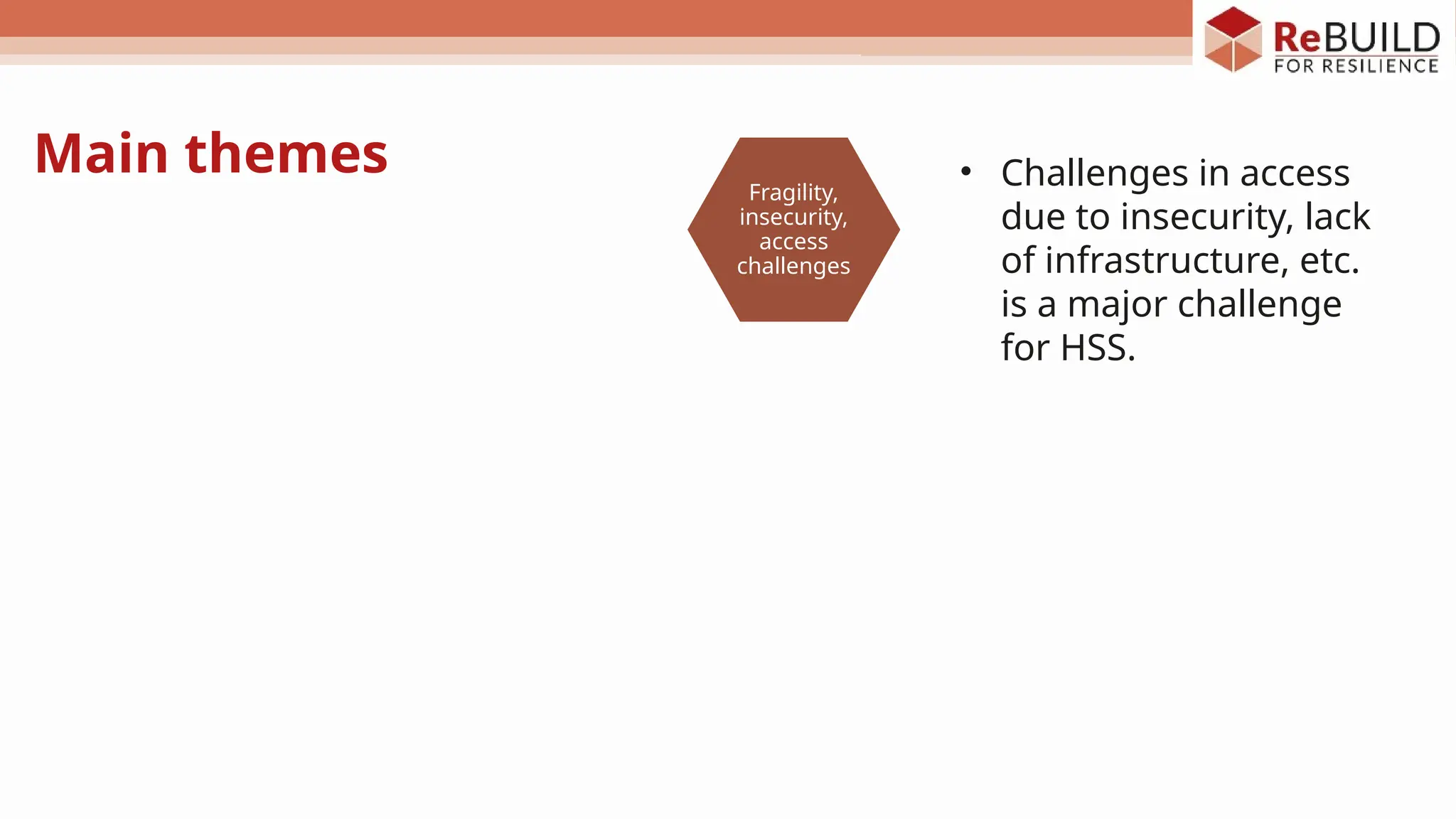
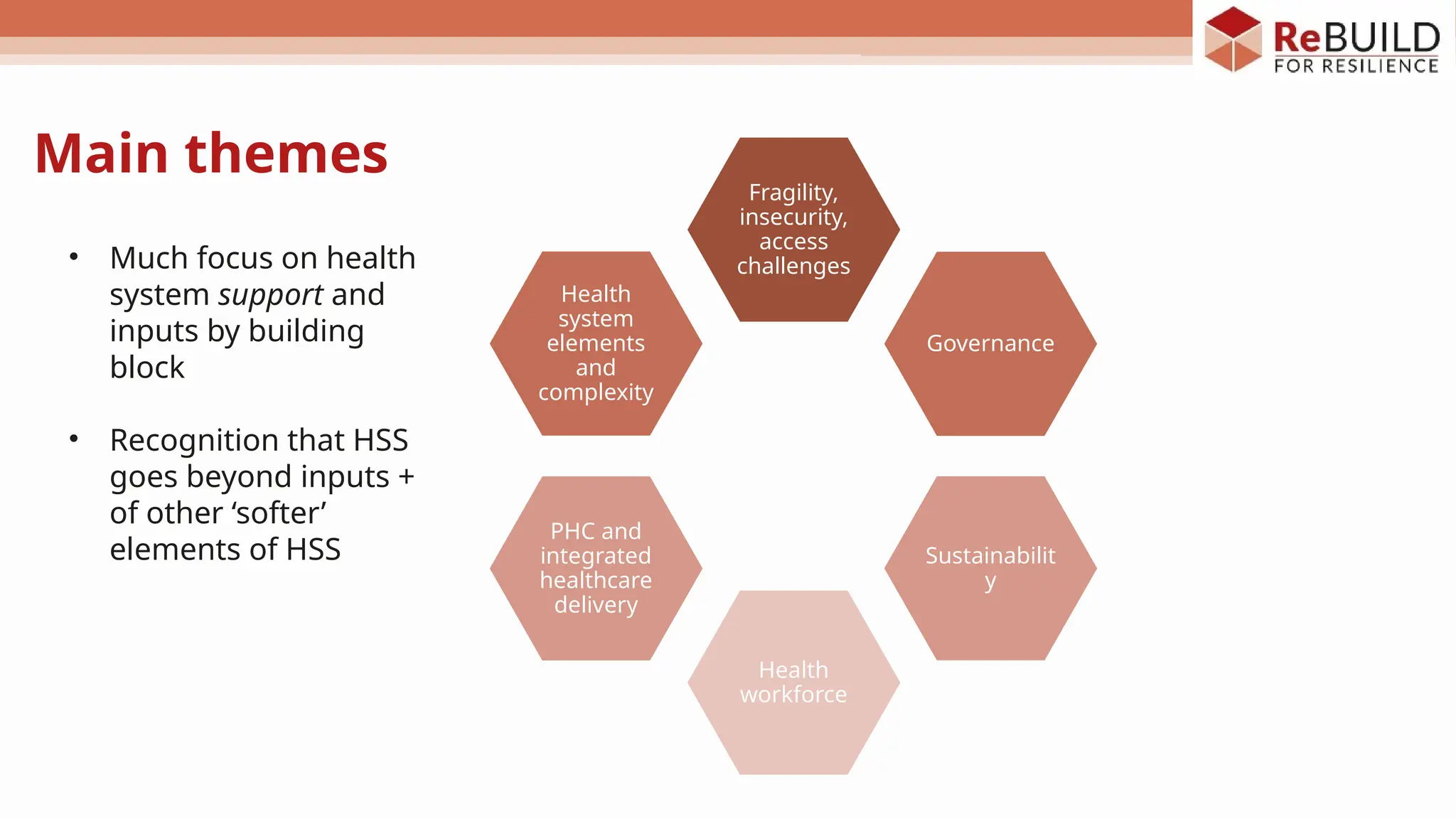
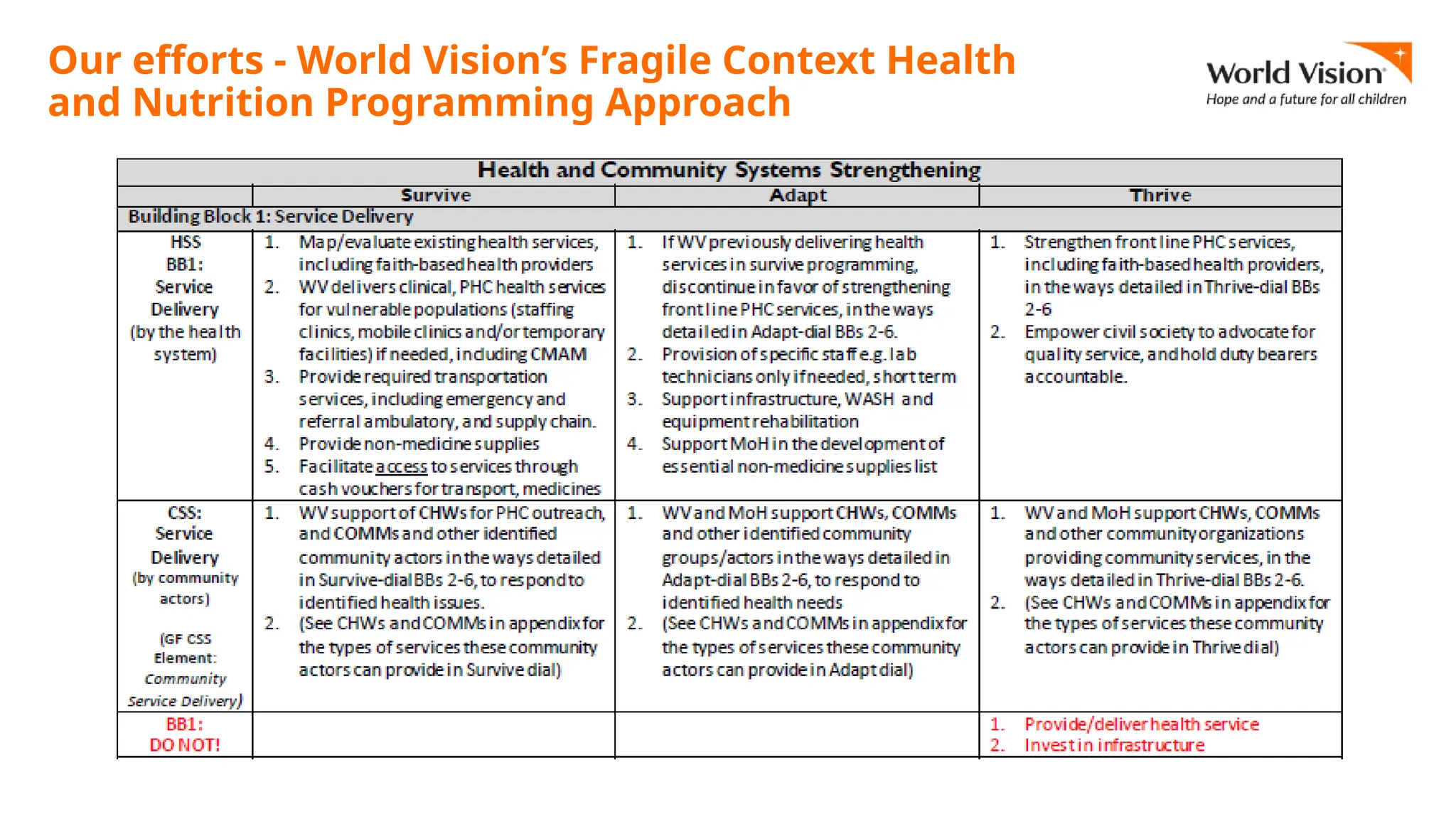
The document discusses health systems strengthening (HSS) in fragile and conflict-affected settings (FCAS), highlighting the operational experiences and challenges faced by NGOs in these contexts. It synthesizes findings from key informant interviews, emphasizing the need for flexibility, better governance, and integration between humanitarian and development efforts. The session aims to foster discussion on promoting effective HSS programming in FCAS while addressing critical gaps and challenges.









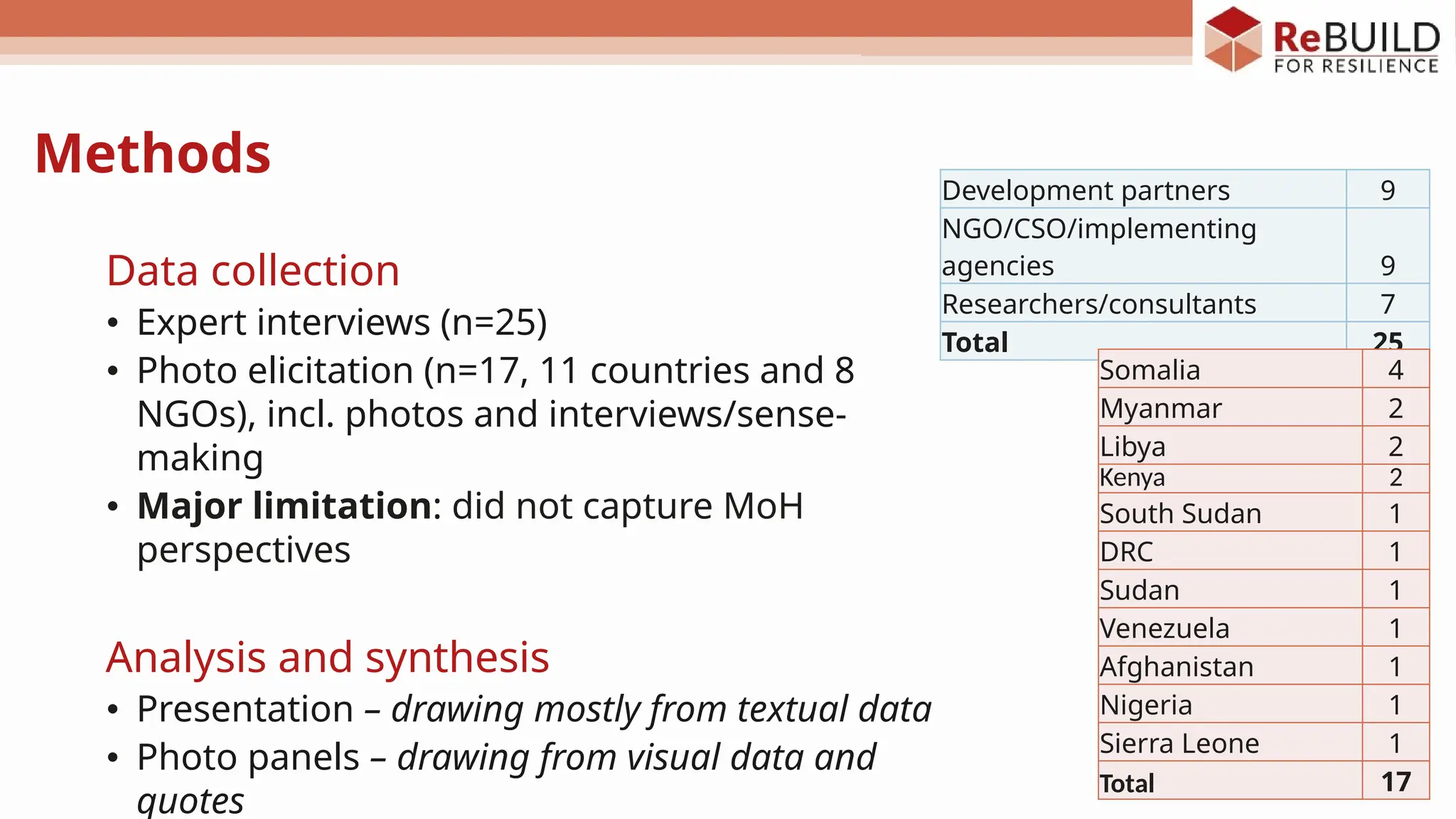

![• Potential to leverage the
humanitarian phase for HSS
• In some cases, crisis can even
provide windows for reforms / HSS:
▫ COVID-19
▫ Ukraine
▫ Vulnerabilities are more visible
“We need to have a clear understanding of what is
possible in each setting. We have to be realistic
about what is possible in terms of HSS. It is very
contextualised” (KII).
“It is important not to overestimate the priority of
HSS in humanitarian contexts, where the priority is
saving lives. Humanitarian actors are happy to use
existing systems where possible, but gaps are
sometimes too big. NGOs need to deliver, so having
to hire externally or bringing their own systems
might be needed” (KII).
• Priority is saving lives
• Focus on service delivery and
health system support at most “Emergencies are cyclical in a setting like eastern
DRC. We need to be able to capitalise on the
emergency response for HSS” (KII)
“Humanitarian actors are not mandated to do HSS
but [should] at least “do no harm”” (KII)
Fragility, insecurity, humanitarian priorities](https://image.slidesharecdn.com/hssinfcassatellitesession-241203134319-148643d5/75/Health-System-Strengthening-in-Fragile-Conflict-Affected-Settings-19-2048.jpg)

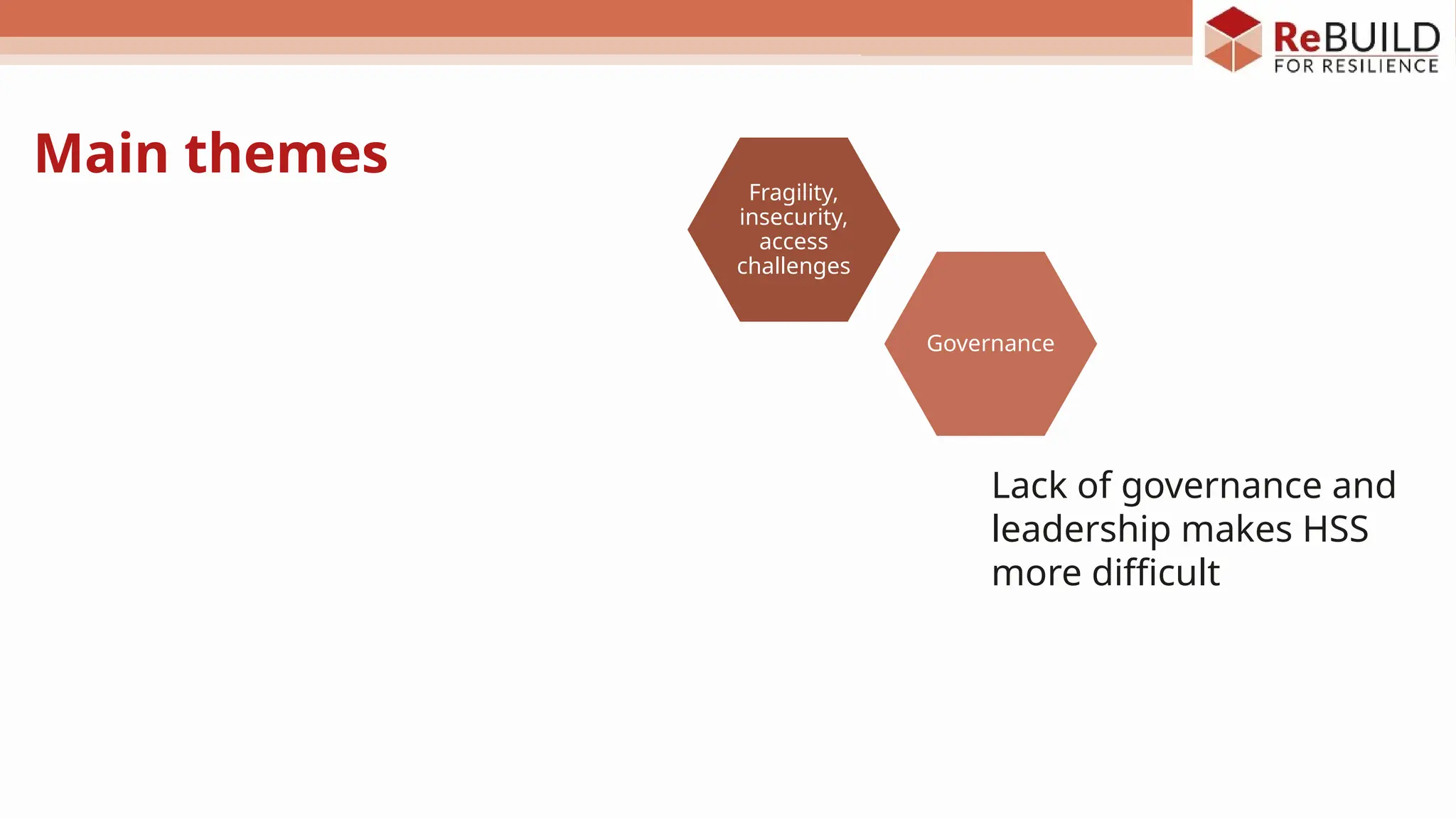
![Governance
• Lack of political peace and weak
governance and leadership make HSS
more difficult.
▫ Governments are weak, absent or multiple,
not legitimate (internally or externally), etc.
• HSS somewhat assumes the existence of a
single, national government and a public
health system as a precondition, what can
be done without it?
• Even more fundamentally, if there is no
government leadership/stewardship, how
can local ownership be fostered which
would make interventions sustainable?
“We are trying to build capacity at all
levels in case the transition [to
Government ownership] has to happen,
but the Somali government is very
politically fragmented, for any
activities there is the need for a lot of
negotiations, to sit with them at
different levels and multiple times, to
bring all to the table”. Photo elicitation:
NGO, Somalia](https://image.slidesharecdn.com/hssinfcassatellitesession-241203134319-148643d5/75/Health-System-Strengthening-in-Fragile-Conflict-Affected-Settings-21-2048.jpg)





![• NGOs are not better placed for HSS and
taking the “strategic view”
• They needs supportive structures and a
clear set of incentives from funders to be
able to facilitate/do HSS
• There is also need for more understanding
and capacity building around HSS
▫ Varying definitions and level of
conceptual reflections
▫ Also reflecting mandates and funding
sources (e.g. humanitarian or GHI
funding)
Role of NGOs
“NGOs have more competence in service delivery and
less in working across the building blocks. Is [HSS]
really their role? They can’t work if [governance]
structures are not well set up. But at the same time, is it
their role to do it [set up governance structures]?” (KII).
“We can’t expect NGOs to be strategic at such high level
(...). But they can be involved in the discussions to
ensure empowerment, allow them to contribute to the
debate and share their learnings, ask donors to set the
right incentives for NGOs” (KII).
“Donors should allow, NGOs should do” (KII).](https://image.slidesharecdn.com/hssinfcassatellitesession-241203134319-148643d5/75/Health-System-Strengthening-in-Fragile-Conflict-Affected-Settings-29-2048.jpg)