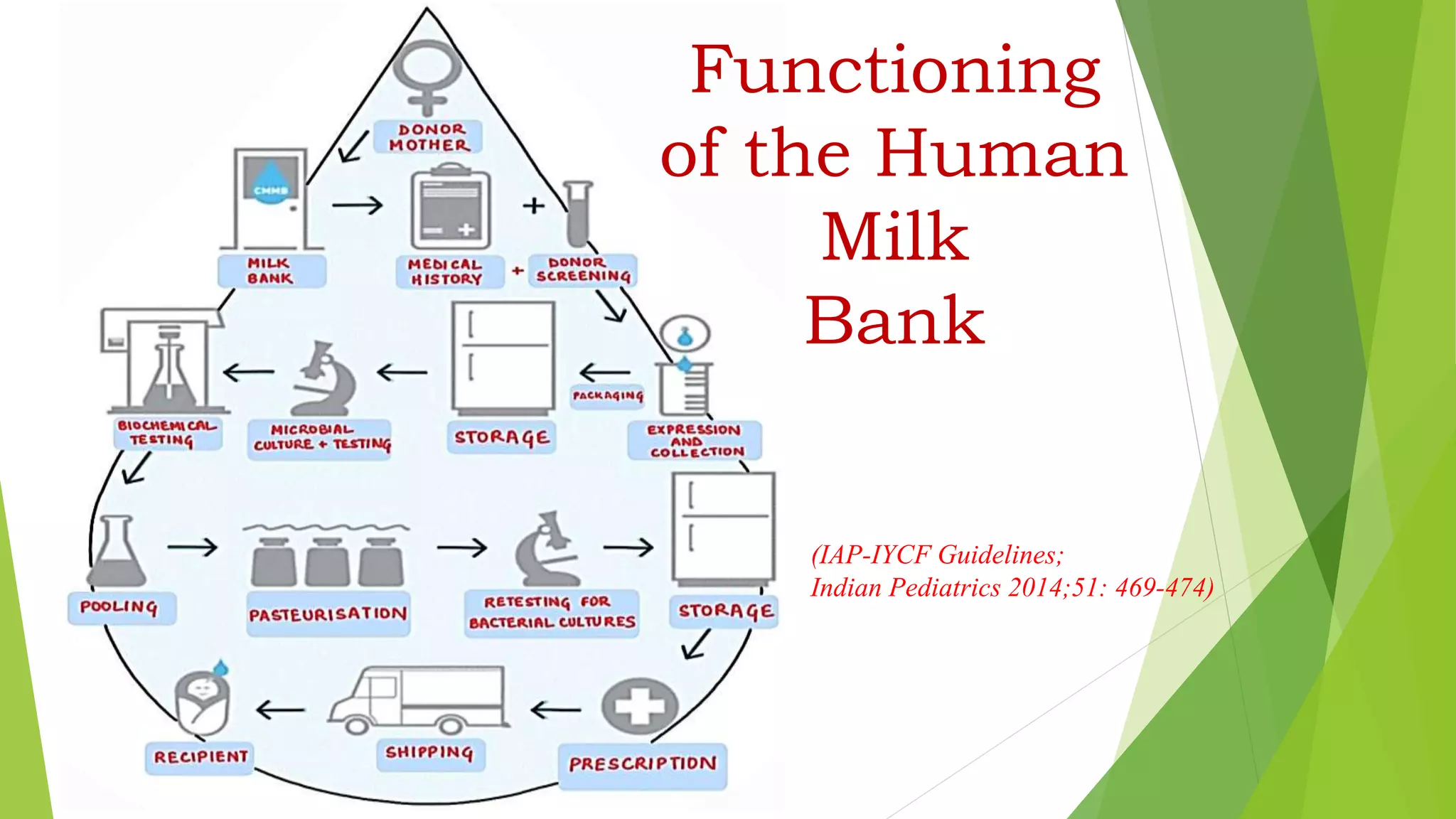
A human milk bank collects, screens, processes, stores, and dispenses donated human milk to infants who need it. Donated milk is preferable to formula or animal milk for preterm and low birth weight babies, as it decreases rates of health issues like necrotizing enterocolitis and improves outcomes. A human milk bank operates by registering and screening donors, collecting and pasteurizing donations, testing the milk, storing it frozen, and distributing it by prescription to reduce risks for recipient infants. Challenges include cost and availability, but human milk banks can improve infant health and reduce long-term costs from issues associated with prematurity.