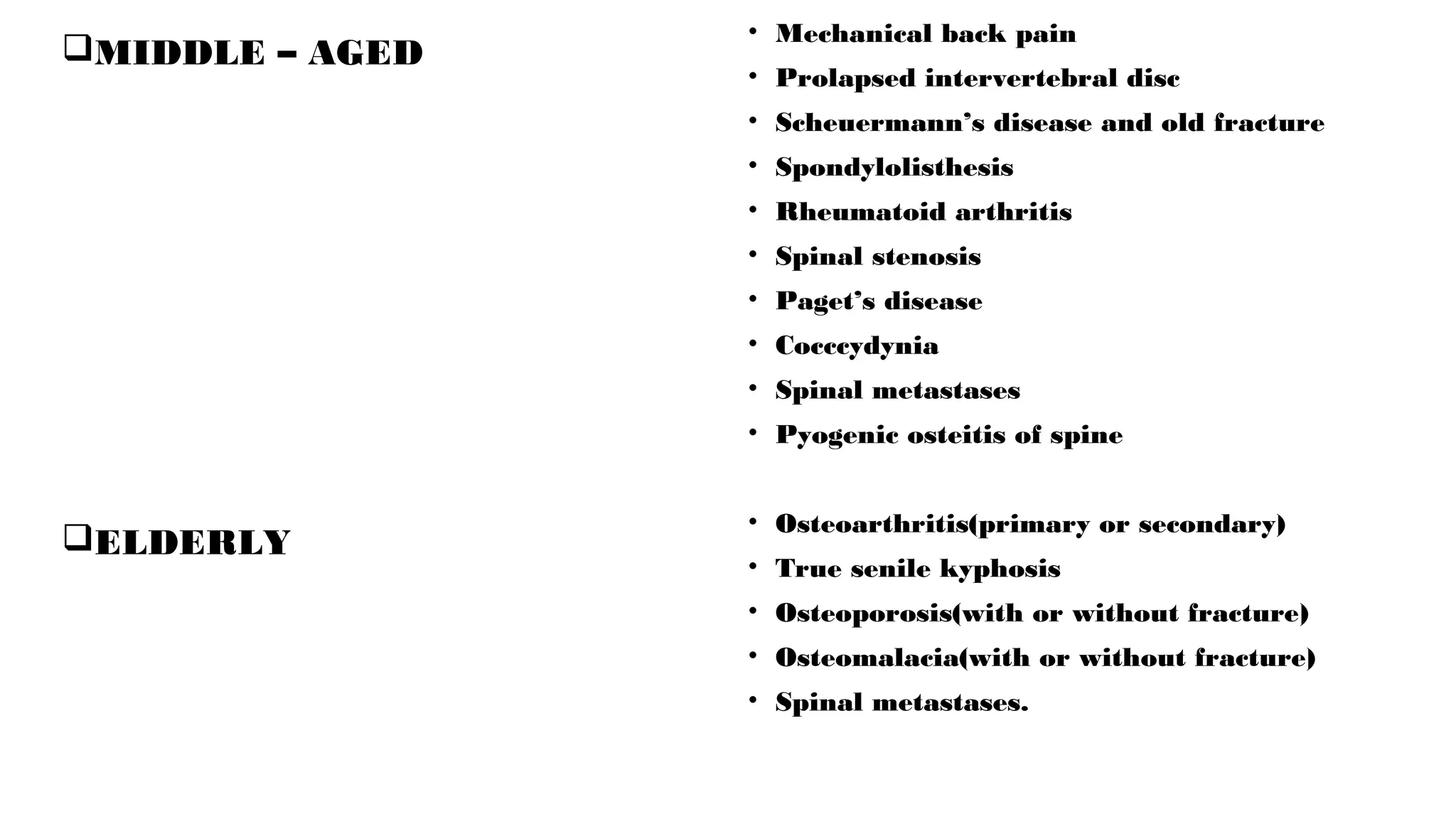
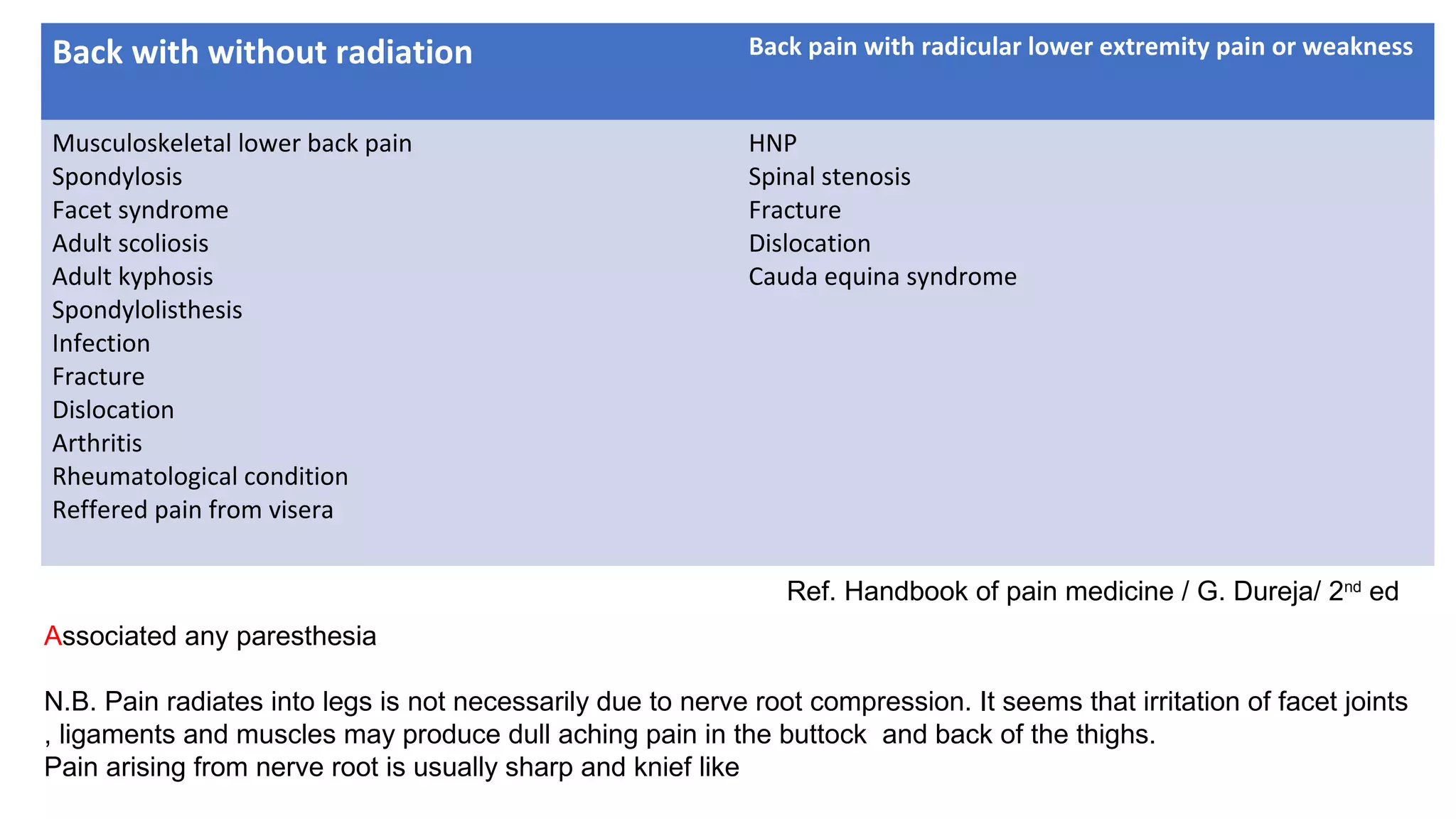
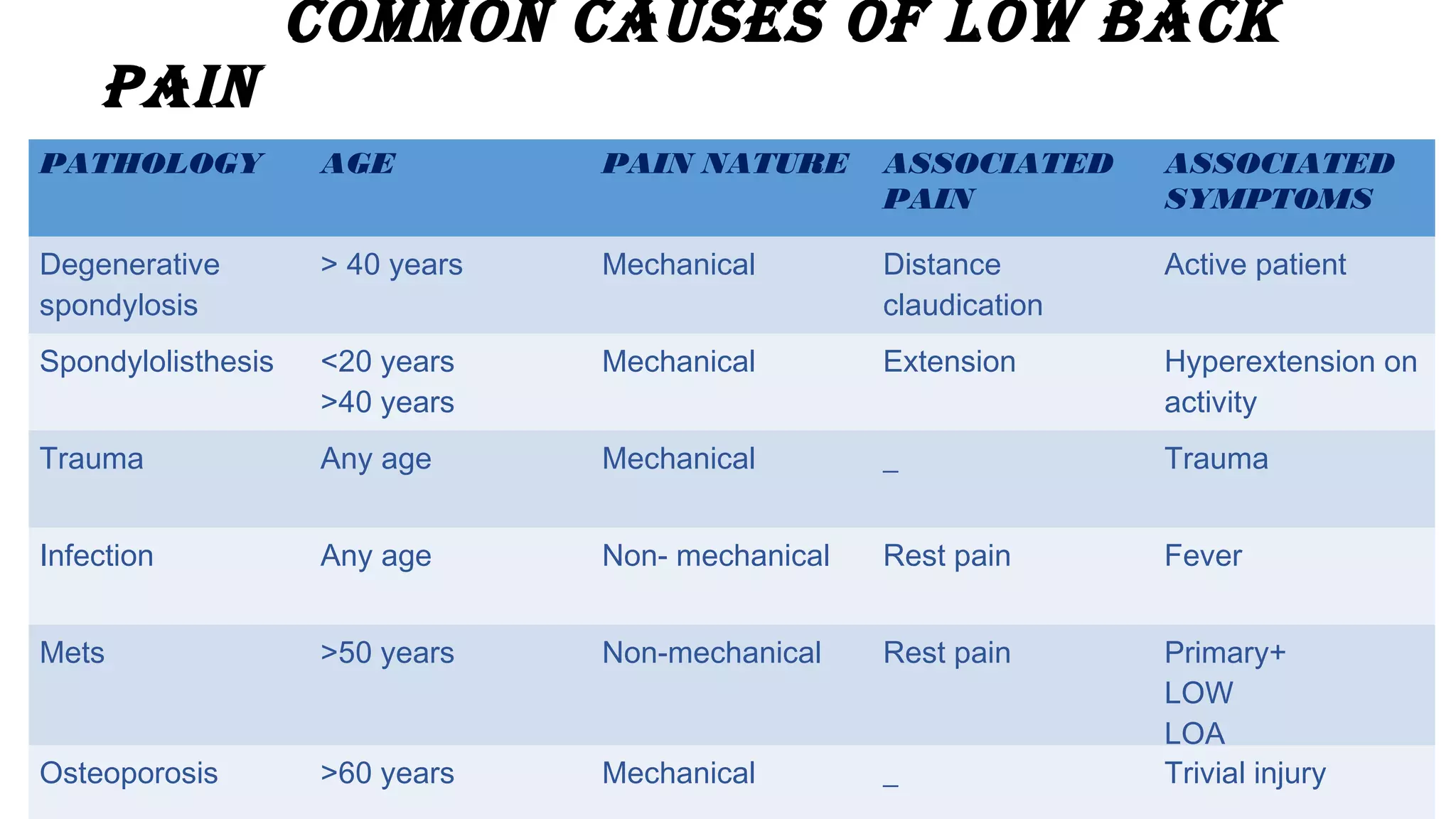
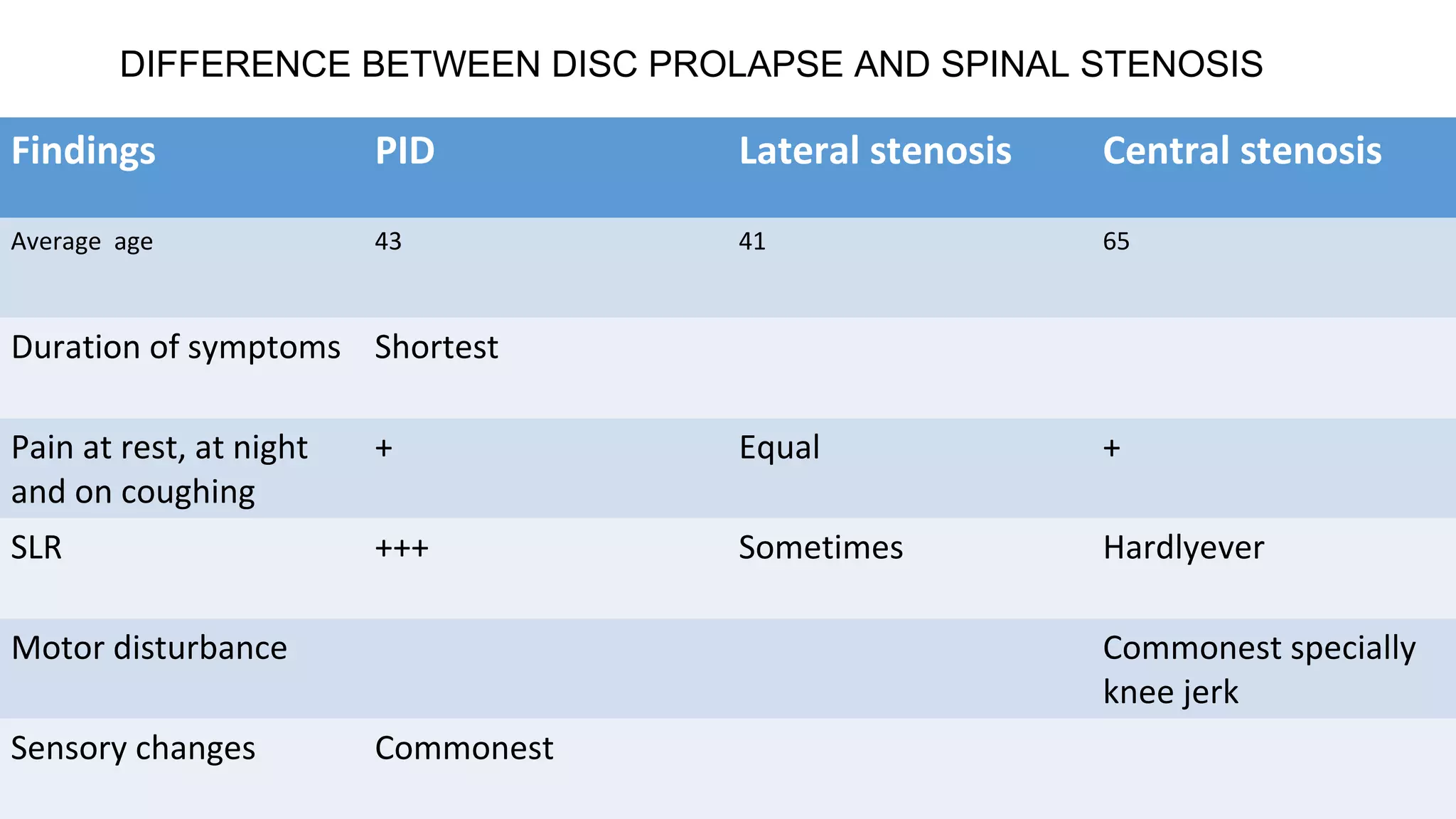
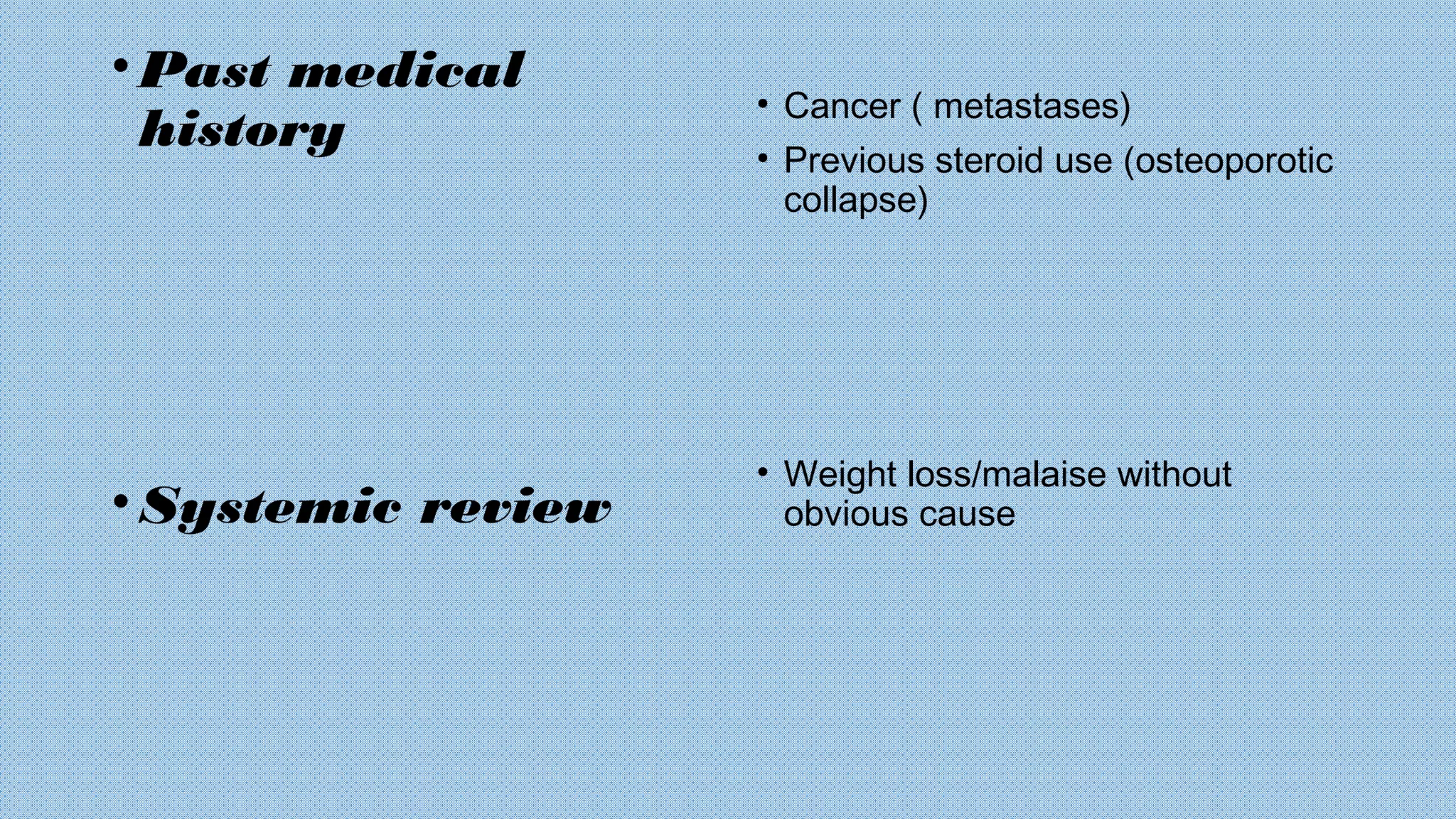
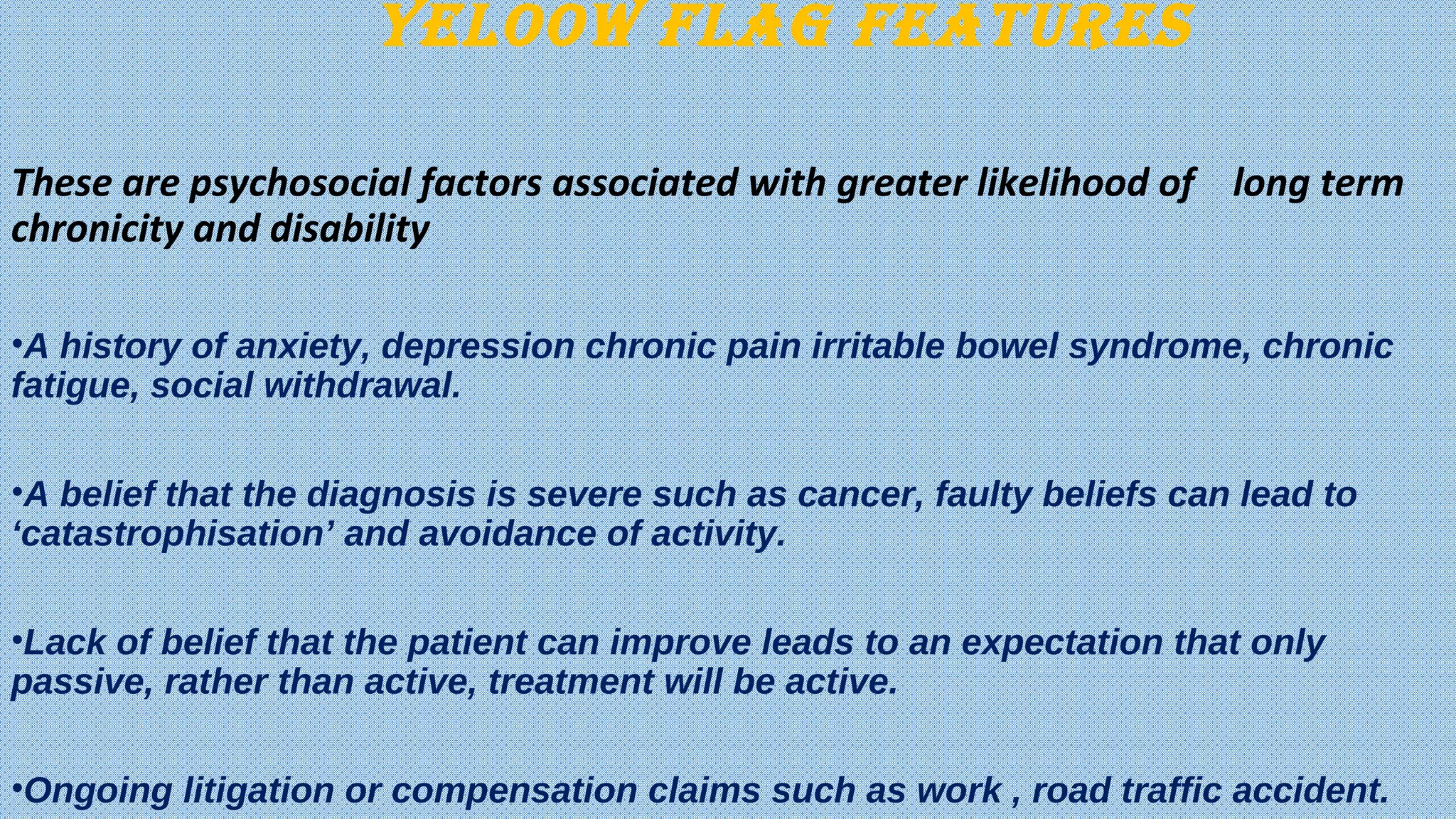
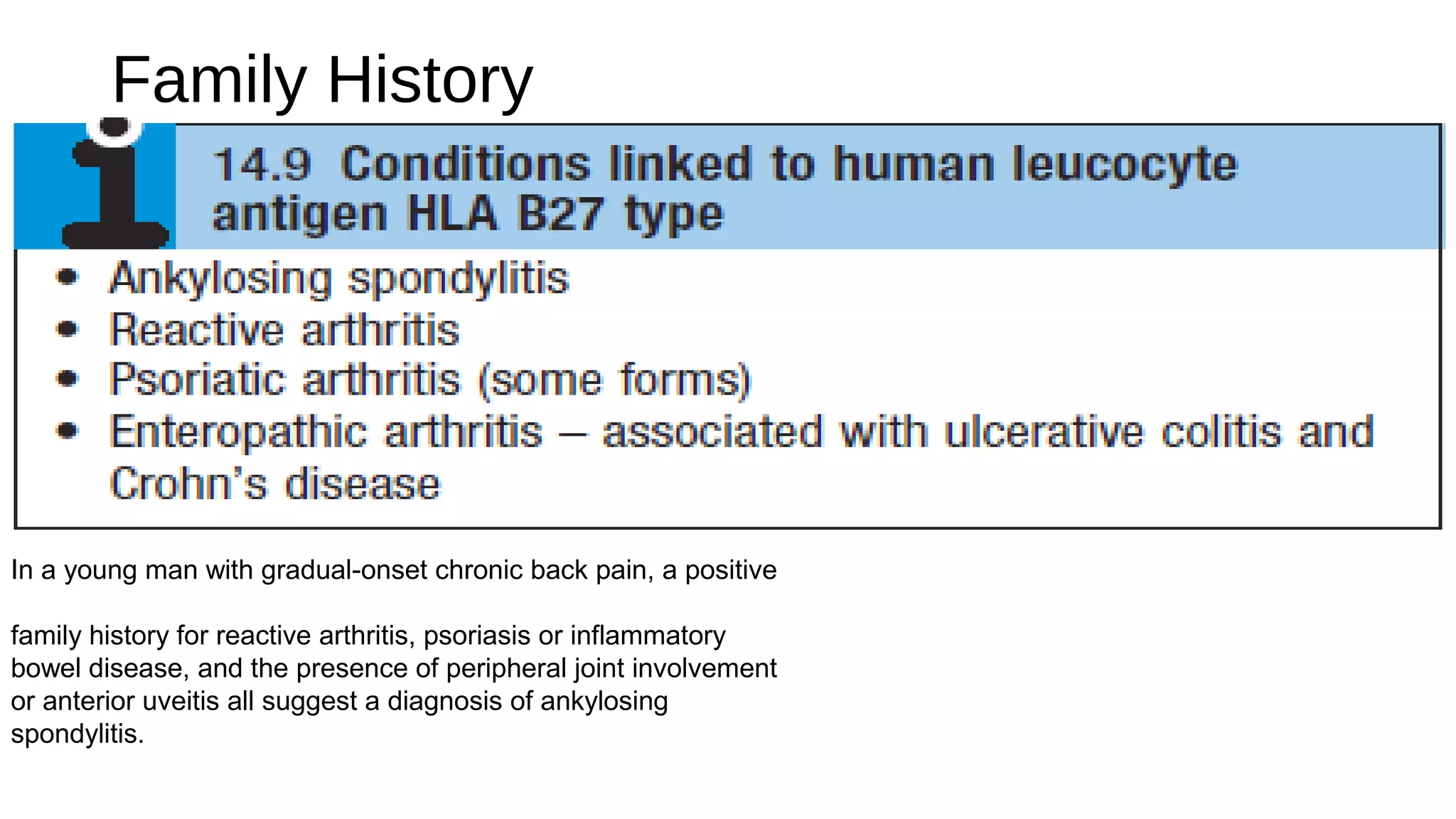
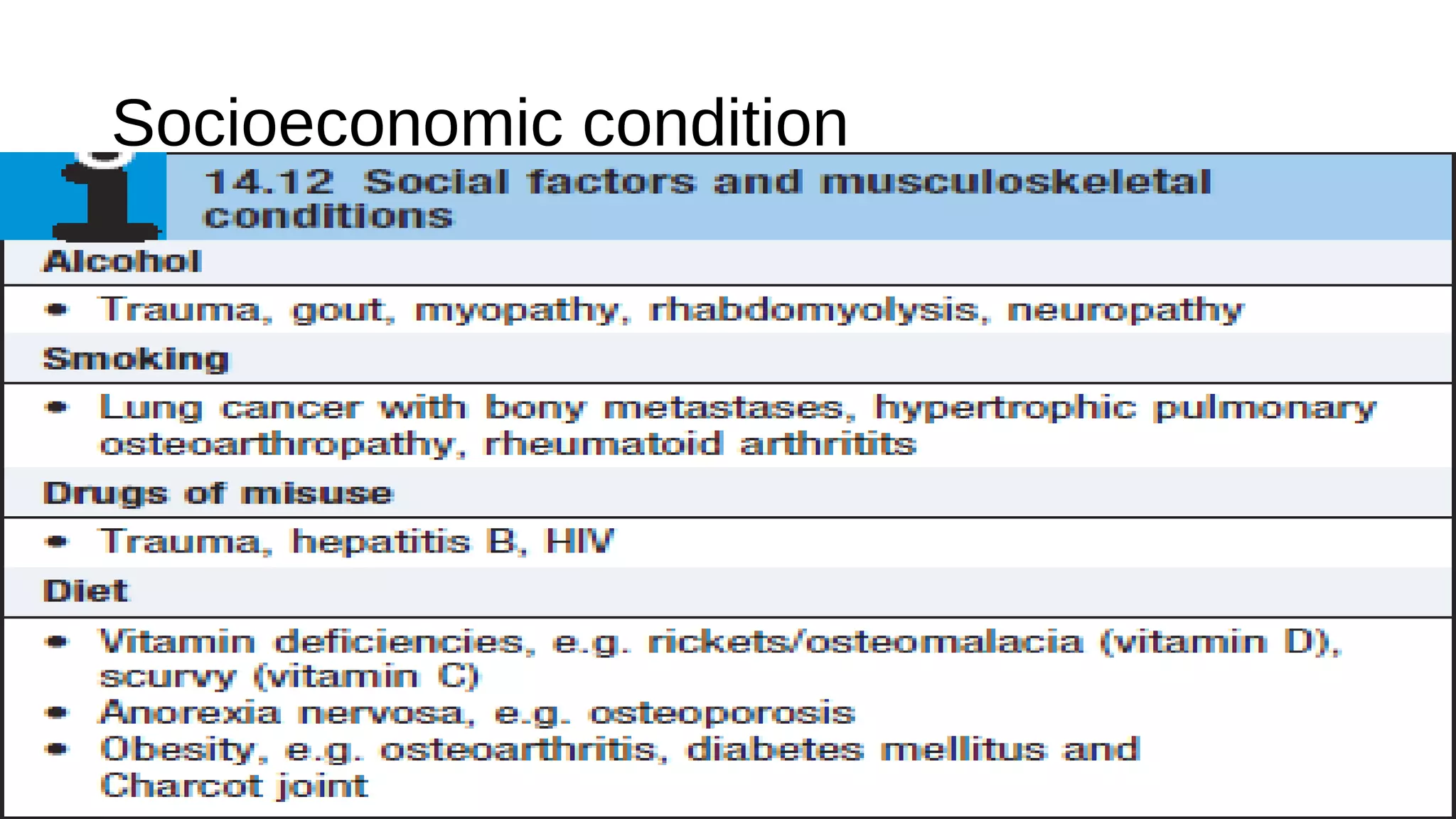
This document discusses the common causes and clinical presentation of low back pain in different age groups. It outlines various pathologies that can cause low back pain such as degenerative spondylosis, spondylolisthesis, trauma, infection, and metastases. The document differentiates between disc prolapse and spinal stenosis. It identifies red flag features that suggest a serious underlying condition and yellow flag psychosocial factors associated with chronic pain. Clinical assessment of low back pain includes history of present illness, review of systems, physical examination, and consideration of psychosocial factors.