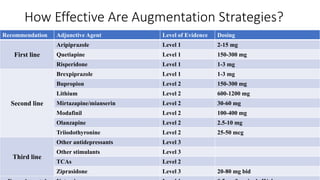
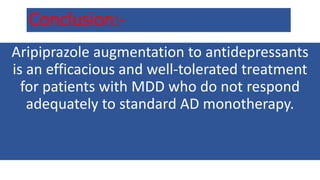
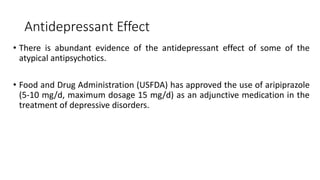
This document discusses the use of aripiprazole as an adjunctive treatment for major depressive disorder.
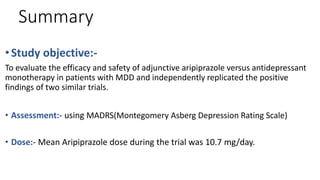
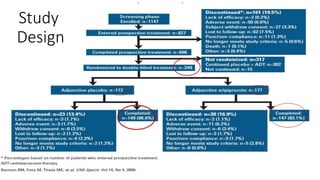
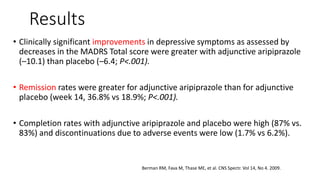
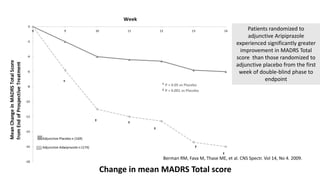
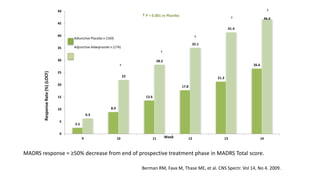
1) A study found that adjunctive aripiprazole resulted in significantly greater improvement in depressive symptoms compared to placebo, as measured by the MADRS scale. Remission rates were also higher with aripiprazole.
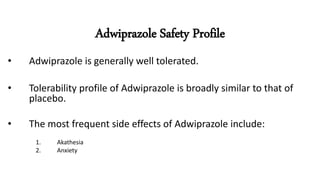
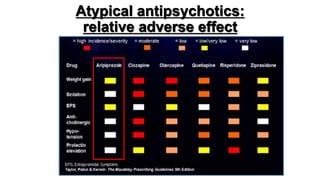
2) Adjunctive aripiprazole was well tolerated with completion rates similar to placebo and lower discontinuation due to adverse events.
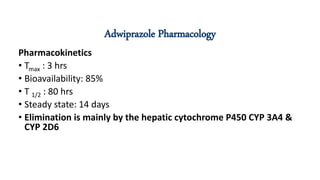
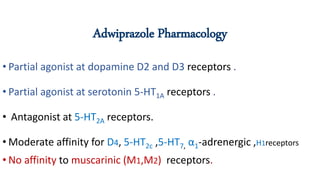
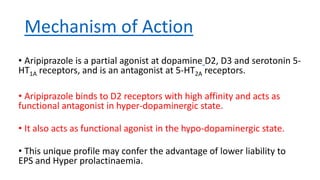
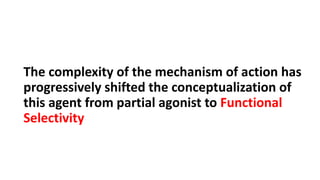
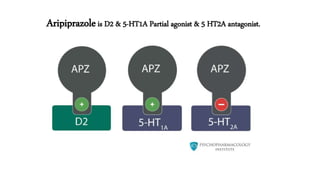
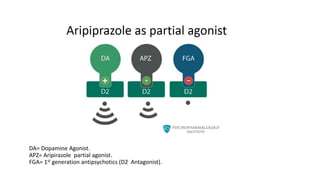
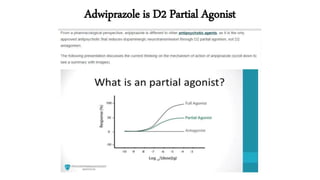
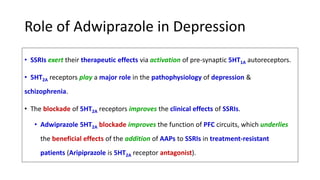
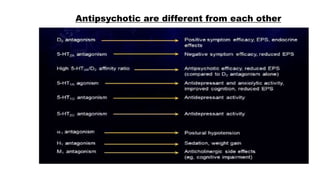
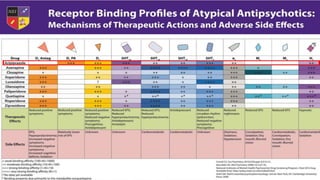
3) Aripiprazole's mechanism of action as a partial agonist at dopamine and serotonin receptors provides a unique pharmacological profile that may improve outcomes for patients with treatment resistant depression when used as an adjunct




![Guidelines
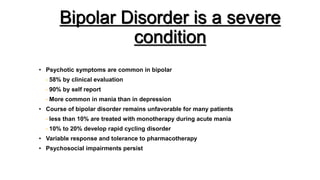
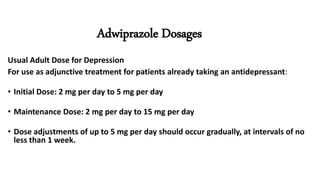
According to the 2016 FDA Medication Guide (FDA
Medication Guide [PDF], 2016). ARIPIPRAZOLE is used to
treat:
• Schizophrenia
• Bipolar I disorder with mania or mixed episodes
• Major depressive disorder (MDD) when used with antidepressant
medicines
• Irritability associated with autistic disorder
• Tourette’s disorder](https://image.slidesharecdn.com/hanipsycharipiprazoleasantidepressant-190919002359/85/Hanipsych-aripiprazole-as-antidepressant-46-320.jpg)
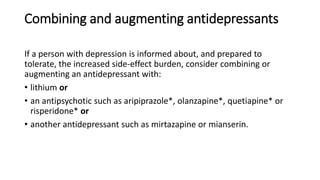
![• Second-generation antipsychotic – In choosing a second-generation
antipsychotic as augmentation for treatment resistant depression, our
general order of preference is as follows, based upon the evidence of
benefits and harms, as well as formulary
availability: aripiprazole or brexpiprazole, quetiapine, risperidone, and
more rarely, ziprasidone or olanzapine [30,34,39,41-43].](https://image.slidesharecdn.com/hanipsycharipiprazoleasantidepressant-190919002359/85/Hanipsych-aripiprazole-as-antidepressant-49-320.jpg)