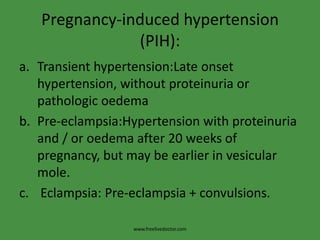
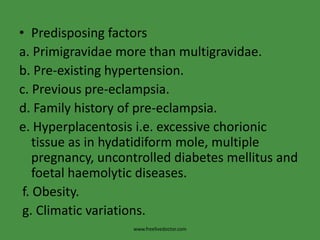
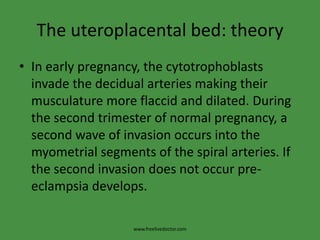
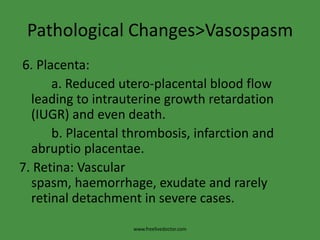
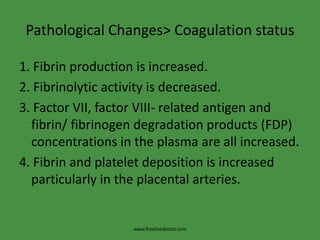
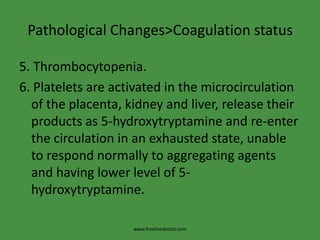
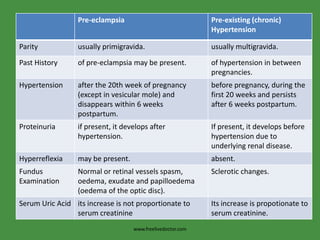
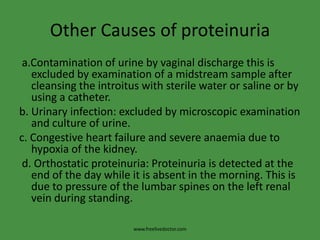
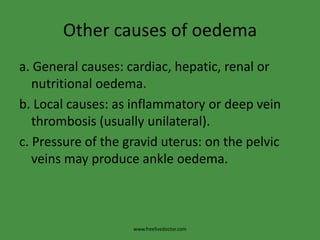
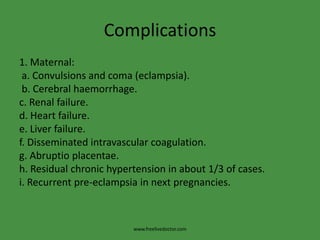
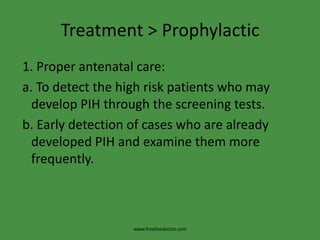
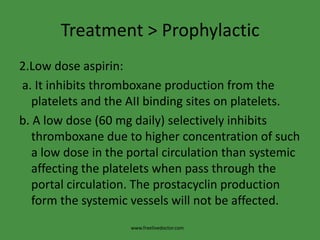
This document discusses hypertensive disorders in pregnancy, including their classification, etiology, pathological changes, diagnosis, and investigations. It classifies hypertensive disorders as pre-existing (chronic) hypertension, pregnancy-induced hypertension (PIH), or superimposed pre-eclampsia/eclampsia. For PIH, it further subclassifies as transient hypertension, pre-eclampsia, or eclampsia. It explores several theories for the etiology of PIH and lists risk factors. Key pathological changes involve vasospasm, coagulation abnormalities, and sodium/water retention. Diagnosis involves signs of hypertension and proteinuria, while investigations include urine analysis and kidney/coagulation tests.