identify the attitude of mothers having obese children, regarding the causes and
prevention of childhood obesity. We included this study, because we wanted to
know how knowledge and attitude of mothers towards overweight and obesity, can
affect the outcome of a healthy lifestyle in children and adolescents. It was
relevant to our study because if the mothers have deficit in knowledge; of](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-119-320.jpg)



![124
Thus we see, that even while trying to manage the behavioural problems, counselling
parents and involving them at different steps is advisable to control and prevent the
behavioural consequences of obesity and overweight.
• Rajesh Sagar, and Tanu Gupta, ‘Psychological Aspects of Obesity in Children
and Adolescents’,is a Review Article found that:[ 24] Many studies highlighted
the increased prevalence of childhood obesity in India, but very few studies target
the mental state of an obese child. The existing Indian Literature does report the
presence of more behavioural problems in obese children as compared to their](https://image.slidesharecdn.com/mcftp002gb-241120044153-a48759c3/85/IGNOU-Sample-Dissertation-File-for-MCFTP002-GB-124-320.jpg)