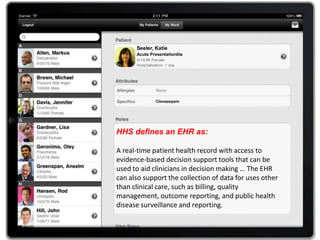
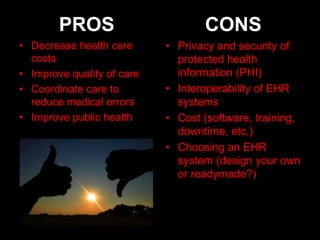
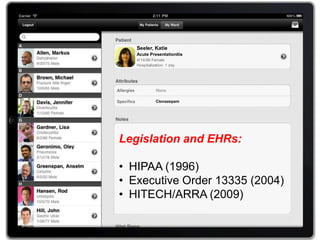
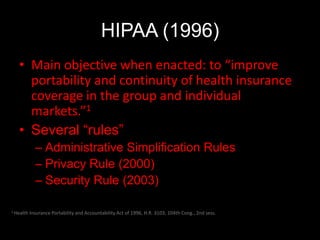
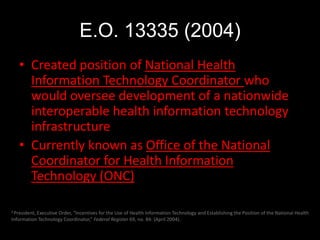
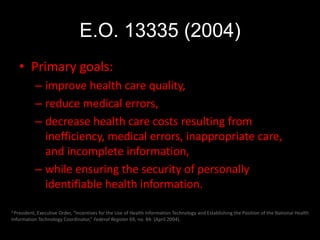
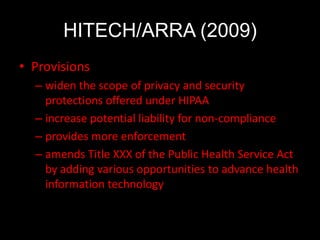
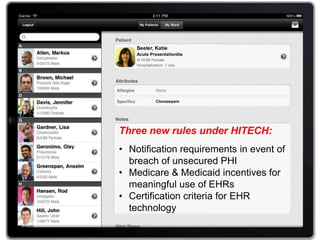
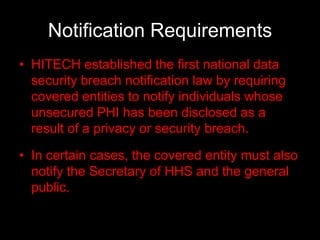
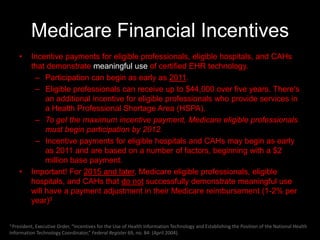
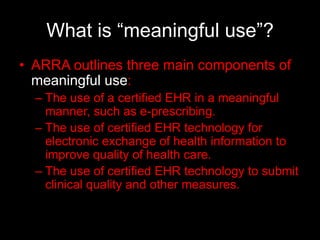
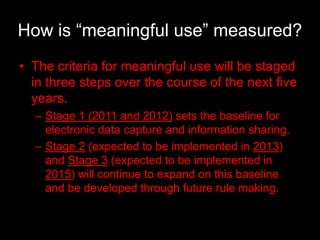
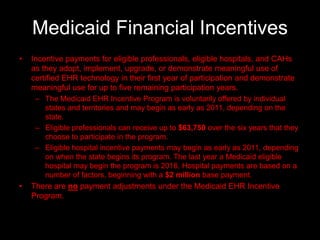
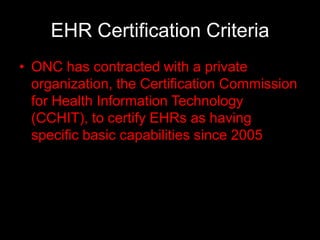
The document discusses electronic health records (EHRs), defining them as real-time health records that support clinical decision-making and data collection for various uses. It outlines pertinent legislation, including HIPAA and HITECH/ARRA, emphasizing goals like improving care quality and ensuring data privacy and security. The document also covers Medicare and Medicaid financial incentives for meaningful EHR use, alongside challenges and questions regarding implementation and the role of EHRs in public health.