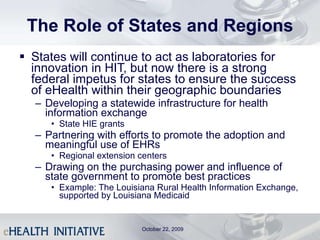
The document discusses a survey conducted by eHealth Initiative on regional extension centers and meaningful use of electronic health records. Key findings from the survey include:
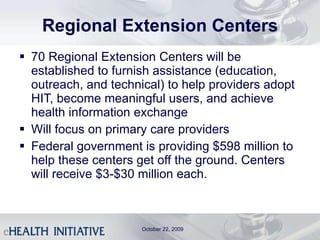
- Regional extension centers should be flexible and not constrained by state or regional boundaries in order to best meet local needs. There should be 10-100 centers.
- Quality improvement organizations are best suited to run the extension centers based on their experience.
- Extension centers should focus on disseminating best practices, providing technical assistance to clinicians, and assisting primary care practices and those in rural/underserved areas.

![Thank You! Robert D. Marotta, Esq. Senior Vice-President and Chief Regulatory Counsel, HLTH/WebMD Health Corp. President, eHealth Foundation [email_address] (614) 462-5435 October 1, 2009](https://image.slidesharecdn.com/hitfinal-091104154346-phpapp01/85/2009-Kegler-Brown-HIT-Seminar-16-320.jpg)


![Thank You! Jennifer Covich Bordenick [email_address] 202-624-3288 www.eHealthInitiative.org Don’t Miss eHI’s Annual Conference in Washington, DC on January 25 th and 26 th ! October 22, 2009](https://image.slidesharecdn.com/hitfinal-091104154346-phpapp01/85/2009-Kegler-Brown-HIT-Seminar-57-320.jpg)











![Thank You! Élise Spriggs Director, Kegler Brown [email_address] (614) 462-5451](https://image.slidesharecdn.com/hitfinal-091104154346-phpapp01/85/2009-Kegler-Brown-HIT-Seminar-88-320.jpg)





![Thank You! Jeff Porter Director, Kegler Brown [email_address] (614) 462-5418](https://image.slidesharecdn.com/hitfinal-091104154346-phpapp01/85/2009-Kegler-Brown-HIT-Seminar-131-320.jpg)