Vidushi Sharma presented on bone repair and joint replacement techniques. Key points include:
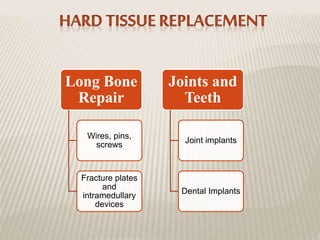
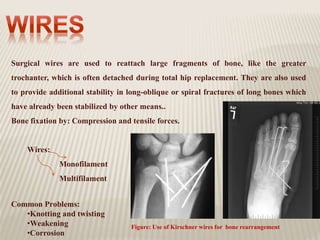
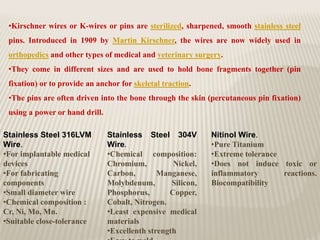
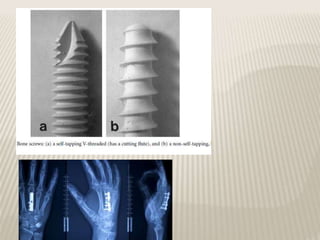
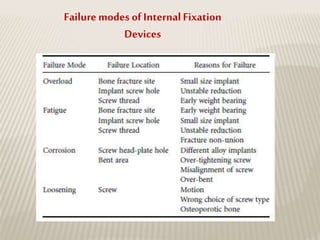
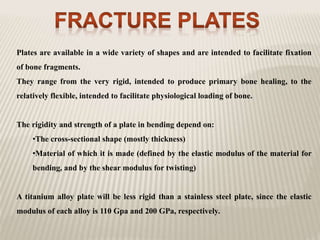
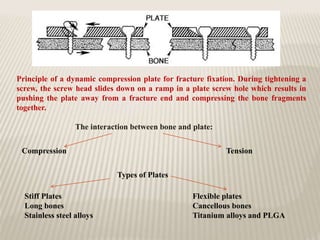
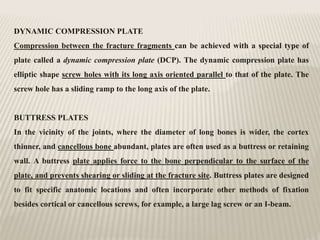
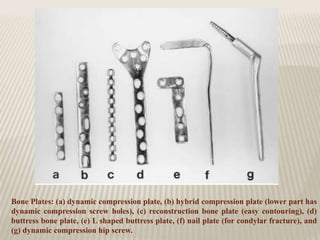
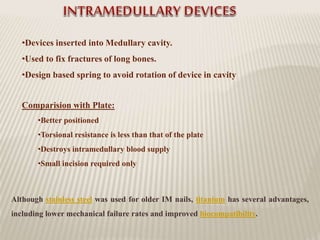
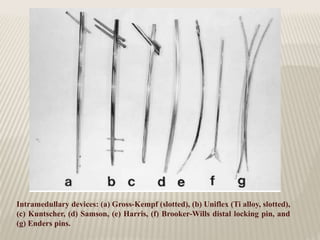
1) Bone has the ability to regenerate through a balance of bone formation and resorption processes. Various surgical techniques like plates, screws, and intramedullary devices are used to stabilize fractures during healing.
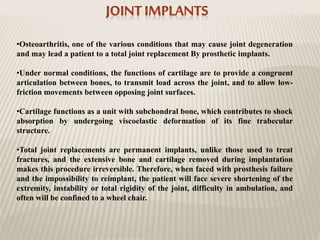
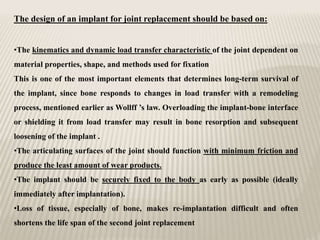
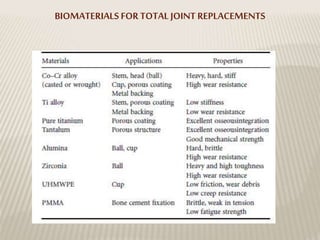
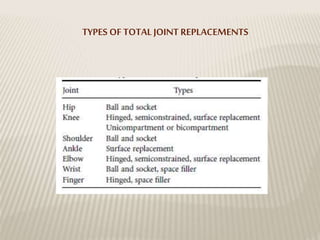
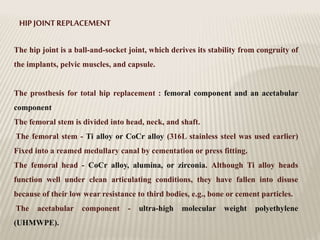
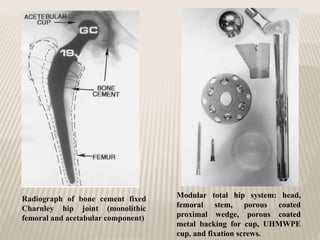
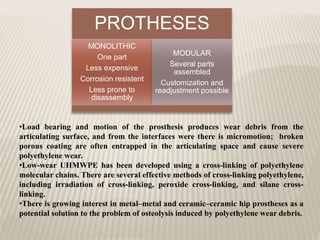
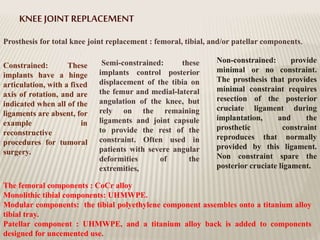
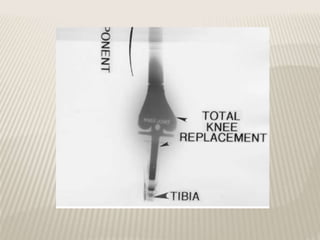
2) Joint replacements are used to treat joint degeneration and involve removing bone and cartilage to implant prosthetics. Implant design considers load transfer and articulation to minimize wear and promote fixation.
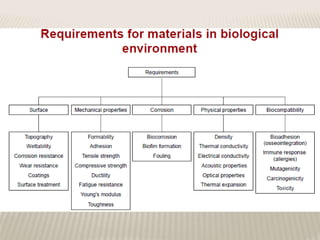
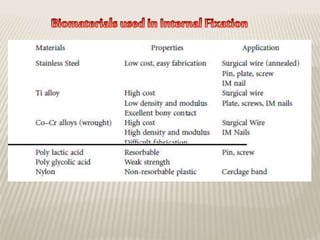
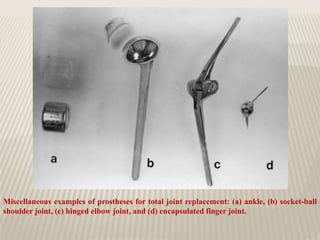
3) Common techniques were discussed, including dynamic compression plates, intramedullary nails, and total hip replacements using ball-and-socket implants. Biocompatible materials like stainless steel and titanium