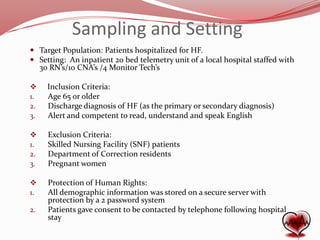
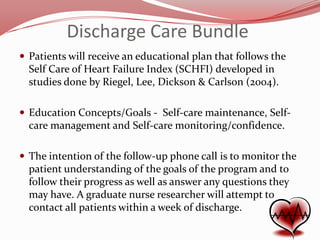
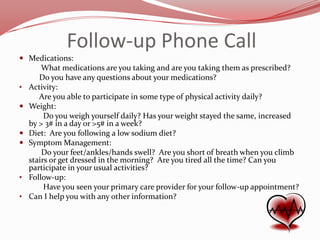
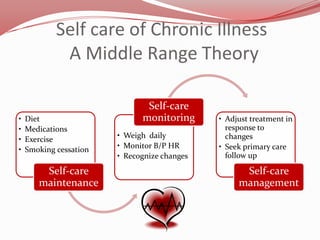
This study aims to determine if a nurse-delivered discharge planning bundle that includes a follow-up phone call within 1 week of discharge will decrease rapid readmissions of patients with heart failure. The researchers will implement a discharge care bundle including patient education and a follow-up phone call on a hospital unit. They will compare rates of readmission before and after the intervention to see if the bundle reduces readmissions. The goal is to improve patient outcomes and lower healthcare costs for heart failure patients.