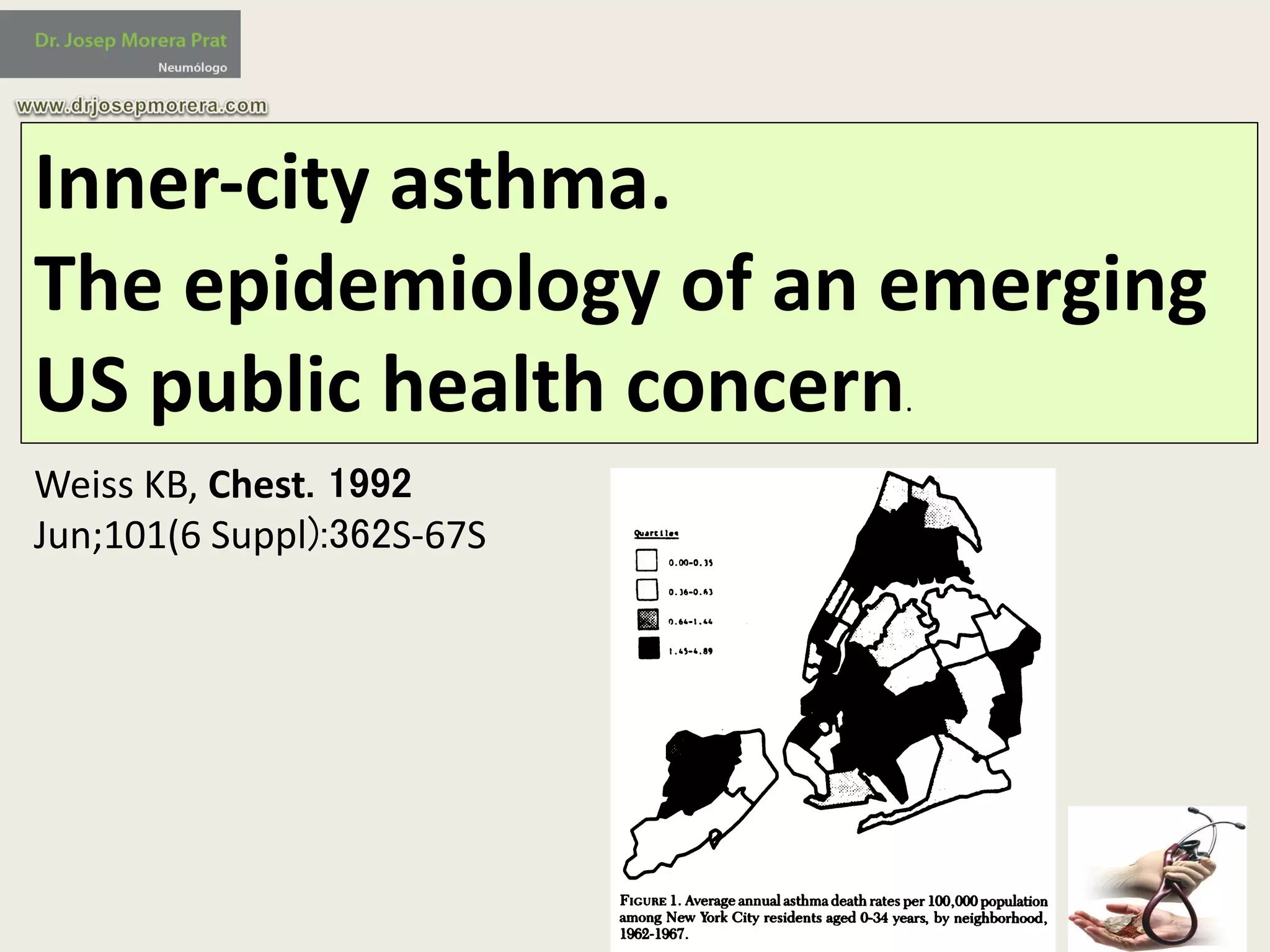
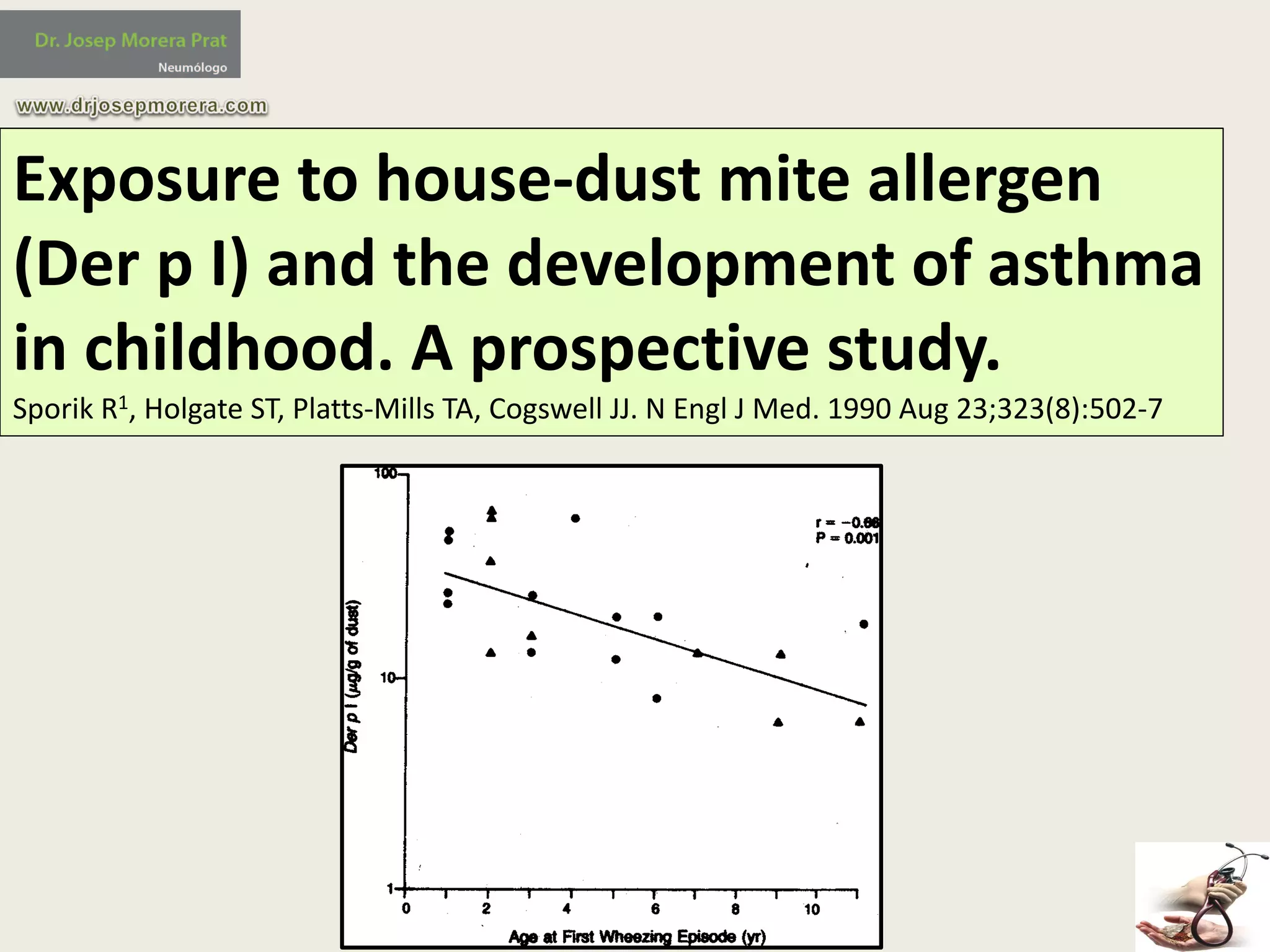
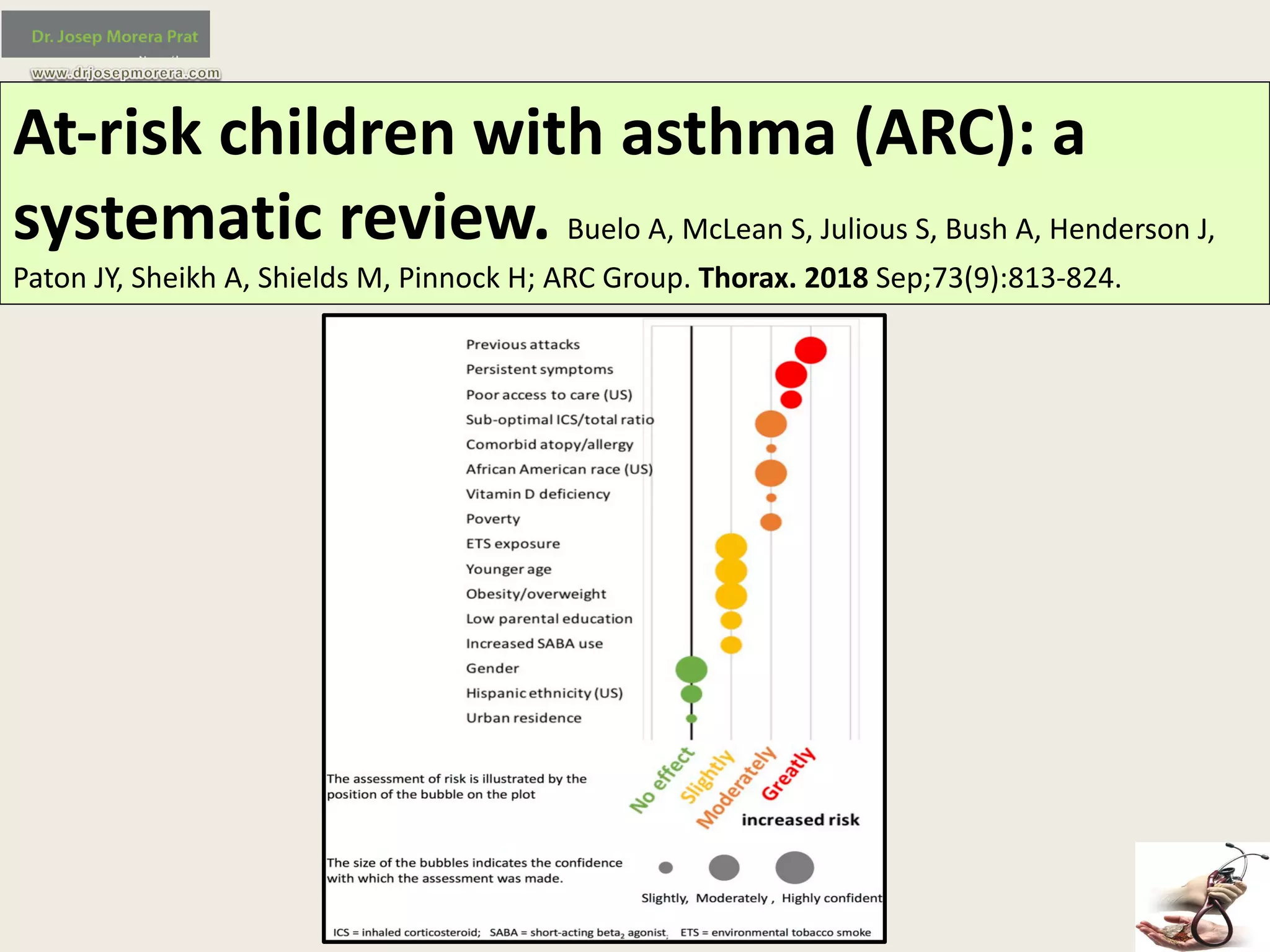
The document provides an overview of the 'hygiene hypothesis' and its implications regarding allergic diseases such as asthma and hay fever, suggesting that declining family size and improved hygiene may contribute to increased prevalence of these conditions. However, it concludes that the hypothesis does not sufficiently explain the rise in asthma and emphasizes that asthma is multifactorial, influenced by genetic, epigenetic, and environmental factors. Additionally, it highlights the importance of considering inner-city asthma, viral infections, and certain lifestyle practices that may affect allergy development.