IDENTIFICATION OF MICROORGANISMS
**Methods for identifying microbes
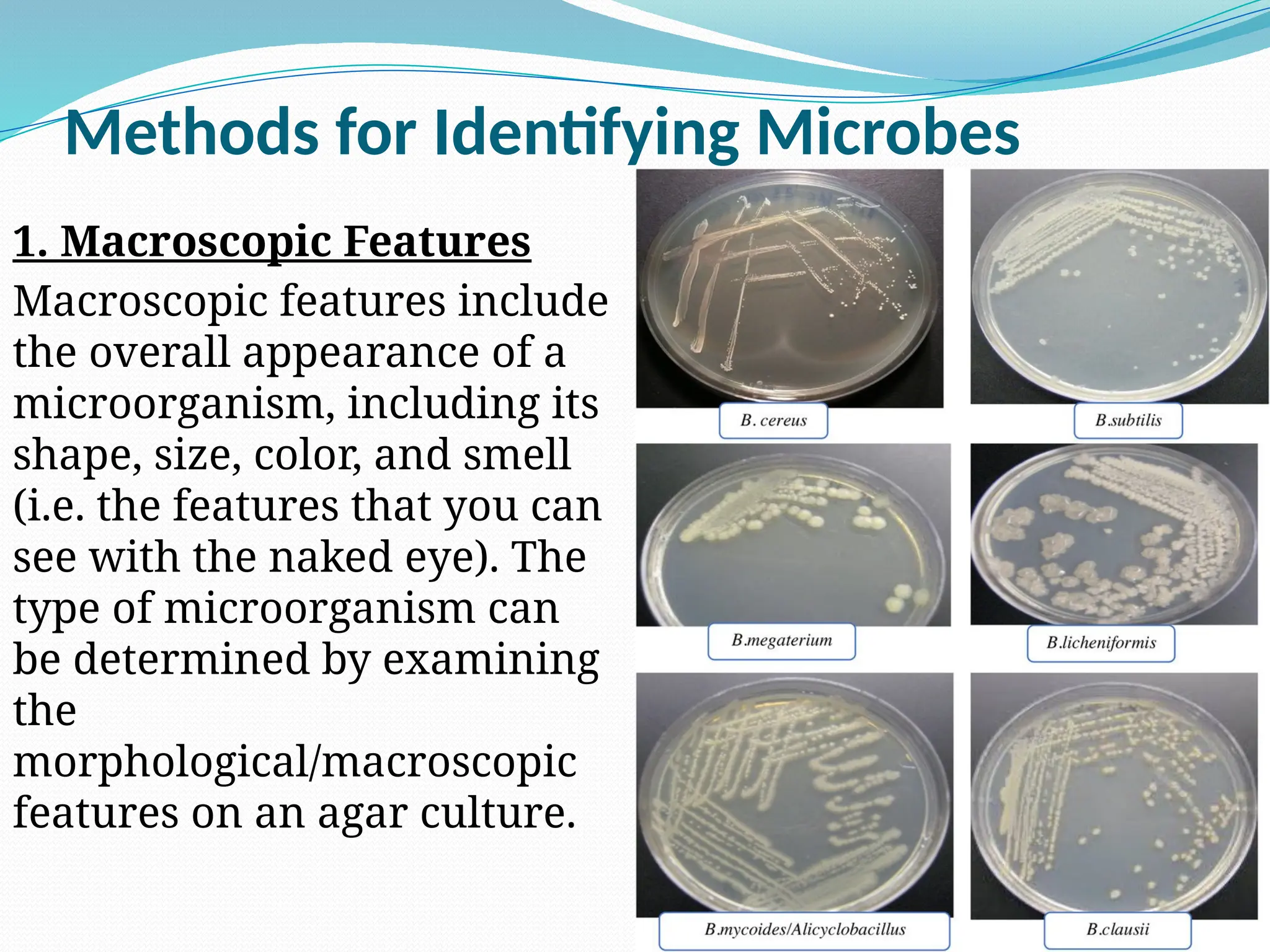
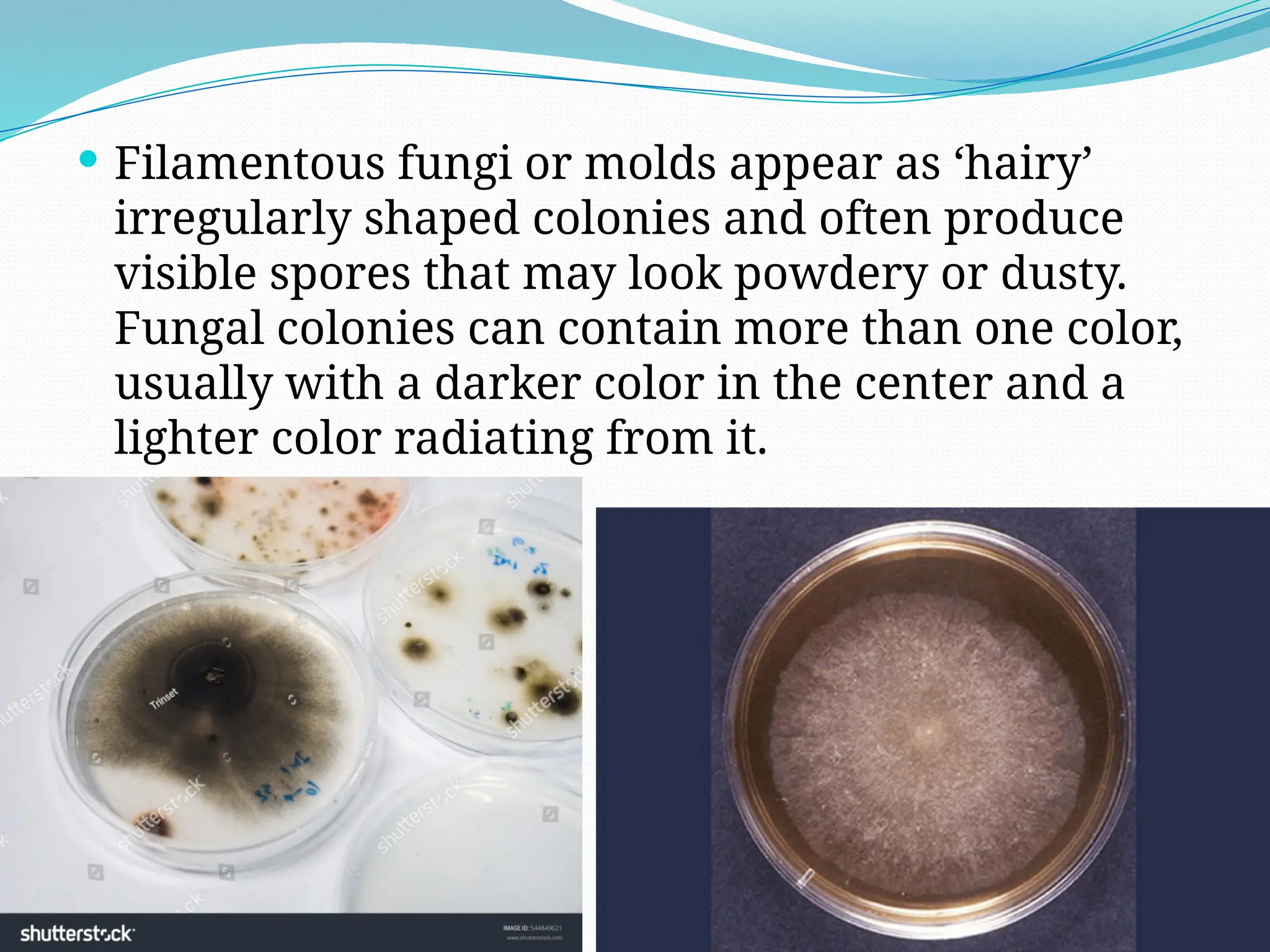
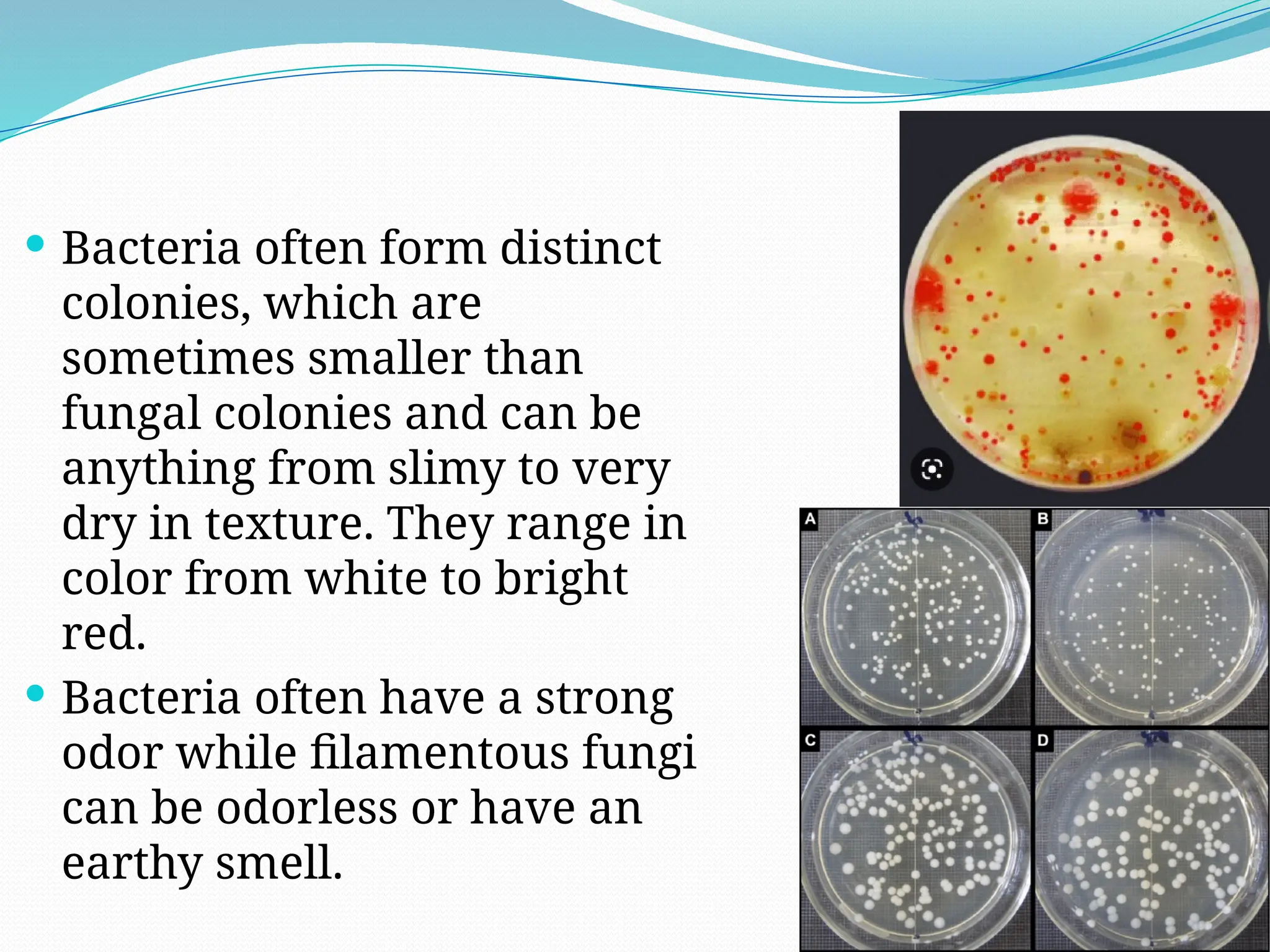
1. Macroscopic Features
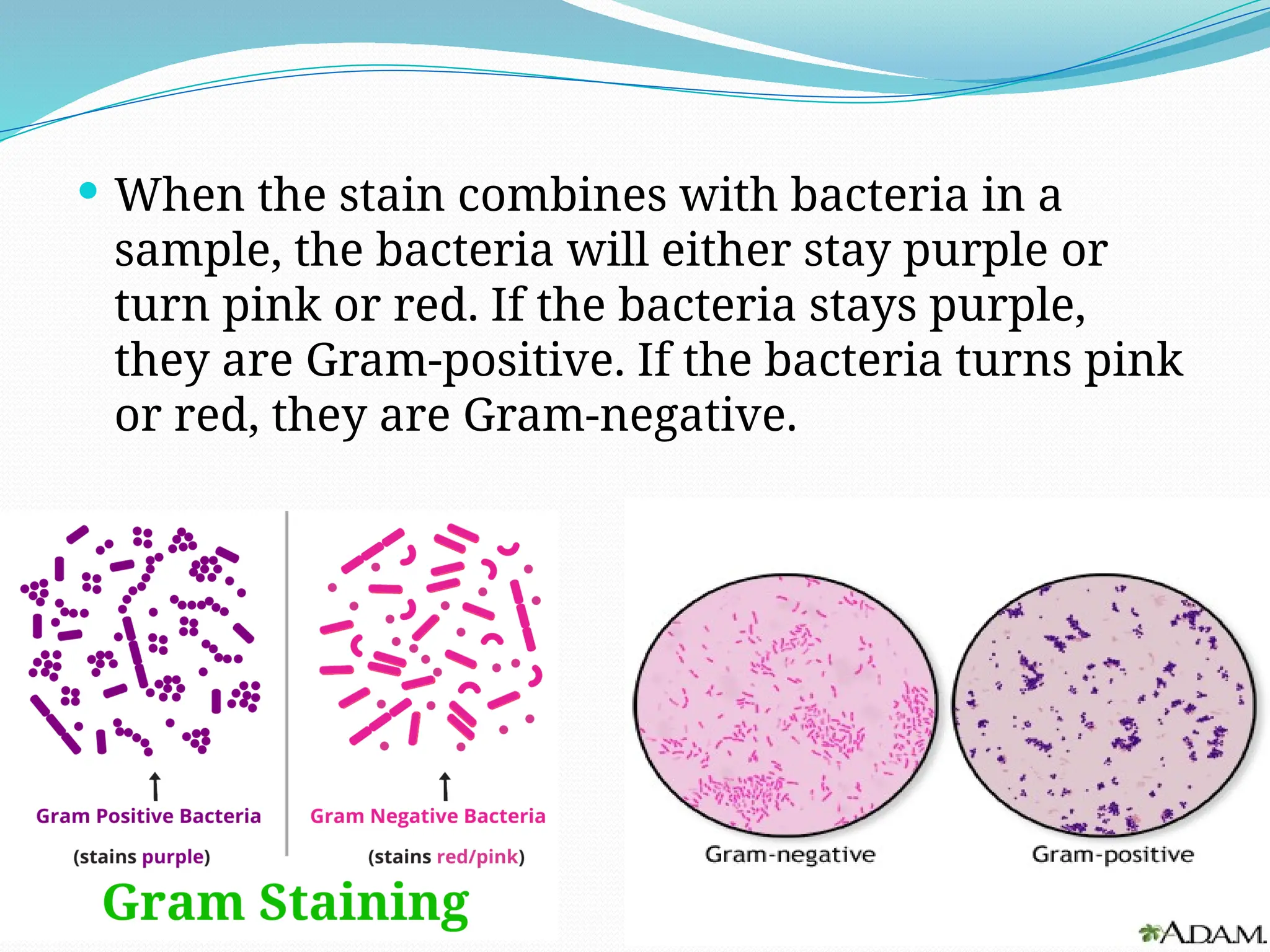
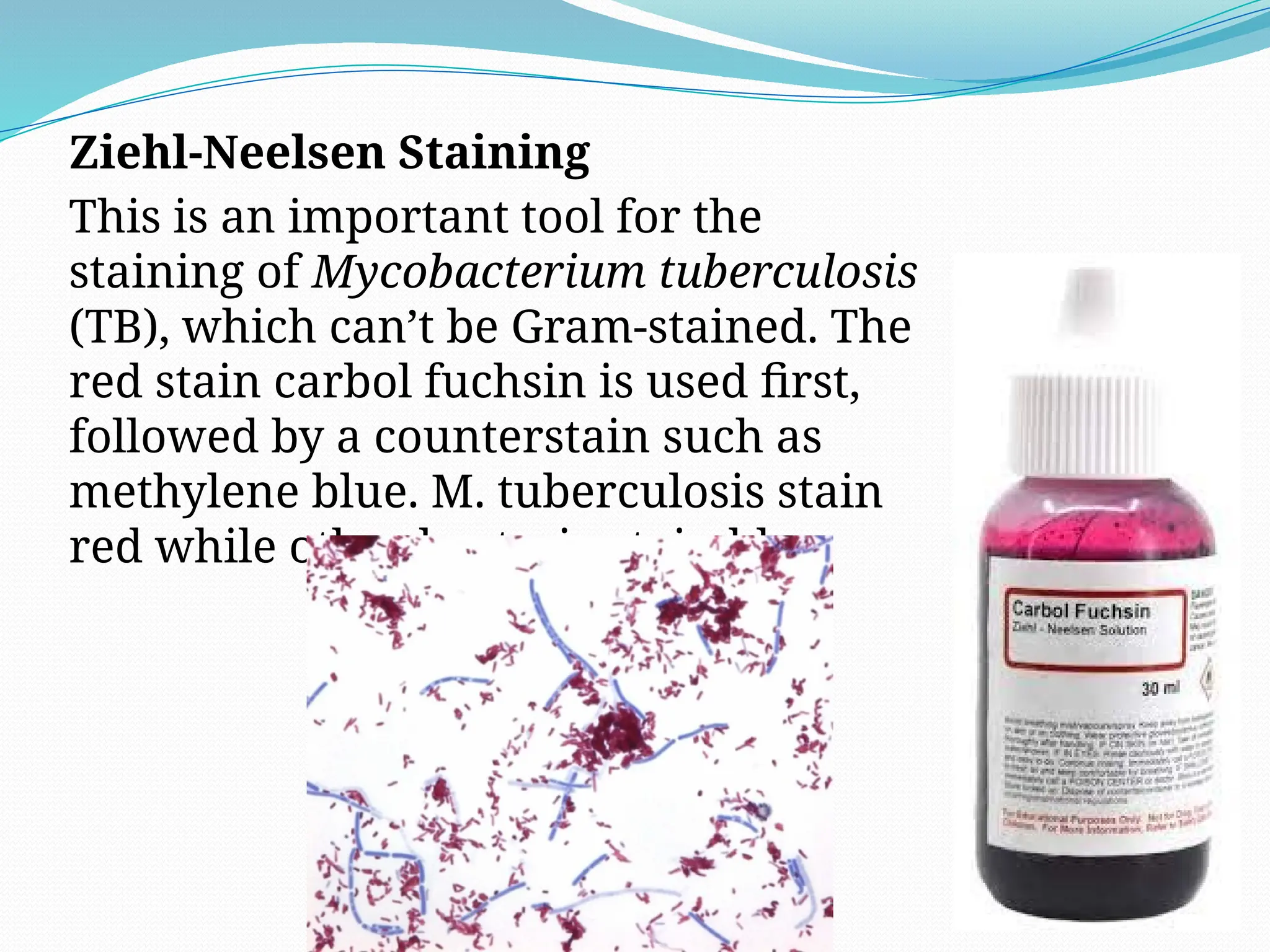
2. Staining and Microscopy (Gram staining, Endospore staining, Ziehl-Neelsen Staining, Stains for Fungi and Yeast)
3. Simple Biochemical Tests (Catalase Testing, Oxidase Testing)
4. Identifying Microbes Using PCR
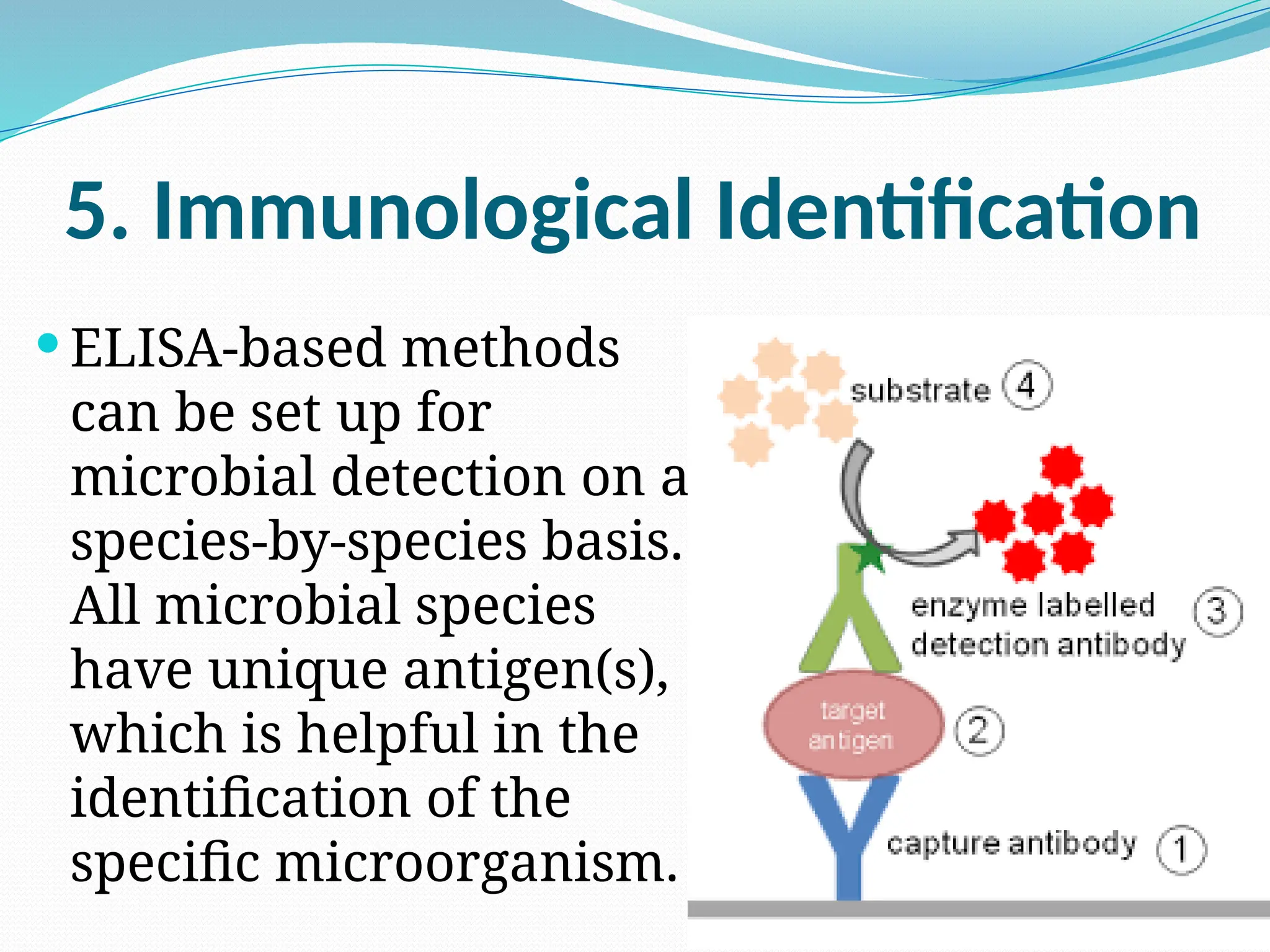
5. Immunological Identification