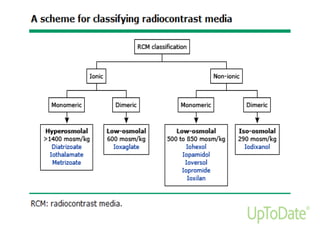
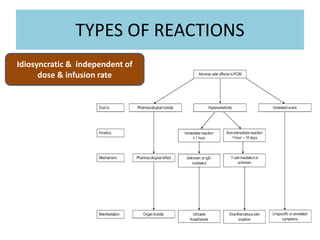
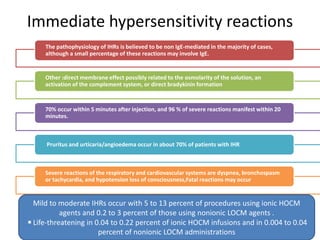
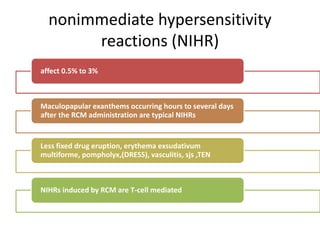
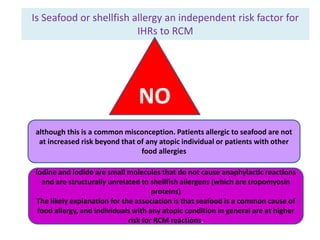
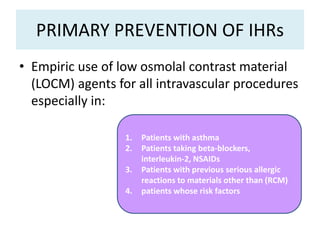
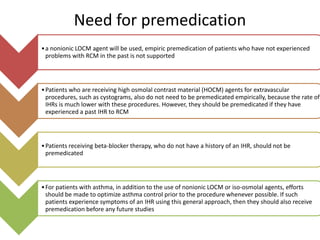
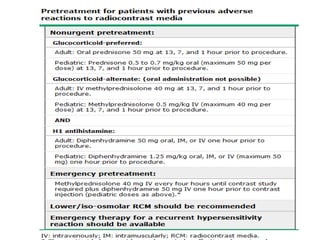
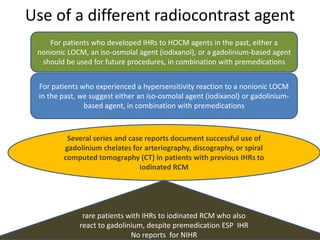
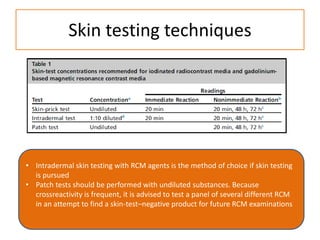
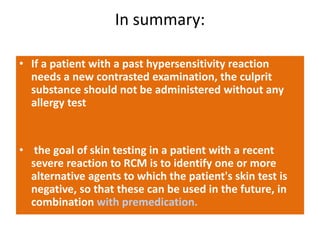
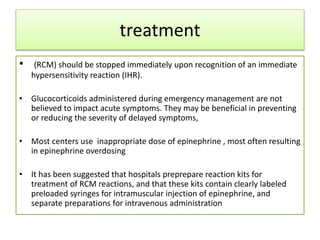
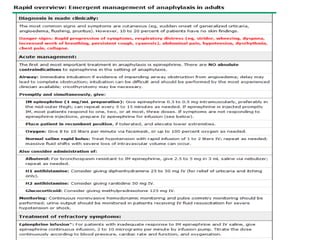
Hypersensitivity to contrast media can occur through immediate or non-immediate reactions. Immediate reactions are usually IgE-mediated and occur within 20 minutes of administration, commonly causing urticaria, pruritus, or respiratory distress. Non-immediate reactions occur hours to days later and are T-cell mediated, often resulting in maculopapular rashes. Risk factors include a history of allergies, asthma, or previous contrast reactions. Low-osmolality contrast agents and premedication can help reduce risk of reactions. Skin testing may help identify safe alternative agents, but provocation testing carries risk and should only be done by experienced allergy specialists.