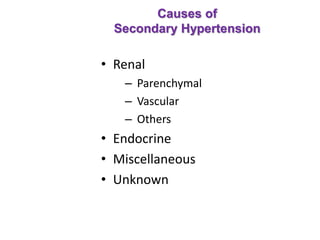
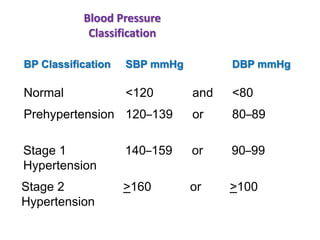
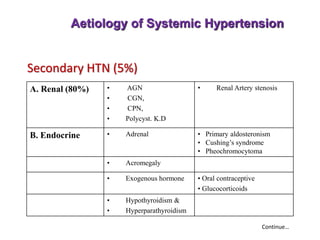
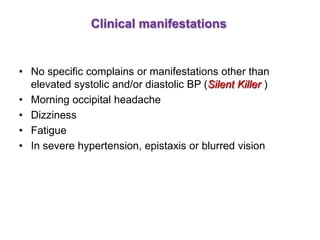
1. Hypertension is defined as a systolic blood pressure of 160 mmHg or higher and/or a diastolic blood pressure of 95 mmHg or higher. It can be essential (95% of cases, no identifiable cause) or secondary (5% of cases, an underlying cause such as kidney, endocrine, or other diseases).
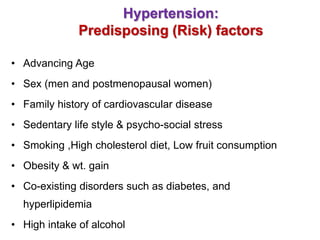
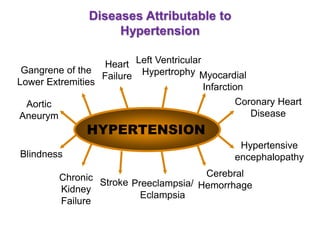
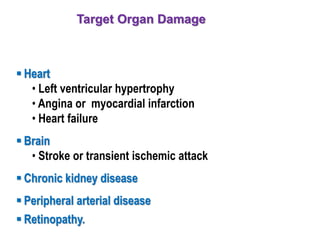
2. Risk factors for hypertension include increasing age, male sex, family history, sedentary lifestyle, smoking, diet high in salt and cholesterol, obesity, diabetes, and alcohol use. Target organ damage includes heart, brain, kidneys, and eyes.
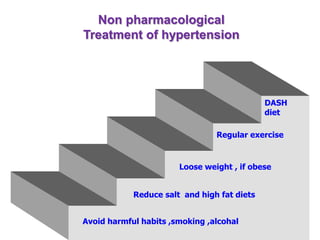
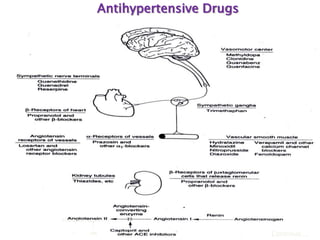
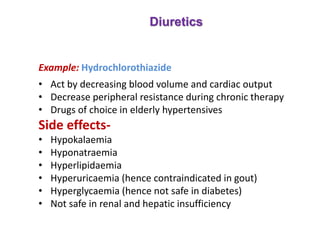
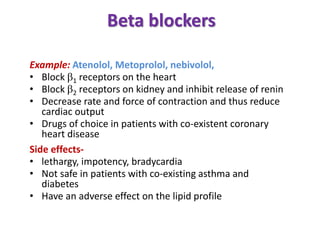
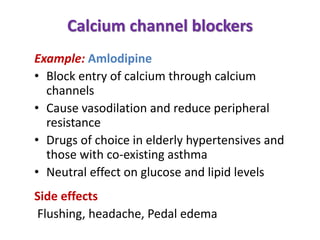
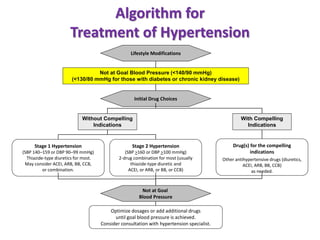
3. Treatment involves lifestyle modifications like weight loss, exercise, diet changes, and limiting alcohol. Medic