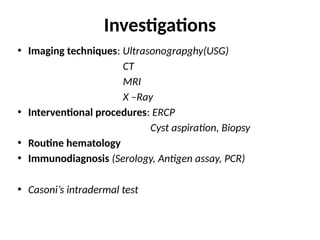
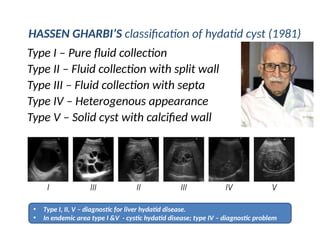
The document details the diagnosis and investigation methods for liver hydatid disease, emphasizing imaging techniques such as ultrasonography, CT, and MRI. It outlines diagnostic classifications and features, along with the importance of routine hematology and immunological tests in confirmation. Various interventional procedures and their indications are also discussed, as well as differential diagnoses and clinical criteria needed for establishing the diagnosis.