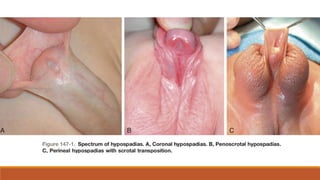
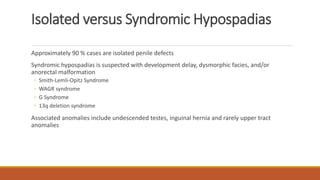
Hypospadias is a congenital anomaly where the urethral opening is on the underside of the penis. It occurs in about 1 in 300 male births and has some genetic factors. Treatment is through surgical urethroplasty to reconstruct the urethra and correct any curvature. Outcomes include some urinary and sexual dysfunction compared to controls, with more issues for proximal versus distal hypospadias. The goal of surgery is a functional penis with normal appearance.