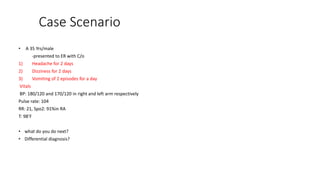
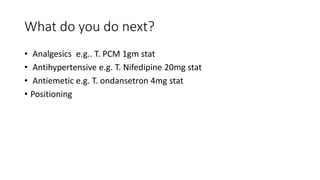
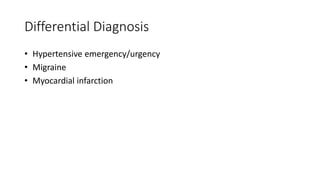
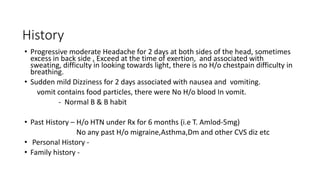
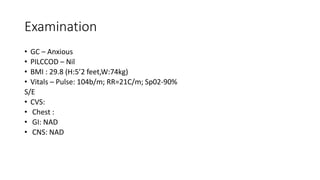
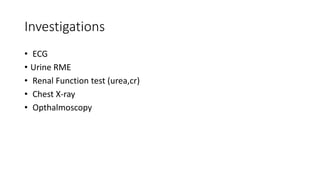
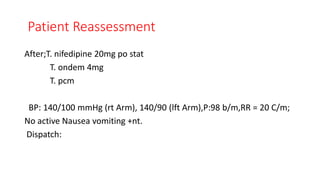
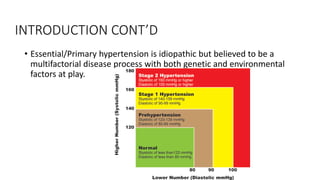
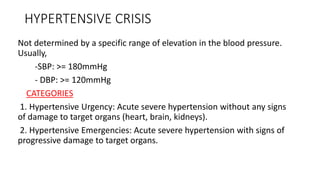
The document details a case presentation of a 35-year-old male with a hypertensive urgency, exhibiting symptoms like headache, dizziness, and vomiting. Initial treatments included antihypertensives and antiemetics, and the provisional diagnosis was supported by investigations such as ECG and renal function tests. Hypertension is classified into urgency and emergencies, with specific management protocols outlined for each category.